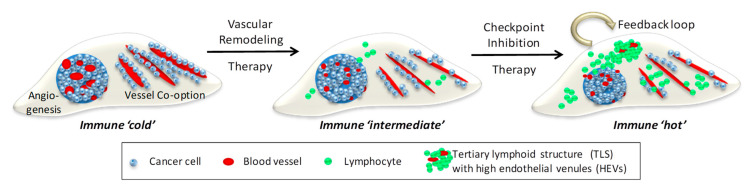
Figure 2.
Combination Vascular-Immune Therapy in Metastatic Cancer. Left, depicted are 2 distinct metastatic vascularization patterns in host tissue, neo-angiogenesis and co-option of existing blood vessels. Developing tumors are devoid of lymphocytes and therefore immune ‘cold’. Middle, vascular remodeling therapy, e.g., anti-angiogenesis and anti-co-option strategies, normalize aberrant angiogenic vessels and reduce cancer adhesion to pre-existing vessels. Improved tumor perfusion facilitates lymphocyte influx and alleviates immune suppression, thus creating an immune ‘intermediate’ environment. Right, this sets the stage for checkpoint inhibitors to activate local adaptive immunity and generate a positive feedback loop where normalized vessels increase T cell infiltration and activated effector T cells normalize blood vessels for more lymphocyte influx. A critical mass of T and B cells forms clusters resembling tertiary lymphoid structures (TLS) containing high endothelial venules (HEVs) which further support naive and memory T cell migration. A self-perpetuating immune ‘hot’ environment has been created following sequential vascular remodeling and immune enhancing combination therapies.