Abstract
Objective
To characterize SUDEP discussion practices of child neurologists approximately 6 and 12 months after publication of the American Academy of Neurology SUDEP Clinical Practice Guideline and explore factors associated with discussion practice.
Methods
Child Neurology Society members (~2450) were electronically surveyed in November 2017 and May 2018 regarding their practice of discussing SUDEP with patients with epilepsy or their caregivers. Multivariable proportional odds ordinal logistic regression evaluated factors associated with discussing SUDEP with a greater proportion of epilepsy patients/caregivers. Reasons for changing practice were described.
Results
Among the 369 child neurologist respondents, 36% reported discussing SUDEP with at least half of their epilepsy patients/caregivers including 12% who discuss with all or almost all (>90%) of their epilepsy patients/families. Those who discussed SUDEP with an increased proportion of their patients were more likely to agree that they knew enough to talk about SUDEP, agree that healthcare providers have an ethical obligation to discuss SUDEP, and disagree that there is not enough time to talk about SUDEP. Those who agreed SUDEP could provoke excessive anxiety or worry were less likely to discuss SUDEP with an increased proportion of their patients. Reading the SUDEP Clinical Practice Guideline was a frequently cited reason among respondents who reported a recent change in discussion practice.
Significance
Most child neurologists do not follow the current SUDEP Clinical Practice Guideline regarding SUDEP discussion. Feeling sufficiently knowledgeable and ethically obligated to discuss SUDEP were associated with increased discussion practice, suggesting an educational intervention may be effective at increasing SUDEP discussion rates.
Keywords: epilepsy, medical ethics, pediatrics, seizures, sudden death
Key Points.
Most child neurologists do not follow the current SUDEP Clinical Practice Guideline regarding SUDEP discussion
36% of child neurologists discuss with at least half of patients with epilepsy or their families; 12% discuss with >90% of patients
Those agreeing SUDEP could provoke excessive worry were less likely to discuss SUDEP with an increased proportion of their patients
Feeling sufficiently knowledgeable and ethically obligated to discuss SUDEP were associated with increased discussion
1. BACKGROUND
SUDEP is the sudden unexpected death of an individual with epilepsy, when no cause of death can be found on autopsy. A meta‐analysis of the incidence of SUDEP in children reported approximately 1 in 4500 children with epilepsy die of SUDEP annually, though more recent work suggests that the incidence of pediatric SUDEP is approximately 1 in 1000 per year. 1 , 2 , 3 The mechanism(s) of SUDEP are not well understood, and the most robustly identified risk factor is the frequency of generalized tonic‐clonic seizures. 1 Recommended prevention strategies relate to controlling seizures with some limited evidence toward nocturnal monitoring or supervision. 1
Historically, most healthcare providers have not routinely discussed the risk of SUDEP with patients with epilepsy or their caregivers 4 , 5 , 6 , 7 despite ample evidence indicating patients and caregivers want to know. 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 Child neurologists’ reported reasons for not discussing SUDEP center on the perceived minimal benefit to discussion with the potential for worsening quality of life or mood. 4 , 7
In April 2017, the American Academy of Neurology (AAN) and American Epilepsy Society (AES) jointly published a Clinical Practice Guideline stating physicians should discuss the risk of SUDEP with people with epilepsy or their caregivers. The effect of this Guideline on discussion practices of child neurologists is unknown. Here, we report child neurologists’ current SUDEP discussion practices with children with epilepsy or their caregivers and explore the factors associated with SUDEP discussion and reasons for change in practice.
2. METHODS
2.1. Data collection
Members of the Child Neurology Society were invited to participate in two online surveys distributed via email in November 2017 and May 2018. Respondents were eligible if they reported being healthcare providers devoting at least 5% of their time to clinical care and treating at least one patient for epilepsy in the past 6 months. Two email reminders were sent during the one‐month period that each survey was open for participation. Both surveys were anonymous: respondent names, email addresses, or other identifying information was not collected.
Data collected in the November 2017 survey included questions regarding demographics, the proportion of patients with epilepsy or their families with whom they discuss SUDEP, experience with losing patient(s) to SUDEP, knowledge of SUDEP (incidence, risk factors), and familiarity with the AAN/AES SUDEP Clinical Practice Guideline. To assess opinions and attitudes regarding SUDEP discussion, respondents were asked to indicate their agreement or disagreement using a 5‐point Likert scale on 10 statements about SUDEP and SUDEP discussion. An optional 10‐minute educational video detailing SUDEP incidence, risk factors, the medical ethics of SUDEP discussion, and strategies for discussion was included at the end of the first survey. Respondents were queried as to whether they watched the video to completion.
Data collected in the second survey in May 2018 included the same questions regarding practice of discussing SUDEP with patients or their families, opinions/attitudes about SUDEP discussion, knowledge of SUDEP, and familiarity with AAN/AES SUDEP Guideline. Additional questions included whether child neurologists had changed their discussion practice in the previous 6 months, how practice was changed, and reasons for the change.
The primary outcome of interest—characterizing the current SUDEP discussion practice of child neurologists—was operationalized by querying “Approximately, what proportion of your patients with epilepsy or their families do you talk to about the increased risk of sudden death (SUDEP)?”. Response options included “All or almost all (>90%),” “Most (50%–90%),” “Some (10%–49%),” “Few (1%–9%),” or “None (0%).” All survey questions are included in the supplemental materials.
2.2. Analysis
Respondents self‐identifying as child neurologists or as pediatricians with advanced training in epilepsy were included in this analysis. Current residents and fellows were not included. Incomplete surveys, defined as those who did not report the proportion of epilepsy patients/families with whom they discuss SUDEP, were also excluded.
Data from the two surveys was linked to distinguish individuals who participated in both surveys. Study data were anonymous, so responses were linked or identified as unique using a code derived from nonidentifiable personal information (ie last 4 digits of cell phone number, first letter of mother's maiden name, first letter of respondent's last name, and day of the month of birth). If two or more surveys had the same code, for example if a respondent completed the survey twice, only the first response was included.
After linking, it was noted that there was insufficient subjects completing the survey at both time points, rendering the original study objective of evaluating for an association between watching the SUDEP educational video and subsequent change in discussion practice infeasible. Consequently, the analysis plan was redesigned to analyze the factors associated with child neurologists’ SUDEP discussion practice and self‐reported reasons for changing it.
To characterize respondents’ SUDEP discussion practices and assess factors associated with SUDEP discussion, the November 2017 and May 2018 respondents were merged. For subjects who completed surveys at both timepoints, information regarding the demographics, SUDEP discussion practice, and attitudes about SUDEP were taken from the first timepoint. Distributions of the approximate number of patients treated for epilepsy in the past 6 months and proportions of families/patients with whom respondents discuss SUDEP were visually compared across survey groups.
Proportional odds ordinal logistic regression was used to model factors associated with SUDEP discussion practice. Predictors of interest included the 10 questions assessing child neurologists’ opinions and attitudes regarding SUDEP and SUDEP discussion. To address risk of overfitting and multicollinearity of the predictors, potential explanatory variables were correlated with each other. Where Spearman correlations between potential predictors >0.35 were observed, the potential predictors were correlated with SUDEP discussion practice and the potential predictor with stronger correlation was retained. In the proportional odds ordinal logistic regression model, “strongly disagree”/ “disagree” and “strongly agree”/ “agree” categories in the explanatory variables were merged. Similarly, as very few child neurologists reported discussing SUDEP with none of their patients, “None (0%)” and “Few (1%–9%)” categories were merged. Responses with missing data were assumed to neither agree nor disagree. The proportional hazards assumption was investigated for each predictor by evaluating a proportional odds model against a multinomial logistic regression model.
Additional details of child neurologists’ experiences relating to the factors identified as significant from the multivariable model were summarized. Relationship of the factors with respect to change in SUDEP discussion practice on the May 2018 survey was examined. Missing data were excluded from these exploratory analyses. Data were summarized by frequency and percent and compared between groups using chi‐square tests or Fisher's exact test where expected cell counts <5. Comparisons including variables measured with a five‐point Likert scale were condensed into 3 categories by combining the “strongly disagree” with “disagree” and “strongly agree” with “agree.”
Data were collected and managed using REDCap. 17 Analysis was conducted using R version 3.4.1 18 and MedCalc. 19 Statistical significance was accepted at the 0.05 level, and all tests were two‐sided. No adjustments were made for multiple comparisons. All subjects gave informed consent to participate. This study was approved by the Hospital for Sick Children Research Ethics Board. Anonymized data will be shared by request from any qualified investigator.
3. RESULTS
Emails were distributed to the approximately 2450 Child Neurology Society members in November 2017 and May 2018 (Figure 1). The total number of practicing child neurologists within this group is unknown. In the November 2017 survey, there were 276 participants including 219 child neurologists and 3 pediatricians with additional epilepsy and/or neurophysiology subspecialty training. In the May 2018 survey, 231 child neurologists participated. Eighty‐four individuals completed the surveys at both timepoints. Merging child neurologist respondents yielded 369 unique child neurologists or pediatricians with advanced training in epilepsy.
FIGURE 1.
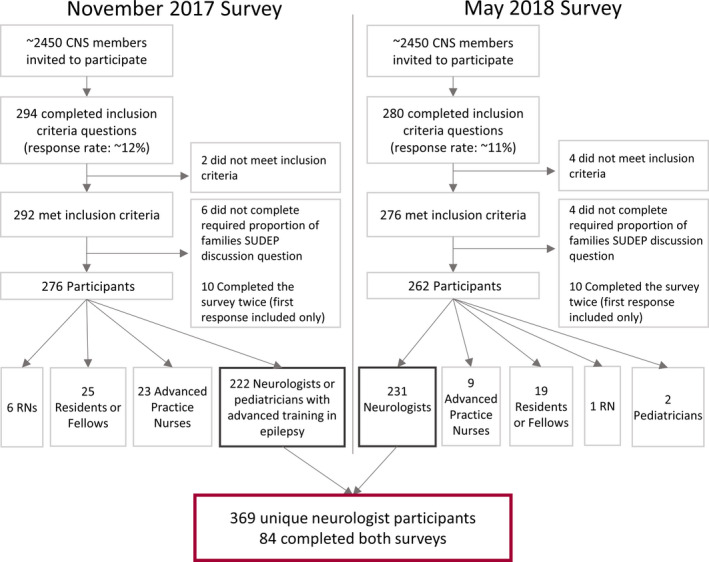
Study participants for November 2017 and May 2018 surveys
Most child neurologists in the pooled cohort (65%; n = 239) reported treating at least 50 patients for epilepsy in the past 6 months (Table 1). Stratified by survey timepoint, the number of patients treated for epilepsy in the past 6 months and the proportion of patients/families with whom they discuss SUDEP were similar (difference < 6.5% for each category between timepoint groups).
TABLE 1.
Characteristics of child neurologists who participated in the study at either time point
| Pooled Cohort a | Nov. 2017 Respondents | May 2018 Respondents b | |
|---|---|---|---|
| n | 369 | 222 | 147 |
| Patients treated for epilepsy in past 6 months, n (%) | |||
| <10 | 17 (4.6) | 11 (5.0) | 6 (4.1) |
| 11‐25 | 43 (11.7) | 27 (12.2) | 16 (10.9) |
| 26‐50 | 70 (19.0) | 47 (21.2) | 23 (15.6) |
| 51‐100 | 95 (25.7) | 56 (25.2) | 39 (26.5) |
| >100 | 144 (39.0) | 81 (36.5) | 63 (42.9) |
| Approximate proportion of epilepsy patients/families with whom neurologists discuss SUDEP | |||
| None (0%) | 5 (1.4) | 4 (1.8) | 1 (0.7) |
| Few (1%‐9%) | 94 (25.5) | 58 (26.1) | 36 (24.5) |
| Some (10%‐49%) | 137 (37.1) | 86 (38.7) | 51 (34.7) |
| Most (50%‐90%) | 88 (23.8) | 50 (22.5) | 38 (25.9) |
| All or almost all (>90%) | 45 (12.2) | 24 (10.8) | 21 (14.3) |
Includes only Nov. 2017 response of those who participated in both surveys (n = 84).
Excludes responses of those who also participated in Nov. 2017 survey (n = 84).
3.1. SUDEP discussion practice
Overall in the pooled cohort, 36% (n = 133) of child neurologists reported discussing SUDEP with at least half of their epilepsy patients/families, including 12% (n = 45) who reported discussing with > 90% of epilepsy patients or their families. On the May 2018 survey (n = 231), all respondents were queried about change in SUDEP discussion practice in the past 6 months, and 38% (n = 88) of child neurologists reported a change. Eighty‐nine percent (n = 79) reported increasing the proportion of epilepsy patients/families with whom they discuss SUDEP, and 67% (n = 59) reported increasing the amount of information they share about SUDEP when they discuss it.
3.2. AAN/AES SUDEP clinical practice guideline
Familiarity with the AAN/AES SUDEP Guideline 1 was associated with SUDEP discussion practice. About half (54%; n = 199) of survey respondents reported previously reading the AAN/AES SUDEP Guideline, and familiarity with the Guideline was associated with SUDEP discussion practice (χ2 = 20.0, df = 1, P < 0.001). Thirty‐six percent of those who discussed SUDEP with none or few of their patients reported previously reading the Guideline, while 54% of those who discussed with some of their patients, 68% who discussed with most, and 67% who discussed with all or almost all of their patients reported familiarity with the AAN/AES SUDEP Guideline.
3.3. Factors associated with discussion practice
Results from the multivariable model examining attitudes and opinions associated with discussion practice are presented in Table 2. Four predictors were included in the model after Spearman correlations were used to exclude correlated predictors. Respondents who agreed healthcare providers have an ethical obligation to talk about SUDEP were 5.7 (CI: 3.3, 10.0) times more likely to discuss SUDEP with an increasing proportion of patients than those who felt neutrally, and those who felt neutrally were 3.2 (CI: 1.1, 9.1) times more likely to discuss SUDEP with an increasing proportion of patients than those who disagreed. Other significant predictors included agreeing that they knew enough to talk about SUDEP (OR 3.5; CI 1.9, 6.6) and disagreeing that there is no enough time to talk about SUDEP (OR 2.1; CI 1.2, 3.6). Predictors associated with decreased likelihood of discussion included agreeing that talking about SUDEP could provoke excessive anxiety or worry (OR 0.4; CI 0.2, 0.7).
TABLE 2.
Proportional odds ordinal logistic regression model for increased SUDEP discussion practice
| Opinion | β | SE | OR (95% CI) | P‐value | |
|---|---|---|---|---|---|
| Talking about SUDEP with the patient/family can provoke excessive anxiety or worry | Disagree (n = 37, 10%) | 0.33 | 0.40 | 1.40 (0.64, 3.05) | 0.40 |
| Neutral (n = 88, 24%) | Reference category | ||||
| Agree (n = 244, 66%) | −0.90 | 0.27 | 0.41 (0.24, 0.69) | <0.001 | |
| Healthcare providers have an ethical obligation to talk about SUDEP | Disagree (n = 27, 7%) | −1.15 | 0.52 | 0.32 (0.11, 0.85) | 0.03 |
| Neutral (n = 100, 27%) | Reference category | ||||
| Agree (n = 242, 66%) | 1.73 | 0.29 | 5.65 (3.26, 9.99) | <0.001 | |
| There is not enough time to talk about SUDEP | Disagree (n = 156, 43%) | 0.74 | 0.28 | 2.11 (1.23, 3.64) | 0.007 |
| Neutral (n = 105, 28%) | Reference category | ||||
| Agree (n = 108, 29%) | −0.01 | 0.30 | 0.99 (0.55, 1.77) | 0.96 | |
| I know enough to talk about SUDEP | Disagree (n = 34, 9%) | −0.55 | 0.47 | 0.58 (0.22, 1.45) | 0.25 |
| Neutral (n = 83, 22%) | Reference category | ||||
| Agree (n = 252, 68%) | 1.25 | 0.32 | 3.49 (1.87, 6.63) | <0.001 |
P‐values shown in bold denote statistical significance at P < 0.05
3.4. Ethical obligation to discuss SUDEP
In the model‐building procedure for the proportional odds ordinal logistic regression model, feeling that healthcare providers have an ethical obligation to discuss SUDEP was correlated with 5 of the 6 excluded potential explanatory variables for SUDEP discussion practice, including generally, the benefits of talking about SUDEP with a patient/family outweigh potential harms; for many patients, there are opportunities to reduce the risk of SUDEP; there are no significant consequences to withholding information about SUDEP; my patients want to know about SUDEP; and talking about SUDEP can improve the doctor‐patient relationship. In an unadjusted correlation, belief that healthcare providers have an ethical obligation to discuss SUDEP had a Spearman correlation coefficient of ρ = 0.51 with child neurologists’ discussion practice. Of the 88 respondents who reported changing practice within the past 6 months on the May 2018 survey, 44% agreed or strongly agreed that feeling guilty for not talking about SUDEP was a reason for practice change while 24% disagreed or strongly disagreed with this statement (Figure 2A).
FIGURE 2.
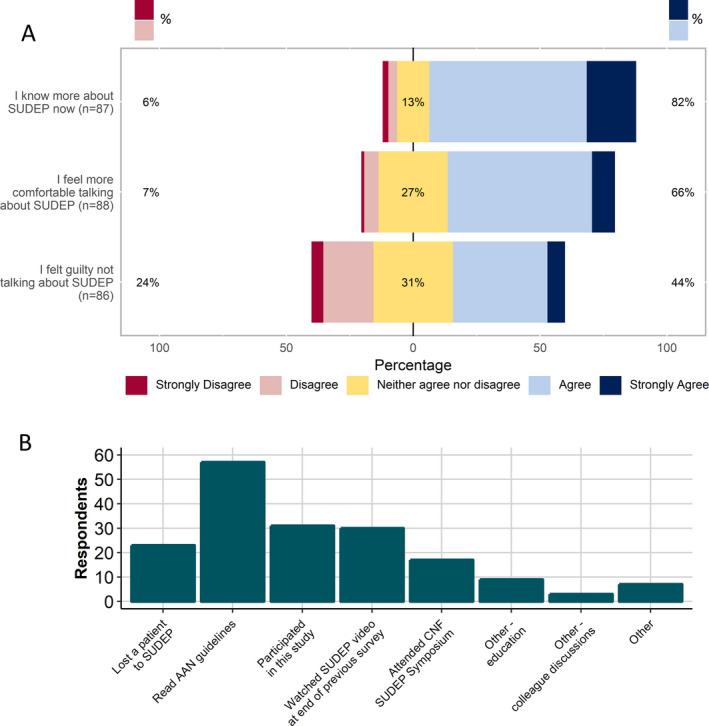
A, Themes for changing SUDEP discussion practice in the past 6 months reported by May 2018 survey respondents. B, Specific reasons for practice change in the past 6 months reported by May 2018 survey respondents
3.5. Anxiety or worry in patients/caregivers
Of 346 respondents, 71% (n = 244) of child neurologists agreed or strongly agreed that discussing SUDEP could provoke excessive anxiety or worry. Among the 45 child neurologists who discuss SUDEP with all or nearly all of their epilepsy patients/families, there was a trend toward those who routinely discuss SUDEP at diagnosis being less likely to agree that talking about SUDEP can provoke excessive anxiety or worry than those who do not routinely discuss at diagnosis (37% vs 67%, P = 0.07).
3.6. Knowledge of SUDEP
Feeling sufficiently knowledgeable to discuss SUDEP was significantly associated with discussion practice in the multivariable model. Agreement about feeling sufficiently knowledgeable to talk about SUDEP was associated with correct assessment (1 in 1000 1 or 1 in 5000 2 , 3 ) of pediatric SUDEP incidence (χ2 = 15.1, df = 2, P < 0.001), history (χ2 = 12.3, df = 2, P = 0.002), and frequency (χ2 = 19.3, df = 2, P < 0.001) of generalized tonic‐clonic seizures as a risk factor. There was no significant association between correct identification of SUDEP as the most common epilepsy‐ or seizure‐related cause of death and feeling sufficiently knowledgeable to discuss SUDEP (χ2 = 1.09, df = 2, P = 0.58). Responses to SUDEP knowledge questions are presented in Table 3.
TABLE 3.
Child neurologists’ knowledge of SUDEP
| Pooled cohorts | Agree know enough to discuss | Neither agree nor disagree | Disagree know enough to discuss | |
|---|---|---|---|---|
| N a | 369 | 252 | 59 | 34 |
| Approximate annual incidence of SUDEP in children with epilepsy, n (%) | ||||
| 1 in 100 | 12 (3.3) | 9 (3.6) | 0 (0.0) | 3 (9.1) |
| 1 in 1000 | 71 (19.7) | 53 (21.2) | 10 (16.9) | 6 (18.2) |
| 1 in 5000 | 127 (35.3) | 102 (40.8) | 11 (18.6) | 9 (27.3) |
| 1 in 10 000 | 59 (16.4) | 35 (14.0) | 13 (22.0) | 5 (15.2) |
| 1 in 15 000 | 14 (3.9) | 9 (3.6) | 2 (3.4) | 2 (6.1) |
| 1 in 50 000 | 8 (2.2) | 7 (2.8) | 1 (1.7) | 0 (0.0) |
| Not sure | 69 (19.2) | 35 (14.0) | 22 (37.3) | 8 (24.2) |
| Most common seizure/epilepsy related cause of death, n (%) | ||||
| SUDEP | 148 (48.4) | 111 (50.0) | 20 (45.5) | 10 (40.0) |
| Aspiration | 33 (10.8) | 22 (9.9) | 6 (13.6) | 5 (20.0) |
| Status epilepticus | 43 (14.1) | 26 (11.7) | 5 (11.4) | 6 (24.0) |
| Trauma or drowning | 82 (26.8) | 63 (28.4) | 13 (29.5) | 4 (16.0) |
| Factors associated with risk of SUDEP (check all that apply) | ||||
| History of generalized tonic‐clonic seizure | 271 (73.4) | 201 (79.8) | 36 (61.0) | 21 (61.8) |
| Frequency of generalized tonic‐clonic seizures | 311 (84.3) | 230 (91.3) | 44 (74.6) | 24 (70.6) |
| Specific anticonvulsant drugs | 21 (5.7) | 15 (6.0) | 3 (5.1) | 3 (8.8) |
| History of nocturnal seizures | 238 (64.5) | 175 (69.4) | 29 (49.2) | 20 (58.8) |
| History of Status Epilepticus | 182 (49.3) | 123 (48.8) | 35 (59.3) | 14 (41.2) |
| Sleep environment | 134 (36.3) | 104 (41.3) | 14 (23.7) | 11 (32.4) |
| Adult onset epilepsy | 18 (4.9) | 13 (5.2) | 1 (1.7) | 3 (8.8) |
| Not sure | 17 (4.6) | 9 (3.6) | 4 (6.8) | 3 (8.8) |
Includes only Nov. 2017 survey response of those who participated in both surveys (n = 84).
Learning about SUDEP was a key theme for reason for change in practice: 82% agreed or strongly agreed that they changed practice because they knew more about SUDEP (Figure 2A). Specific reasons for practice change included reading the AAN/AES SUDEP Clinical Practice Guideline (65%; n = 57) and participating in this study (35%; n = 31) (Figure 2B). This finding was consistent when examining the 84 child neurologists who completed both surveys. The proportion who agreed or strongly agreed they knew enough to talk about SUDEP on the November 2017 survey was similar between those who later reported changing practice and those who did not (67%). On the May 2018 survey, 83% of those who reported changing practice agreed or strongly agreed compared with 71% who agreed or strongly agreed but did not report practice change.
Approximately two‐thirds (n = 144) of child neurologists loaded the educational video about SUDEP at the end of the November 2017 survey, and 111 reported watching the full video. Of those who loaded the video, 74% (n = 107) agreed or strongly agreed they learned something new, and 63% (n = 90) agreed or strongly agreed that the video would change their clinical practice. Of the 90 child neurologists who planned to change practice as a result of watching the video, 32% (n = 29) discussed SUDEP with few of their patients, 32% (n = 29) discussed with some, 23% (n = 21) with most, and 12% (n = 11) with all or almost all. Among 84 child neurologists who completed both surveys, there was a trend toward the 58 individuals who loaded educational video at the end of the first survey being more likely to report a change in practice 6 months later (57% vs 39%; χ2 = 3.52, df = 1, P = 0.06) than the 26 individuals who completed both surveys but did not load the video. This association was significant when comparing those who reported watching the video to completion to those who did not (65% vs 29%; P = 0.001).
4. DISCUSSION
The AAN/AES Clinical Practice Guideline recommends discussing SUDEP risk with all patients with epilepsy or their caregivers; however, only 12% of the 369 child neurologists who participated in this study adhere to these recommendations. In a multivariable model, feeling ethically obligated to talk about SUDEP, feeling sufficiently knowledgeable about SUDEP, and disagreeing that there is insufficient time to talk about SUDEP were associated with an increased proportion of patients with whom child neurologists talk about SUDEP, while endorsing that discussing SUDEP could provoke excessive anxiety or worry for the patient or caregiver was negatively associated. Increased knowledge was the most commonly cited reason for changing SUDEP discussion practice, and the most commonly referenced source for this knowledge was the AAN/AES SUDEP Clinical Practice Guideline.
Compared with previous studies, our findings suggest a modest increase in the proportion of patients/families with whom neurologists discuss SUDEP (Figure 3). Relative to a survey of Canadian and American neurologists and child neurologists in 2011, a smaller proportion of respondents in the present study indicated they talk to none (1% vs 12%) or few (26% vs 31%) of their patients about SUDEP; a similar proportion discussing with some of their patients (37% vs 35%); and a greater proportion of providers discussing with most (24% vs 15%) or nearly all (12% vs 7%). 4 While this may reflect a difference in study populations—a blended cohort of adult and child neurologists compared with exclusively child neurologists—it may represent change in SUDEP discussion practice. We also found a smaller proportion of child neurologists stating that they do not discuss SUDEP with any patients than described in previous studies conducted in other countries. 5 , 6 , 7 , 14 , 20
FIGURE 3.
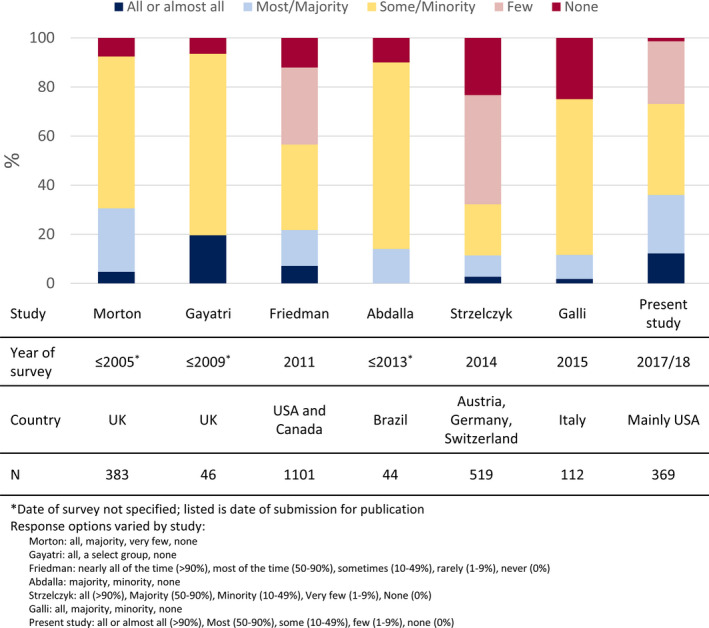
SUDEP discussion practices by neurologists and child neurologists across studies
Most child neurologists in our study agreed that SUDEP discussion could provoke excessive anxiety or worry in caregivers. This concern is consistent with past surveys of neurologists 4 , 7 but discordant with literature examining the effects of SUDEP disclosure on patients and families. 13 , 14 , 21 It is possible that excessive anxiety or worry perceived by child neurologists when discussing SUDEP does not persist after the end of the clinic visit, and child neurologists’ concerns are unfounded; however, other possible explanations for the discordance deserve consideration. Epidemiological understanding of SUDEP has improved 1 , 2 , 3 in recent years with reported current SUDEP incidence in children an order of magnitude more common than previously estimated in 2001 22 and recognition that SUDEP can occur in those without underlying conditions or intellectual disability. 23 One possibility is that the message currently conveyed to families is more ominous than that conveyed in previous research studies, potentially provoking excessive anxiety or worry. It is also possible that, in previous studies, families or patients have misunderstood or had limited understanding of SUDEP thus explaining the lack of emotional impact. 24
Families’ reactions perceived as excessively anxious or worrisome may also be partially attributable to the timing of the conversation. Literature from oncology indicates an important component of breaking bad news is the recipient's expectations. 25 We report a trend that among child neurologists who discuss with all or nearly all epilepsy patients/families, those who discuss at diagnosis were less likely to feel SUDEP discussion could provoke excessive anxiety or worry. While this was an exploratory analysis and the association may not be causal, it is consistent with literature from patients with epilepsy or their caregivers stating that they want to receive information about SUDEP at the time of diagnosis. 14 , 15 We hypothesize that diagnosis may be a preferable time for discussion of SUDEP as families may have expectations for worse news than at regular follow‐up visits; however, further work is necessary to confirm or refute this.
Improving SUDEP knowledge among child neurologists may increase the frequency with which child neurologists discuss SUDEP. There is room for improvement in child neurologists’ understanding of SUDEP: More than 40% did not know the incidence of pediatric SUDEP or selected an incorrect response option, and 16% did not know that the frequency of generalized tonic‐clonic seizures is associated with SUDEP risk. Most did not know that SUDEP is the most common epilepsy‐ or seizure‐related cause of death. The odds of discussing SUDEP with an increasing proportion of epilepsy patients/families was six times higher among those who felt they knew enough about SUDEP to discuss it. Knowledge was also the most important reason for changing practice to talk about SUDEP with more patients: Of the 88 child neurologists who reported changing their practice, 82% changed because they knew more about SUDEP.
Feeling ethically obligated to discuss SUDEP was associated with discussing it with an increased proportion of patients. Feeling an ethical obligation was correlated with five other potential predictors, including whether there are opportunities to reduce risk for many patients, and patients desire to know about SUDEP. We hypothesize that further education about SUDEP may impact child neurologists’ feeling of ethical obligation as patients do desire to know, 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 controlling seizures is associated with decreased risk, 1 and talking about SUDEP is consistent with modern medical ethics. 26
There is a long history of debate regarding SUDEP risk disclosure. Among this cohort of child neurologists, only 36% reported discussing SUDEP with at least half of their epilepsy patients or caregivers. Certain factors, such as the age of the child or epilepsy syndrome, may influence the decision to discuss SUDEP. While it has been previously reported that SUDEP is rarer in children, there is now data from at least 2 population‐based studies demonstrating that the risk of SUDEP in children is equal to that in adults 2 , 3 Further, although SUDEP is quite rare in certain epilepsy syndromes, it has been documented to occur even in self‐limited epilepsy syndromes. 27 Regardless of risk, discussion of SUDEP should be part of comprehensive epilepsy education given to all families of children with epilepsy. Full disclosure regarding the risks associated with epilepsy is consistent with ethical provision of care. 26 It has been well demonstrated that parents of children with epilepsy want to know about their child's risk 14 , 15 and health care providers represent the most reliable source for accurate information about a child's epilepsy. When SUDEP risk is low, the discussion can be reassuring to families that are anxious about their child's risk.
This study is subject to multiple limitations. First, those who elect to participate in a survey about SUDEP may not be an adequate representation of child neurologists in general: they may be more interested in SUDEP, know more about SUDEP, and perhaps be more likely to discuss SUDEP with their patients than those who do not participate. This could result in an overestimation of the proportion of patients/families with whom child neurologists discuss SUDEP. We anticipate our conclusion of a modest increase in discussion would be minimally impacted by this, as past surveys of neurologists suffer from the same limitation. Our response rate was about 15% total across the two surveys, though this is likely an underestimate as it is unknown how many of those who did not respond to the survey would have been eligible. While the response rate is low, it is consistent with surveys of physicians both about SUDEP and other topics. 4 , 28 , 29 Second, while the questionnaire was piloted by child neurologists in our community, it was not validated. Third, as we did not collect respondents’ identifying information, it is possible that some subjects participated in both surveys but were not linked due to changes between the information supplied for the 4 data points used to link. We attempted to minimize this possibility by explaining the purpose of the data points to respondents to encourage correct entry of the data points. It is also possible, though we believe unlikely, that multiple unique respondents had the same responses for the 4 data points. We hoped to include analyses evaluating the association between watching an educational video on SUDEP discussion and change in practice 6 months later, after controlling for confounding factors; however, due to the relatively small number of respondents completing both surveys, this objective could not be evaluated. Instead, we have presented descriptive statistics of the reasons cited by child neurologists for change in practice, which importantly suggest that education interventions for neurologists may be successful. Finally, the primary objective of this study was to characterize SUDEP discussion practices. We included analyses and exploration of factors associated with these practices as exploratory analyses. We encourage future research to confirm these findings. Additionally, future studies may also add to the literature by assessing demographic characteristics including subspecialty training and areas of practice interest. This may facilitate targeted recruitment for intervention studies evaluating for change in SUDEP discussion practice. This study did not address several important aspects of SUDEP discussion, namely inclusion of the child with epilepsy in the discussion about SUDEP and communication strategies and mediums for discussing SUDEP with families. We encourage future research to develop evidence‐based approaches in these areas.
The present study provides a detailed look at current child neurologists’ SUDEP discussion practices 6 and 12 months after publication the AAN/AES SUDEP Clinical Practice Guideline. We explored factors associated with discussion practice and reasons for practice change. Additional strengths of this study include a relatively large number (n = 369) of child neurologist respondents with diverse SUDEP discussion practices and preliminary evidence toward the impact of a video educational intervention on SUDEP discussion practice.
5. CONCLUSION
This study presents current evidence that most child neurologists do not follow the AAN/AES Clinical Practice Guideline recommendation that SUDEP risk be discussed with families of children with epilepsy. Child neurologists are concerned that discussing SUDEP could provoke excessive anxiety or worry for caregivers; however, when child neurologists feel they know enough about SUDEP and/or feel ethically obligated, they discuss SUDEP with a greater proportion of their patients. Importantly, we present limited data documenting an association between watching an educational video about SUDEP and, at 6‐month follow‐up, reporting a change in practice to discuss SUDEP with more patients. Future research should robustly explore the impact of educational interventions on neurologists’ SUDEP discussion practice. Additional future work should assess whether there are sustained negative emotional or mental health impacts to patients with epilepsy or their caregivers when learning current SUDEP information. Most importantly, this work should include evaluation of strategies to minimize this potential harm.
CONFLICT OF INTEREST
Elizabeth J. Donner has received honoraria from UCB and Eisai. The remaining authors have no conflicts of interest. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Supporting information
Supplementary Material
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank Cyndi Wright and Amy Brin (Child Neurology Foundation) for their support of this project.
Keller AE, Whitney R, Donner EJ. Why child neurologists talk about SUDEP: Results from two cross‐sectional surveys. Epilepsia Open. 2021;6:195–205. 10.1002/epi4.12465
REFERENCES
- 1. Harden C, Tomson T, Gloss D, Buchhalter J, Cross JH, Donner E, et al Practice guideline summary: sudden unexpected death in epilepsy incidence rates and risk factors. Neurology. 2017;88(17):1674–80. [DOI] [PubMed] [Google Scholar]
- 2. Sveinsson O, Andersson T, Carlsson S, Tomson T. The incidence of SUDEP: a nationwide population‐based cohort study. Neurology. 2017;89(2):170–7. [DOI] [PubMed] [Google Scholar]
- 3. Keller AE, Whitney R, Li S‐A, Pollanen MS, Donner EJ. Incidence of sudden unexpected death in epilepsy in children is similar to adults. Neurology. 2018;91(2):e107–e111. [DOI] [PubMed] [Google Scholar]
- 4. Friedman D, Donner EJ, Stephens D, Wright C, Devinsky O. Sudden unexpected death in epilepsy: knowledge and experience among U.S. and Canadian neurologists. Epilepsy Behav. 2014;35:13–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Galli F, Vignoli A, Canevini Maria P, Cerioli G, Vegni E. Sudden unexpected death in epilepsy (SUDEP) disclosure in pediatric epilepsy: an Italian survey on “to tell or not to tell”. Epilepsy Behav. 2017;67:33–8. [DOI] [PubMed] [Google Scholar]
- 6. Abdalla IG, Scorza CA, Cavalheiro EA, de Albuquerque M, de Almeida ACG, Scorza FA. Attitudes of Brazilian epileptologists to discussion about SUDEP with their patients: truth may hurt, but does deceit hurt more? Epilepsy Behav. 2013;27(3):470–1. [DOI] [PubMed] [Google Scholar]
- 7. Strzelczyk A, Zschebek G, Bauer S, Baumgartner C, Grond M, Hermsen A, et al Predictors of and attitudes toward counseling about SUDEP and other epilepsy risk factors among Austrian, German, and Swiss neurologists and neuropediatricians. Epilepsia. 2016;57(4):612–20. [DOI] [PubMed] [Google Scholar]
- 8. Long L, Cotterman‐Hart S, Shelby J. To reveal or conceal? Adult patient perspectives on SUDEP disclosure. Epilepsy Behav. 2018;86:79–84. [DOI] [PubMed] [Google Scholar]
- 9. Henning O, Nakken KO, Lossius MI. People with epilepsy and their relatives want more information about risks of injuries and premature death. Epilepsy Behav. 2018;82:6–10. [DOI] [PubMed] [Google Scholar]
- 10. Keddie S, Angus‐Leppan H, Parker T, Toescu S, Nash A, Adewunmi O, et al Discussing sudden unexpected death in epilepsy: Are we empowering our patients? A questionnaire survey. JRSM Open. 2016;7(9):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harden J, Tonberg A, Chin RF, McLellan A, Duncan S. “If you’re gonna die, you’re gonna die”: young adults’ perceptions of sudden unexpected death in epilepsy. Chronic Illn. 2015;11(3):230–41. [DOI] [PubMed] [Google Scholar]
- 12. Prinjha S, Chapple A, Herxheimer A, McPherson A. Many people with epilepsy want to know more: a qualitative study. Fam Pract. 2005;22(4):435–41. [DOI] [PubMed] [Google Scholar]
- 13. Fong CY, Lim WK, Kong AN, Lua PL, Ong LC. Provision of sudden unexpected death in epilepsy (SUDEP) information among Malaysian parents of children with epilepsy. Epilepsy Behav. 2017;75:6–12. [DOI] [PubMed] [Google Scholar]
- 14. Gayatri NA, Morrall MCHJ, Jain V, Kashyape P, Pysden K, Ferrie C. Parental and physician beliefs regarding the provision and content of written sudden unexpected death in epilepsy (SUDEP) information. Epilepsia. 2010;51(5):777–82. [DOI] [PubMed] [Google Scholar]
- 15. RamachandranNair R, Jack SM, Meaney BF, Ronen GM. SUDEP: What do parents want to know? Epilepsy Behav. 2013;29(3):560–4. [DOI] [PubMed] [Google Scholar]
- 16. RamachandranNair R, Jack SM. SUDEP: what do adult patients want to know? Epilepsy Behav. 2016;64:195–9. [DOI] [PubMed] [Google Scholar]
- 17. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap) ‐ a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. R Core Team . R: A Language and Environment for Statistical Computing [Internet]. Vienna, Austria; 2016. http://www.r‐project.org/ [Google Scholar]
- 19. MedCalc Statistical Software version 17.2 (MedCalc Software bvba, Ostend, Belgium; 2017. http://www.medcalc.org [Google Scholar]
- 20. Morton B, Richardson A, Duncan S. Sudden unexpected death in epilepsy (SUDEP): don’t ask, don’t tell? J Neurol Neurosurg Psychiatry. 2006;77(2):199–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Radhakrishnan DM, Ramanujam B, Srivastava P, Dash D, Tripathi M. Effect of providing sudden unexpected death in epilepsy (SUDEP) information to persons with epilepsy (PWE) and their caregivers‐Experience from a tertiary care hospital. Acta Neurol Scand. 2018;138(5):417–24. [DOI] [PubMed] [Google Scholar]
- 22. Donner EJ, Smith CR, Snead OC 3rd. Sudden unexplained death in children with epilepsy. Neurology. 2001;57(3):430–4. [DOI] [PubMed] [Google Scholar]
- 23. Berg AT, Nickels K, Wirrell EC, Geerts AT, Callenbach PMC, Arts WF, et al Mortality risks in new‐onset childhood epilepsy. Pediatrics. 2013;132(1):124–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tonberg A, Harden J, McLellan A, Chin RFM, Duncan S. A qualitative study of the reactions of young adults with epilepsy to SUDEP disclosure, perceptions of risks, views on the timing of disclosure, and behavioural change. Epilepsy Behav. 2015;42:98–106. [DOI] [PubMed] [Google Scholar]
- 25. Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES‐A six‐step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5(4):302–11. [DOI] [PubMed] [Google Scholar]
- 26. Ronen GM. Applying ethical principles in discussing SUDEP with patients and families. Epilepsy Behav. 2017;13–4. [DOI] [PubMed] [Google Scholar]
- 27. Doumlele K, Friedman D, Buchhalter J, Donner EJ, Louik J, Devinsky O. Sudden unexpected death in epilepsy among patients with benign childhood epilepsy with centrotemporal spikes. JAMA Neurol. 2017;74(6):645–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cook DA, Wittich CM, Daniels WL, West CP, Harris AM, Beebe TJ. Incentive and reminder strategies to improve response rate for internet‐based physician surveys: a randomized experiment. J Med Internet Res. 2016;18(9):e244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Viera AJ, Edwards T. Does an offer for a free on‐line continuing medical education (CME) activity increase physician survey response rate? A randomized trial. BMC Res Notes. 2012;5(1):129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material


