Reduction of tobacco use is a longstanding cardiovascular public health goal. A burgeoning array of novel tobacco products threaten to offset gains achieved in lowering cigarette smoking rates. Hookahs, or waterpipes, have been used for centuries, mainly in the Middle East, but their popularity has been growing worldwide. The uptake of hookah smoking in the United States has been attributed to the availability of flavored tobacco, advertising on social media, and the lack of regulation.1 Recent surveys report that 1 in 6 adults in the United States use hookahs and that most regular users are young adults, suggesting the potential for further increases in use.2 Furthermore, hookah smoking is associated with the use of other tobacco products and higher combustible cigarette consumption among youth, suggesting that hookah smoking may serve as a gateway to other tobacco products.2,3
Hookah smoking is often perceived to be safer than combustible cigarettes, largely because of the assumption that the water filters out carcinogens and toxicants and the perception that hookah uses more natural ingredients.4 Hookah smoke produced by traditional charcoal briquette heating contains particulate constituents similar to combustible cigarette smoke and delivers comparable levels of nicotine.5 However, the patterns of hookah use are different from the patterns of use of combustible cigarettes. Hookah smoking is usually intermittent, over the course of 30 to 60 minutes, and typically takes place in a social setting.2 During hookah use, charcoal briquettes heat the tobacco but do not achieve temperatures as high as combustible cigarette smoking (400°C versus 900°C).5 Consequently, hookah smoke contains higher levels of incomplete combusted products than combustible cigarette smoke, including higher carbon monoxide (CO) levels.5 More recently, an electric version of hookah (e-hookah) was developed that heats the tobacco by using a battery-powered device, much like electronic cigarettes. Whether produced by charcoal or electronic heating elements, hookah smoke contains multiple potential toxicants (Figure). The health effects of individual toxicants including flavorings and carbon monoxide remain incompletely understood.
Figure. Vascular effects of hookah use.
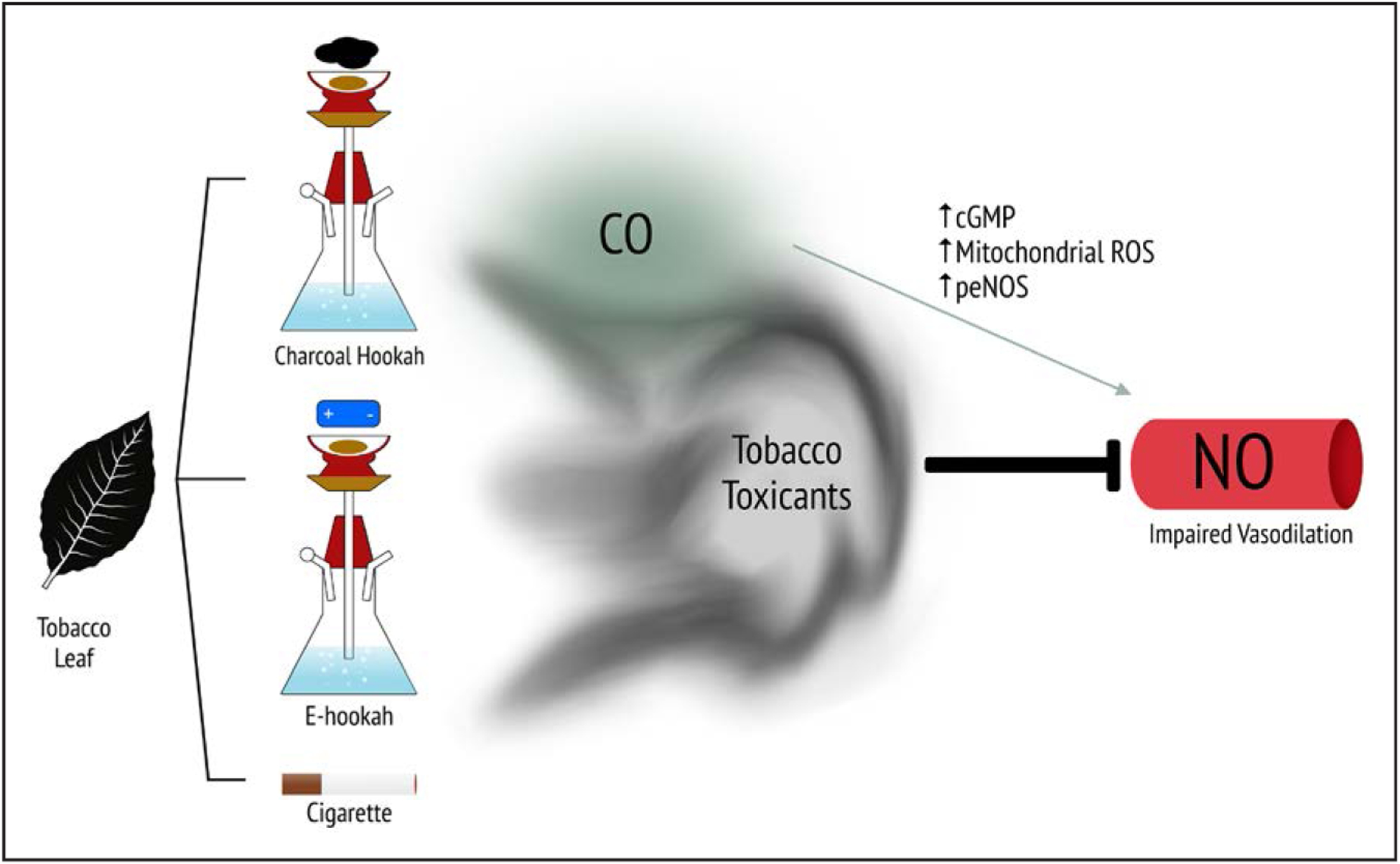
Tobacco leaf–derived product is heated electronically (e-hookah) or burned using charcoal briquettes or cigarettes, resulting in a complex cloud of smoke. Tobacco toxicants in tobacco smoke lower nitric oxide (NO) activity and block vasodilation. Charcoal-heated hookah smoke has greater amounts of carbon monoxide (CO), which masks the adverse effects on vascular function, potentially by altering mitochondrial ROS signaling, activating cGMP, and activating eNOS. In aggregate, hookah smoke produced by either charcoal or e-hookah impairs vasodilator function. peNOS indicates phosphorylated endothelial nitric oxide synthase; and ROS, reactive oxygen species.
Few prior studies have evaluated the cardiovascular effects of hookah use. The burden of long-term hookah use has been associated with the presence and severity of coronary artery disease.6 Acute charcoal-heated hookah smoking has been shown to increase measures of arterial stiffness, blood pressure, and sympathetic activation.7–10 Circulating apoptotic endothelial cell microparticles were found to be higher in occasional hookah smokers than in nonsmokers, further suggesting that hookah use is associated with vascular injury.11 In vitro treatment of endothelial cells with hookah smoke extract decreased cell viability and pro-liferation, increased the number of cells in cell cycle arrest, increased oxidative stress, decreased both endothelial nitric oxide synthase and AMP-activated protein kinase signaling, and increased inflammatory signaling.12 Collectively, these studies suggest that hookah use is associated with vascular stiffening, sympathetic activation, and endothelial cell dysfunction.
In this issue of Circulation, Rezk-Hanna and colleagues13 report the results of a carefully conducted controlled-exposure study comparing the acute vascular effects of electrically and charcoal-heated hookah smoking. It is surprising that flow-mediated vasodilation increased following the use of a charcoal-heated hookah, an observation that at first interpretation suggests an augmentation of endothelial function. In contrast, use of an e-hookah decreased flow-mediated dilation in a fashion similar to that induced by smoking a combustible cigarette. As expected from prior studies, exhaled CO levels were 9-fold higher following charcoal-heated hookah use in comparison with either electrically heated hookah or cigarette smoking. Inhalation exposure to CO in hookah users increased flow-mediated dilation to a greater degree than charcoal-heated hookah smoking with similar exhaled CO levels. These findings provide evidence that CO acts as a vasodilator in humans and that charcoal-heated hookah use produces additional tobacco toxicants that counteract the vasodilation induced by CO.
CO is a gaseous compound and well-known pollutant that is increasingly recognized as a signaling molecule.14 The major sources of external CO exposure are environmental exposures such as tobacco smoke, but CO is also produced in small amounts in the body. Endogenous production of CO by heme oxygenase inhibits mitochondrial cytochrome C, increasing reactive oxygen species creation to activate protective signaling pathways. Furthermore, CO, like nitric oxide, activates cGMP, leading to vasodilation. In addition, CO may stimulate endothelial nitric oxide synthase–mediated nitric oxide production, through Akt-mediated phosphorylation and calcium release.15 The present study indicates that inhalation of exogenous CO augments nitric oxide bioactivity that may be attributable to either decreased oxidative stress or increased nitric oxide production. In the case of charcoal-heated hookah smoke inhalation, the vascular effects of CO cover, in part, the adverse effects of the other tobacco smoke toxicants. It is important to note that the net vascular effect, whether a benefit or harm from CO, likely depends on many factors including endogenous or exogenous sources, level, and duration of exposure. The chronic vascular effects of CO exposure in conjunction with hookah smoke remain to be defined.
Several additional questions remain unanswered by the Rezk-Hanna et al study. Hookahs are often smoked in a social setting, with hookah bars being especially popular among college students.2 Consequently, hookah users are exposed to secondhand hookah smoke that may have different components and additional cardiovascular effects. Future studies are needed to evaluate the long-term cardiovascular effects of nondaily hookah use and to evaluate additional product characteristics, such as the different flavors of tobacco, which are especially appealing to youth, who are the predominant hookah smokers in the United States.
Misperceptions that hookah smoking is safer than cigarette smoking persist. The study by Rezk-Hanna et al provides scientific evidence indicating that acute exposure to hookah smoke, generated by either charcoal or electric heating, has vascular toxicity similar to combustible cigarette smoke. Additional longitudinal evidence is warranted, but the current available evidence supports efforts to enhance educational and regulatory efforts to reduce hookah use and prevent further youth uptake.
Sources of Funding
Drs Fetterman and Hamburg are supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award Nos. 5P50HL120163 and U54HL120163, and an American Heart Association Mentored Clinical and Population Research Award 17MCPRP32650002 (to Dr Fetterman). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosures
None.
REFERENCES
- 1.Maziak W, Taleb ZB, Bahelah R, Islam F, Jaber R, Auf R, Salloum RG. The global epidemiology of waterpipe smoking. Tob Control. 2015;24(suppl 1):i3–i12. doi: 10.1136/tobaccocontrol-2014-051903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robinson JN, Wang B, Jackson KJ, Donaldson EA, Ryant CA. Characteristics of hookah tobacco smoking sessions and correlates of use frequency among US adults: findings from wave 1 of the Population Assessment of Tobacco and Health (PATH) Study. Nicotine Tob Res. 2018;20:731–740. doi: 10.1093/ntr/ntx060 [DOI] [PubMed] [Google Scholar]
- 3.Doran N, Godfrey KM, Myers MG. Hookah use predicts cigarette smoking progression among college smokers. Nicotine Tob Res. 2015;17:1347–1353. doi: 10.1093/ntr/ntu343 [DOI] [PubMed] [Google Scholar]
- 4.Castañeda G, Barnett TE, Soule EK, Young ME. Hookah smoking behavior initiation in the context of millennials. Public Health. 2016;137:124–130. doi: 10.1016/j.puhe.2016.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shihadeh A, Schubert J, Klaiany J, El Sabban M, Luch A, Saliba NA. Toxicant content, physical properties and biological activity of waterpipe tobacco smoke and its tobacco-free alternatives. Tob Control. 2015;24(suppl 1):i22–i30. doi: 10.1136/tobaccocontrol-2014-051907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sibai AM, Tohme RA, Almedawar MM, Itani T, Yassine SI, Nohra EA, Isma’eel HA. Lifetime cumulative exposure to waterpipe smoking is associated with coronary artery disease. Atherosclerosis. 2014;234:454–460. doi: 10.1016/j.atherosclerosis.2014.03.036 [DOI] [PubMed] [Google Scholar]
- 7.Rezk-Hanna M, Doering L, Robbins W, Sarna L, Elashoff RM, Victor RG. Acute effect of hookah smoking on arterial stiffness and wave reflections in adults aged 18 to 34 years of age. Am J Cardiol. 2018;122:905–909. doi: 10.1016/j.amjcard.2018.05.033 [DOI] [PubMed] [Google Scholar]
- 8.Kadhum M, Jaffery A, Haq A, Bacon J, Madden B. Measuring the acute cardiovascular effects of shisha smoking: a cross-sectional study. JRSM Open. 2014;5:2054270414531127. doi: 10.1177/2054270414531127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson MD, Rezk-Hanna M, Rader F, Mason OR, Tang X, Shidban S, Rosenberry R, Benowitz NL, Tashkin DP, Elashoff RM, Lindner JR, Victor RG. Acute effect of hookah smoking on the human coronary microcirculation. Am J Cardiol. 2016;117:1747–1754. doi: 10.1016/j.amjcard.2016.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cobb CO, Sahmarani K, Eissenberg T, Shihadeh A. Acute toxicant exposure and cardiac autonomic dysfunction from smoking a single narghile waterpipe with tobacco and with a “healthy” tobacco-free alternative. Toxicol Lett. 2012;215:70–75. doi: 10.1016/j.toxlet.2012.09.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strulovici-Barel Y, Shaykhiev R, Salit J, Deeb RS, Krause A, Kaner RJ, Vincent TL, Agosto-Perez F, Wang G, Hollmann C, Shanmugam V, Almulla AM, Sattar H, Mahmoud M, Mezey JG, Gross SS, Staudt MR, Walters MS, Crystal RG. Pulmonary abnormalities in young, light-use waterpipe (hookah) smokers. Am J Respir Crit Care Med. 2016;194:587–595. doi: 10.1164/rccm.201512-2470OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro effects of waterpipe smoke condensate on endothelial cell function: a potential risk factor for vascular disease. Toxicol Lett. 2013;219:133–142. doi: 10.1016/j.toxlet.2013.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rezk-Hanna M, Mosenifar Z, Benowitz NL, Rader F, Rashid M, Davoren K, Moy NB, Doering L, Robbins W, Sarna L, Li N, Chang LC, Elashoff RM, Victor RG. High carbon monoxide levels from charcoal combustion mask acute endothelial dysfunction induced by hookah (waterpipe) smoking in young adults. Circulation. 2019;139:2215–2224. doi: 10.1161/CIRCULATIONAHA.118.037375 [DOI] [PubMed] [Google Scholar]
- 14.Rochette L, Cottin Y, Zeller M, Vergely C. Carbon monoxide: mechanisms of action and potential clinical implications. Pharmacol Ther. 2013;137:133–152. doi: 10.1016/j.pharmthera.2012.09.007 [DOI] [PubMed] [Google Scholar]
- 15.Yang PM, Huang YT, Zhang YQ, Hsieh CW, Wung BS. Carbon monoxide releasing molecule induces endothelial nitric oxide synthase activation through a calcium and phosphatidylinositol 3-kinase/Akt mechanism. Vascul Pharmacol. 2016;87:209–218. doi: 10.1016/j.vph.2016.09.010 [DOI] [PubMed] [Google Scholar]


