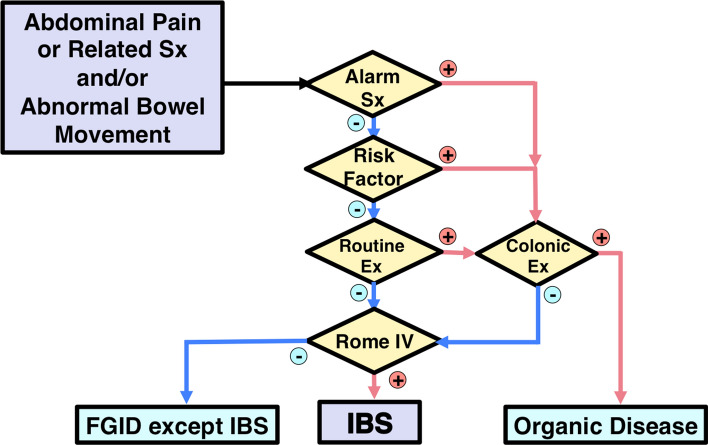
Fig. 1.
Diagnostic Algorithm for IBS. Check whether the answer is positive (yes) or negative (no) at the diamond. Alarm symptoms: bloody stool, unexpected weight loss more than 3 kg within 6 months, fever, and arthralgia. Alarm signs: palpable abdominal mass, abdominal fluctuation, palpable mass, or blood on the examining gloved finger on digital rectal examination. Risk factors: age over 50 years, past or family history of organic diseases of the colorectum, and patient’s requirement for colonic examination. Routine examinations: blood chemistry analyses including plasma glucose and thyroid-stimulating hormone, complete blood count, an inflammatory reaction such as (high-sensitive) C-reactive protein, urinalysis, fecal occult blood test, and plain abdominal X-ray. The colonic examination will be indicated if these factors are positive. Note that positive fecal occult blood, anemia, hypoproteinemia, or positive inflammatory reaction especially will require colonic examination. The colonic examination is mainly colonoscopy. It is the clinician’s responsibility to perform an adequate examination to reach an accurate diagnosis. The guidelines do not guarantee 100% exclusion of unexpected organic diseases. Depending on the clinical situation, the following examinations may be indicated: gastrointestinal mucosal biopsy, upper gastrointestinal endoscopy, barium enema, upper gastrointestinal series, abdominal ultrasonography, fecal ova test, stool bacterial culture, abdominal computed tomography, computed tomographic colonography, abdominal magnetic resonance imaging, small intestinal endoscopy, small intestinal fluoroscopy, lactose tolerance test, and hydrogen breath test. If clinical examinations results are negative and the Rome IV criteria are positive, a diagnosis of IBS is made. If the Rome IV criteria for IBS are negative, patients may be classified into other functional gastrointestinal disorders (FGIDs)