Abstract
Purpose
To report a case of a hemi-retinal vein occlusion (HRVO) in the setting of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Observations
A 32-year-old healthy male presented with a paracentral scotoma, retinal hemorrhages, and dilated and tortuous retinal vessels inferiorly in the right eye. He was diagnosed with HRVO in the setting of recent SARS-CoV-2 infection.
Conclusions and importance
Venous thromboembolic complications and coagulation abnormalities have been widely reported in association with SARS-CoV-2 infection. We highlight this case to raise awareness that a retinal vein occlusion in an otherwise healthy, young patient may be a potential manifestation of the thromboinflammatory state associated with SARS-CoV-2 infection.
Keywords: Retinal vein occlusion, SARS, COVID-19, Thromboembolism, Hypercoagulability, Retina
1. Introduction
Hemi-retinal vein occlusion (HRVO) is a variant of central retinal vein occlusion (CRVO) with hypercoagulability thought to be a risk factor, especially in younger patients.1 Abnormal hematologic parameters and an increased risk of venous thromboembolism are common among patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).2,3 We report a case of a young patient with a HRVO in the setting of SARS-CoV-2 infection.
2. Case report
A 32-year-old previously healthy male with fevers, cough, fatigue, and anosmia was diagnosed with SARS-CoV-2 infection with positive reverse transcriptase polymerase chain reaction (RT-PCR) testing from a nasopharyngeal swab. He was referred by his primary care doctor as he reported mild blurriness in his superior visual field in his right eye. The blurring was only present when looking at a light background and had been present for about two weeks. His visual acuity was 20/20 in both eyes and an initial dilated fundus examination was unremarkable. No further diagnostic imaging, including invasive testing such as fluorescein angiography, was performed to limit exposure to other patients and personnel in the clinic given his active infection. Two subsequent RT-PCR tests were positive, followed by two consecutive negative RT-PCR tests and the development of detectable serum IgG antibodies to SARS-CoV-2 about seven weeks after initial symptoms onset. He remained normotensive during and after the time of his illness with SARS-CoV-2.
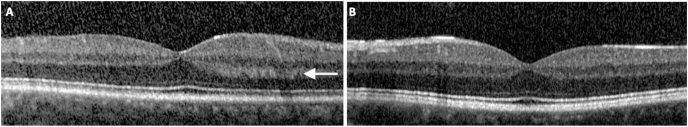
One month after his initial examination, he reported worsening symptoms with sudden onset paracentral scotoma in his right eye and was evaluated the same day. On examination, his visual acuity remained 20/20 in both eyes. Dilated fundus examination of the right eye showed rare scattered hemorrhages in the inferior hemisphere and dilated and tortuous vessels inferiorly (Fig. 1A). Fundus examination of the left eye appeared normal. Fluorescein angiography showed marked delay in filling of the inferior venous circulation (Fig. 1B–C) with late staining of those vessels OD (Fig. 1D). Optical coherence tomography of the macula showed no evidence of central macular edema OU, but there was mild thickening and increased hyperreflectivity of the outer plexiform layer nasally OD, corresponding to the patient's scotoma (Fig. 2).
Fig. 1.
Color photograph (A) and fluorescein angiogram (B–D) of right eye. Dilated and tortuous veins with scattered retinal hemorrhages (arrows) are seen in the inferior retina (A). Fluorescein angiography shows delayed venous filling (B, C) and late staining (D) of the inferior veins. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Optical coherence tomography of the right (A) and left (B) macula. There is mild thickening of the outer plexiform layer in the nasal macula of the affected right eye (A, arrow).
3. Discussion
HRVO and CRVO are believed to result from thrombus formation near the lamina cribosa.1 Classic risk factors include hypertension, cardiovascular disease, glaucoma, and diabetes mellitus. In younger patients without these risk factors, laboratory testing for clotting disorders may be considered; however, an extensive workup for thrombophilia risk factors is often negative.4 Most retina specialists only consider thrombophilia testing for select cases, such as patients with a personal history of thrombosis, family history of thrombosis at a young age, or an unusual presentation.
Indeed, in our patient, laboratory work up including PT, PTT, CBC, anti-cardiolipin antibodies, lupus anticoagulant, Factor V Leiden, protein C and S testing was unremarkable.
In patients with SARS-CoV-2, there is an increased propensity for thromboembolic complications, including both arterial and venous thrombotic events.5,6 Individuals with SARS-CoV-2 infection may have a number of coagulation abnormalities suggesting a hypercoagulable state, which has been called COVID-19 associated coagulopathy.3 Various studies of patients hospitalized with severe COVID-19 infection have significant rates of venous thromboembolic events, including deep venous thrombosis, pulmonary embolism, and catheter-associated thrombosis. Additionally, there have been reports of arterial thrombosis including stroke, limb ischemia, and heart attacks.3,7 Thrombotic events occurred in about 16% of hospitalized patients according to one study of New York City hospital systems.6 While there is limited data in the outpatient setting, SARS-CoV-2 patients may be at risk of venous thromboembolic events, potentially for an extended period of time after acute illness.8
Although this patient did not experience a generalized, systemic cytokine storm associated with more severe disease, milder endothelial damage may increase the risk for thrombosis even after the acute infection.8 Prior studies have demonstrated an association between pro-inflammatory cytokines and onset of venous thromboembolism, suggesting inflammation from recent infection may contribute to thromboembolic risk.9 Researchers postulate that COVID-19 may further elevate this risk given the abnormalities in hematologic markers of coagulation seen with viral infection from COVID-19.2,3In hospitalized patients with coagulopathy, lab abnormalities include modest prolongation of prothrombin times in about 5% of patients, mild thrombocytopenia in approximately 30% of patients, and elevated D-dimer values in 43%–60% of patients.10,11 Of note, D-dimer, fibrinogen, and platelets were within normal limits at the time of this patient's second presentation with more severe ocular symptoms and evidence of vein occlusion. However, this was about two months after the onset of acute infection, which was managed as an outpatient given his relatively mild respiratory symptoms.
4. Conclusions
Though we acknowledge the increasing seroprevalence of SARS-CoV-2 infection, especially among younger patients, and while a causal relationship cannot be established; it is plausible that HRVO in an otherwise healthy, young patient may be a manifestation of a thromboinflammatory state associated with SARS-CoV-2 infection. We highlight this case so that patients with visual symptoms may be properly evaluated and to raise awareness of the potential association of this pandemic infection with retinal venous thromboembolism.
Patient consent
Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support
Other disclosures
Dr. Finn has served as a consultant for Allergan and Genentech.
Dr. Khurana has served as a consultant for Alkahest, Allergan, Clearside Biomedical, Genentech and Regeneron; and received grant support from Allergan, Roche, Santen and Clearside Biomedical.
Dr. Chang has served as a consultant for Allergan.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
None of the authors listed have a proprietary interest in the material presented in this study.
References
- 1.Hayreh S.S., Hayreh M.S. Hemi-central retinal vein occlusion: pathogenesis, clinical features, and natural history. Arch Ophthalmol. 1980;98(9):1600–1609. doi: 10.1001/archopht.1980.01020040452011. [DOI] [PubMed] [Google Scholar]
- 2.Wong R.S.M., Wu A., To K.F. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. Br Med J. 2003;326(7403):1358–1362. doi: 10.1136/bmj.326.7403.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lahey J.M., Tunç M., Kearney J. Laboratory evaluation of hypercoagulable states in patients with central retinal vein occlusion who are less than 56 years of age. Ophthalmology. 2002;109(1):126–131. doi: 10.1016/S0161-6420(01)00842-9. [DOI] [PubMed] [Google Scholar]
- 5.Becker R.C. COVID-19 update: covid-19-associated coagulopathy. J Thromb Thrombolysis. 2020;50(1):54–67. doi: 10.1007/s11239-020-02134-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bilaloglu S., Aphinyanaphongs Y., Jones S., Iturrate E., Hochman J., Berger J.S. Thrombosis in hospitalized patients with COVID-19 in a New York city health system. J Am Med Assoc. July 2020 doi: 10.1001/jama.2020.13372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Emert R., Shah P., Zampella J.G. COVID-19 and hypercoagulability in the outpatient setting. Thromb Res. 2020;192:122–123. doi: 10.1016/j.thromres.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spencer F.A., Lessard D., Emery C., Reed G., Goldberg R.J. Venous thromboembolism in the outpatient setting. Arch Intern Med. 2007;167(14):1471–1475. doi: 10.1001/archinte.167.14.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemostasis. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levi M., Thachil J., Iba T., Levy J.H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7(6):e438–e440. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]