ABSTRACT
Background
To explore the impact of quarantine measures on the cause of death.
Methods
We use time series analysis with the data from death cause surveillance database of Suzhou from January 2017 to December 2019 to estimate the expected deaths from January to June 2020 and compare these expected deaths with the reported numbers of deaths.
Results
After the implementation of epidemic prevention measures in Suzhou in the first 3 months, overall number of all-cause deaths declined for 5.36, 7.54 and 7.02% compared with predicted numbers. The number of deaths from respiratory causes and traffic accidents declined shapely by 30.1 and 26.9%, totally. When quarantine measures were released (April–June), however, the observed numbers of total deaths exceeded the predicted deaths. People aged over 70 accounted for 91.6% of declined death number in respiratory causes and people aged over 60 accounted for 68.0% of declined death number in traffic accidents. Women over the age of 80 benefited the most from respiratory prevention (accounts for 41% of all reductions), whereas women aged over 60 benefited the most from traffic control (44%).
Conclusions
Overall, the whole population benefited from the epidemic prevention measures especially elderly females. This study is a useful supplement to encourage the government to develop regular preventive measures under the era of normalized epidemic.
Keywords: COVID-19, deaths, quarantine measures, time series analysis
Introduction
Cases of viral pneumonia of unknown cause were firstly reported in December 2019 in Wuhan, China, and spread rapidly across the country and over the world.1,2 On 11 February 2020, the World Health Organization officially named the virus COVID-19.3 This novel severe acute respiratory syndrome corona-virus is mainly transmitted through respiratory tract and people of any ages are vulnerable.4,5 The elderly and the infirm seem to be more susceptible to the infection of this virus and die of secondary severe respiratory problems or other diseases.6 The global epidemic has caused great losses and challenges to human beings.7,8
Powerful measures have been implemented by the Chinese government to contain the outbreak.9,10 Since 23 January 2020, the bus and subway ferry long-distance passenger service of Wuhan city had been suspended; the airport railway station was temporarily closed and citizens were not allowed to leave Wuhan without special reasons.11 In addition, the media have been following the progress of the epidemic on a daily basis, and the government has publicized the knowledge of disease prevention nationwide to enhance the people’s awareness of self-protection, including less out-going, keeping a social distance and wearing mask when you go out. People throughout the country responded positively to the government’s epidemic prevention measures.12,13
In the assessment of the evolution and impact of the pandemic, death is one of the clearest and worst outcomes. A national study in the USA estimated the number of excess deaths attributable to COVID-19 of its country from March to May 2020.14 The results show that the number of all-cause deaths is 28% higher than the number of officially reported deaths caused from COVID-19. In contrast, studies have shown that, with the exception of areas with severe outbreaks, such as Wuhan in China, both air pollution reduction and mortality benefit from the quarantine measures.15,16 The number of lives that were saved due to the decrease in air pollution potentially outnumbered the number of deaths directly due to COVID-19.17 Nevertheless, the extent to which the major causes of deaths are affected by epidemic prevention measures remains to be explored.
To estimate the mortality burden of a new infectious agent in the context of relatively strict quarantine measures, it is common to assess changes in rates of death. Time series analysis is a statistical method of dynamic data processing, which is based on random process theory and mathematical statistics method to study statistical laws followed by random data sequence, so as to solve practical problems.18 Exponential smoothing method and autoregressive integrated moving average (ARIMA) model concern relatively simple theory and do not contain much mathematics or statistics that are commonly used in time series analysis and prediction methods.19,20 Time series analysis has been successfully used in the field of medicine and public health for time series prediction of epidemic diseases21,22 and has been widely applied to predict trends in COVID-19 prevalence and deaths over the world.23
In this study, we estimated the expected deaths due to any cause in each month from January to June 2020 about Suzhou, China—a city affected by a mild COVID-19 outbreak if the pathogen had not circulated. We compare these estimates of expected deaths with the reported numbers of deaths to assess the impact of quarantine measures on all-cause mortality. These analyses may enhance our understanding of the importance of quarantine measures to some deaths and serve as useful evidence for formulating health protection guidelines.
Materials and methods
Data resource
All data in this study were obtained from the death cause surveillance database of Suzhou. The objects of the death registration report are all-cause deaths occurring in the area under the jurisdiction of Suzhou carried out by the district health service institutions and secondary or above hospitals. Basic information includes name, sex, date of birth, nationality, marriage, education, occupation, etc. Death information includes cause of death, date of death, place of death, etc. These data included the total number of all-cause deaths in Suzhou from January 2017 to June 2020 and were stratified by month. Descriptive statistics are given in supplementary materials. In this study, a time series containing 3 years, i.e. 36-month data were used to predict the deaths’ numbers in the next 6 months with 95% relative confidence intervals (CIs).
Prediction model
The prediction method of time series assumes that the change of the predicted object is only related to time, which is a simplification of the complex effect of external factors. According to its changing characteristics, time series analysis can be used to predict its future state based on the principle of inertia.
Exponential smoothing method is a kind of time series analysis and prediction method developed on the basis of moving average method. It is to predict the future of phenomena by calculating exponential smoothing value and combining with a certain time series prediction model. The principle is that the exponential smoothing value of any period is the weighted average of the actual observed value of the period and the exponential smoothing value of the previous period.24
ARIMA model refers to the model established by converting non-stationary time series into stationary time series. The dependent variable is only regressed to its hysteresis value and the present value and hysteresis value of the random error term. ARIMA model contains three parameters: p, d and q. `d’ represents the number of order differentiation required for the sequential data to be stable, also known as I. The general formula of AR (p) and MA (q) models can be expressed in equations.25 In addition, ARIMA model can be divided into seasonal model part and non-seasonal model part. Whether there is obvious seasonality can be judged according to the time series diagram.
The prediction model was selected in exponential smoothing method and ARIMA model using the Statistical Product and Service Solutions (SPSS) for Windows software package (ver.22.0, IBM) expert modeling method. The model choice is based on the stationary R2.
Results
We simulated the number of all-cause deaths and the number of deaths from each major cause over the past 36 months (from January 2017 to December 2019) in Suzhou city using a time series model and predict the deaths’ numbers in the next 6 months (January–June 2020). The time series modeler module of SPSS was used to establish the prediction model by using exponential smoothing method, and ARIMA model, respectively, the recommended model of each cause by SPSS, is a ‘simple seasonal’ model of an exponential smoothing method. The fitting effect of each model is shown in Supplementary Table 1. The outcome of these predictions is presented in Fig. 1. It can be seen from Fig. 1 that models have a good fitting effect expect ‘Tumor’. The distribution of deaths from each cause was generally seasonal, with no significant upward or downward trend.
Fig. 1.
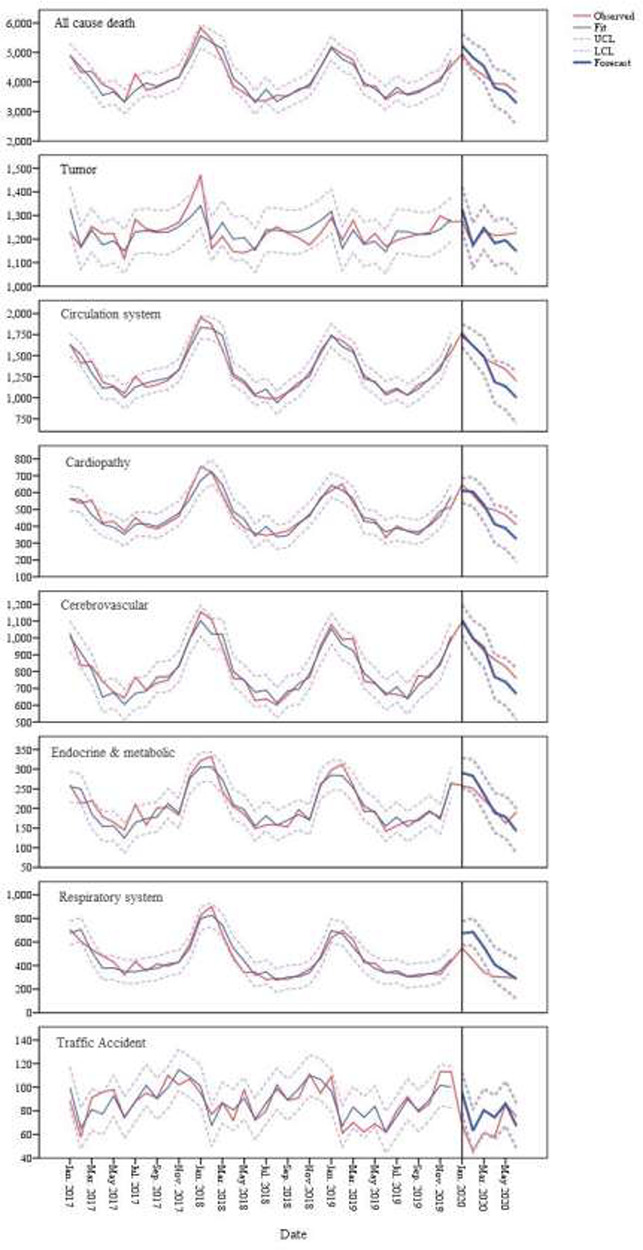
Trend fitting and prediction of all causes of death in Suzhou from January to June 2020.
Then, we compared these estimates of expected deaths with the reported numbers of deaths and the results are shown in Table 1. From January to March of 2020, the observed numbers of deaths from all causes and each major cause were relatively lower than that of the predicted death numbers. The observed deaths from January to March were 5.36, 7.54 and 7.02% lower than predicted data, respectively. The observed numbers of deaths from respiratory causes and traffic accidents were significantly lower than the predicted numbers statistically (the actual numbers of deaths were outside the 95% CI of the predicted number of deaths). In the first 3 months after quarantine measures (January to March) were implemented, the number of deaths from respiratory causes and traffic accidents declined by 30.1 and 26.9%, respectively. In the following 3 months (April–June), however, the observed numbers of deaths (except respiratory causes and traffic accidents) generally exceeded the predicted numbers. More intuitive difference could be seen in Fig. 2. As seen in Fig. 2, the predicted trend of total death is intersected with the actual observed value with poor consistency. From January to June, there is a ‘U’ trend of first decline and thenrise.
Table 1.
Comparison of observed and predicted deaths in Suzhou from January to June 2020
| Observed death | Predicted death (95% CI) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| January | February | March | April | May | June | January | February | March | April | May | June | |
| All-cause death | 4958 | 4464 | 4222 | 3940 | 3928 | 3636 | 5239 (4835, 5642) | 4828 (4335, 5320) | 4541 (3973, 5108) | 3807 (3173, 4441) | 3669 (2975, 4363) | 3284 (2535, 4033) |
| Circulation system | 1780 | 1616 | 1475 | 1402 | 1340 | 1200 | 1742 (1606, 1878) | 1621 (1483, 1804) | 1494 (1274, 1714) | 1189 (937, 1440) | 1136 (856, 1416) | 1002 (696, 1308) |
| Cerebrovascular | 1094 | 991 | 923 | 871 | 829 | 759 | 1107 (1016, 1197) | 998 (892, 1104) | 944 (824, 1063) | 768 (637, 899) | 739 (597, 881) | 668 (516, 820) |
| Cardiopathy | 647 | 587 | 512 | 497 | 466 | 408 | 611 (539, 648) | 606 (517, 694) | 529 (427, 631) | 412 (299, 526) | 389 (264, 513) | 323 (189, 457) |
| Respiratory system | 549 | 452 | 347 | 303 | 301 | 293 | 673 (573, 774) | 685 (568, 802) | 557 (425, 689) | 408 (263, 553) | 349 (192, 505) | 286 (118, 454) |
| Traffic accident | 68 | 46 | 61 | 58 | 86 | 75 | 95 (78, 113) | 63 (45, 81) | 80 (62, 99) | 74 (56, 93) | 86 (67, 105) | 67 (48, 86) |
| Endocrine & metabolic | 258 | 251 | 222 | 196 | 162 | 191 | 290 (252, 328) | 283 (240, 325) | 237 (191, 284) | 189 (138, 239) | 178 (125, 232) | 142 (85, 199) |
Fig. 2.
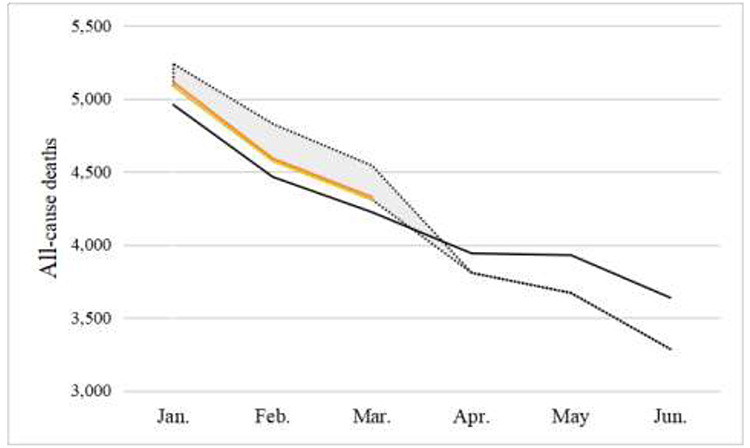
Observed deaths and predicted deaths in Suzhou from January to June 2020.
The observed number of deaths is indicated by the solid line, and the expected number of deaths is indicated by the dashed line. The shaded area represents a reduction of deaths due to respiratory causes and traffic deaths in the first 3 months.
Table 2 shows the comparison of 2020 and 2017–2019 deaths from respiratory causes and traffic accidents in Suzhou in the first 3 months by gender and age. As shown in Table 2, the deaths’ numbers from respiratory causes and traffic accidents in the first 3 months of 2020 were lower than that of the average deaths’ numbers of 2017–2019 in both genders and ages. The decline death in respiratory (−39.66% versus −31.16%) and traffic fatalities (−41.18% versus −22.45%) for women was higher than that for men. Among deaths from respiratory diseases, the absolute number over 70 years of age declined for 219 people, accounted for 91.6% of declined death number, and aged over 60 accounted for 68.0% of declined death number in traffic accidents. And women over the age of 80 benefited the most from the respiratory prevention (accounts for 41% of all reductions), whereas women aged over 60 benefited the most from traffic control (44%).
Table 2.
Comparison of 2020 deaths and 2017–2019 average deaths from respiratory causes and traffic accidents in Suzhou in the first 3 months by age and gender
| January to March 2020 | January to March 2017–2019 | Difference N (%) | Decline rate (%) | ||
|---|---|---|---|---|---|
| Respiratory system | |||||
| Gender | Male | 274 | 398 | −124 (51.9) | −31.16 |
| Female | 175 | 290 | −115 (48.1) | −39.66 | |
| Age (Male) | <60 | 5 | 8 | −3 (1.3) | −37.50 |
| 60− | 18 | 25 | −7 (2.9) | −28.00 | |
| 70− | 55 | 90 | −35 (14.6) | −38.89 | |
| 80− | 196 | 274 | −78 (32.6) | −28.47 | |
| Age (Female) | <60 | 1 | 4 | −3 (1.3) | −75.00 |
| 60− | 3 | 10 | −7 (2.9) | −70.00 | |
| 70− | 22 | 30 | −8 (3.3) | −26.67 | |
| 80− | 148 | 246 | −98 (41) | −39.84 | |
| Traffic accident | |||||
| Gender | Male | 38 | 49 | −11 (44) | −22.45 |
| Female | 20 | 34 | −14 (56) | −41.18 | |
| Age (Male) | <60 | 10 | 17 | −7 (28) | −41.18 |
| ≥60 | 28 | 34 | −6 (24) | −17.65 | |
| Age (Female) | <60 | 6 | 8 | −2 (8) | −25.00 |
| ≥60 | 14 | 25 | −11 (44) | −44.00 | |
Discussion
In this study, the simple seasonal exponential smoothing method was used to predict the death data in January–June 2020, which was regarded as the expected death value without the influence of external factors. By comparing with the actual observed death value, the trend change of the death data in January–June 2020 and the difference between the two were analyzed. The results showed that the predicted trend of total death was intersected with the actual observed value with poor consistency. From January to March, the observed number of total deaths was lower than the predicted total deaths, which was mainly caused by respiratory and traffic accidents death decline. From April to June, the observed numbers of total deaths exceeded the predicted deaths.
The global pneumonia pandemic caused by the COVID-19 virus has brought great impact and huge lose on human society. Nevertheless, there is still experience that the epidemic has brought to us. This virus was first reported in Wuhan, China, and quickly spread across the country taking the Spring Festival express. In the face of this highly contagious epidemic, the Chinese people have fought with one heart and one mind. The epidemic has also been brought under effective control by the government’s strong prevention and control measures (such as timely treatment of patients, strict isolation of the infected and contacts, protection of the vulnerable, and so on).26 Reducing travel, limiting congregational activities and wearing masks are key measures to stopping the spread of the disease.27 By the end of June 2020, China had recorded more than 80 000 confirmed cases and more than 4000 deaths, and most provinces have no local additions. This achievement is worthy of recognition (https://voice.baidu.com/act/newpneumonia/newpneumonia).
Suzhou is a large Chinese city located in East China with a population of about 7 million which has a stable population, developed economy and high medical level. During the virus outbreak, we found a declined trend in the number of all-cause deaths in the first few months in Suzhou after the implementation of the national epidemic prevention measures. In February and March, when preventive measures were fully implemented, the number of observed deaths was 7% lower than expected. The number of deaths from respiratory causes and traffic accidents had declined by 30.1 and 26.9% in the first 3 months. During the special period, Suzhou residents reduced their visits to relatives and friends, and hospitals took strict measures of disinfection and epidemic prevention and mask protection. People’s travel was strictly regulated by the government. The very stringent lock-downs were placed in China, leading to significant decrease in air pollution levels, and one study reported that the number of lives that were saved due to the decrease in air pollution potentially outnumbered the number of deaths directly due to COVID-19.17 Another research also found that during and in the months after the 2008 Beijing Olympics, the health status of populations in areas where air pollution levels fell appeared to improve.28
In addition to the significant decline in deaths from respiratory and traffic accidents, deaths from chronic diseases in other systems such as cardiopathy, cerebrovascular disease, endocrine and metabolic also declined. A study reported that improved air quality during the quarantine period avoided death of which were from cardiovascular diseases.17 And our study found that being at home may also associate with fewer deaths from endocrine and metabolic diseases. However, after 3 months, the outbreak was brought under control (Wuhan—the core city of COVID-19 in China—reported no new infections for the first time on 18 March. All the new confirmed cases in the Chinese mainland on 18 March were imported cases.), and social activities gradually returned to normal and medical institutions began to function. At the same time, the observed numbers of deaths of most causes exceeded the predicted numbers. We think that this may be the delayed compensatory death. Due to the opening of the hospital, it caused a rush of medical treatment and increased pressure on medical resources.29
Besides, this study found that the overall age benefited from the prevention measures. The absolute reduction in deaths was greatest among those over 70 years of age during the period of quarantine measures. The decline deaths in respiratory and traffic fatalities for women were both higher than that for men. And women over the age of 80 benefited the most from the respiratory prevention, whereas women aged 60 benefited the most from traffic control. This was likely because in China usually older women over the age of 60 were more likely to go out and buy food, but they were more confined to their homes during the epidemic, which also reduced their exposure to the outside world. We recommend that people, especially the elderly, wear masks on a regular basis when go out in autumn and winter.
Limitations
There are some limitations in this study. First, death rates are not compared, which can skew the results slightly. However, according to the results of this study, the main population of all-cause deaths is the elderly over 60 years old, and the floating population in Suzhou city is mainly young adults, which has a relatively low contribution to the death of chronic diseases. Second, Suzhou is just one city, and the larger picture still needs to be explored.
Conclusions
This study is based on the number of deaths observed in previous years to predict the number of deaths at baseline this year and to compare the observed and predicted number of deaths. We confirmed that under the quarantine measures, the number of all-cause deaths fell and the number of deaths from respiratory causes and traffic accidents were declined most significantly. The whole population would benefit from the epidemic prevention measures. Overall, our study is a useful supplement to encourage the government to develop regular preventive measures under the era of normalized epidemic.
Supplementary Material
Acknowledgement
This work was supported in part by the National Natural Science Foundation of China (81773541), funds from the Priority Academic Program Development of Jiangsu Higher Education Institutions at Soochow University, the National Key Laboratory of Radiation Medicine and Radiation Protection (GZK1201919) to ZT and by the Suzhou Science and Technology Development Project (SS201811) to HPS. The funding body did not play any roles in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Junjie Shen, Doctor of Public Health [DSc (PH)]
Congju Wang, Research Assistant
Chen Dong, Professor
Zaixiang Tang, Professor
Hongpeng Sun, Associate professor
Data availability
Our data are unidentified participant data. The datasets generated during and/or analyzed during the current study are not publicly available due to cooperation unit needs to be confidential, but are available from the corresponding author on reasonable request.
Conflict of interest
The authors declare no competing interests.
Authors’ contributions
HS and ZT conceptualized and designed the study. CW and CD were involved in data collection and categorization. JS, CW and CD were involved in real data analysis and interpretation. JS and HS led the drafting of the manuscript. All authors reviewed the manuscript.
Reference
- 1. Xu XW, Wu XX, Jiang XG et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ 2020;368:m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wei M, Yang N, Wang F et al. Epidemiology of coronavirus disease 2019(COVID-19) caused by SARS-CoV-2. Disaster Med Public Health Prep 2020;1–9. doi: 10.1017/dmp.2020.155. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. She J, Liu L, Liu W. COVID-19 epidemic: disease characteristics in children. J Med Virol 2020;92(7):747–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zou L, Ruan F, Huang M et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020;382(12):1177–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wei M, Yuan J, Liu Y et al. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA 2020;323(13):1313–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schijns V, Lavelle EC. Prevention and treatment of COVID-19 disease by controlled modulation of innate immunity. Eur J Immunol 2020;50(7):932–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bulut C, Kato Y. Epidemiology of COVID-19. Turk J Med Sci 2020;50(SI-1):563–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zachariah P, Johnson CL, Halabi KC et al. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a children's hospital in New York City, New York. JAMA Pediatr 2020;174(10):e202430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol 2020;92(6):568–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Awadasseid A, Wu Y, Tanaka Y, Zhang W. Initial success in the identification and management of the coronavirus disease 2019 (COVID-19) indicates human-to-human transmission in Wuhan. China Int J Biol Sci 2020;16(11):1846–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lau H, Khosrawipour V, Kocbach P et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med 2020;27(3):taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sun P, Lu X, Xu C et al. Understanding of COVID-19 based on current evidence. J Med Virol 2020;92(6):548–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Xu S, Li Y. Beware of the second wave of COVID-19. Lancet 2020;395(10233):1321–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Weinberger DM, Chen J, Cohen T et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med 2020;180(10):1336–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chauhan A, Singh RP. Decline in PM2.5 concentrations over major cities around the world associated with COVID-19. Environ Res 2020;187:109634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Son JYFK, Heo S, Kim H et al. Reductions in mortality resulting from reduced air pollution levels due to COVID-19 mitigation measures. Sci Total Environ 2020;744:141012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chen K, Wang M, Huang C et al. Air pollution reduction and mortality benefit during the COVID-19 outbreak in China. Lancet Planet Health 2020;4(6):e210–e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Coenen AR, Hu SK, Luo E et al. Primer for microbiome time-series analysis. Front Genet 2020;11:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Singh RK, Rani M, Bhagavathula AS et al. Prediction of the COVID-19 pandemic for the top 15 affected countries: advanced autoregressive integrated moving average (ARIMA) model. JMIR Public Health Surveill 2020;6(2):e19115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liu H, Li C, Shao Y et al. Forecast of the trend in incidence of acute hemorrhagic conjunctivitis in China from 2011-2019 using the seasonal autoregressive integrated moving average (SARIMA) and exponential smoothing (ETS) models. J Infect Public Health 2020;13(2):287–94. [DOI] [PubMed] [Google Scholar]
- 21. Cao LT, Liu HH, Li J et al. Relationship of meteorological factors and human brucellosis in Hebei province. China Sci Total Environ 2020;703:135491. [DOI] [PubMed] [Google Scholar]
- 22. Zhou J, Ren GH, He HB et al. Application of the exponential smoothing model and ARIMA model in prediction of the endemic situation of schistosomiasis in Hunan Province. Zhongguo Xue Xi Chong Bing Fang Zhi Za Zhi 2020;32(3):236–41. [DOI] [PubMed] [Google Scholar]
- 23. Benvenuto D, Giovanetti M, Vassallo L et al. Application of the ARIMA model on the COVID-2019 epidemic dataset. Data Brief 2020;29:105340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Guan P, Wu W, Huang D. Trends of reported human brucellosis cases in mainland China from 2007 to 2017: an exponential smoothing time series analysis. Environ Health Prev Med 2018;23(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ceylan Z. Estimation of COVID-19 prevalence in Italy, Spain, and France. Sci Total Environ 2020;729:138817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ye Q, Wang B, Mao J et al. Epidemiological analysis of COVID-19 and practical experience from China. J Med Virol 2020;92(7):755–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med 2020;9(2):575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rich DQ, Kipen HM, Huang W et al. Association between changes in air pollution levels during the Beijing Olympics and biomarkers of inflammation and thrombosis in healthy young adults. JAMA 2012;307(19):2068–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu Z, Huang S, Lu W et al. Modeling the trend of coronavirus disease 2019 and restoration of operational capability of metropolitan medical service in China: a machine learning and mathematical model-based analysis. Glob Health Res Policy 2020;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Our data are unidentified participant data. The datasets generated during and/or analyzed during the current study are not publicly available due to cooperation unit needs to be confidential, but are available from the corresponding author on reasonable request.


