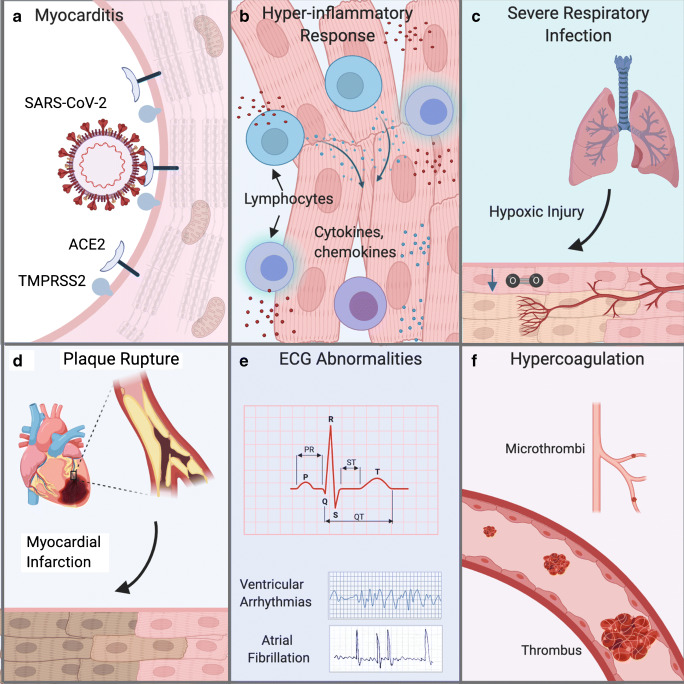
Fig. 2.
Various Routes to Cardiac Injury Due to SARS-CoV-2 Infection. (A) Several studies suggest that SARS-CoV-2 can directly infect cardiac cells of the myocardium and may cause heart damage by a “direct effect“. (B) The heart can also be injured by a systematic hyper inflammatory response that has been reported in COVID-19 patients by an “indirect effect“. High levels of cytokines and chemokines can cause ”bystander effects” and cardiac inflammation also classified as myocarditis or weakening of heart muscle function and may manifest as dilated cardiomyopathy (DCM) and/or heart failure. (C) Severe respiratory infection of SARS-CoV-2 infection can reduce pulmonary function and cause hypoxic injury in many organs including the heart due to low tissue oxygenation. (D) Increased stress on the cardiovascular system of COVID-19 patients can worsen underlying cardiac risk factors including rupture of atherosclerotic plaques leading to ST-segment myocardial infarction (STEMI) myocardial infarction. COVID-19 patients with severe infection can also exhibit non-STEMI myocardial infarction. (E) Various alterations in heart rhythm may occur as the first cardiac symptom in COVID-19 patients and can manifest as ventricular arrhytmias and atrial fibrillation that are detectable by electrocardiogram (ECG). (F) Coagulation abnormalities lead to formation of thrombi that can block blood flow in larger vessels or microthrombi that occlude small blood vessels and capillaries to affect microcirculation. The location and size of the blood vessel blockage dictate extent of ischemic tissue damage. Figure created with BioRender.com