Abstract
Parkinson’s disease (PD) is characterized by the degeneration of dopaminergic neurons in the substantia nigra and the formation of Lewy bodies. The mechanisms underlying these molecular and cellular effects are largely unknown. Previously, based on genetic and other data, we built a molecular landscape of PD that highlighted a central role for lipids. To explore which lipid species may be involved in PD pathology, we used published genome-wide association study (GWAS) data to conduct polygenic risk score-based analyses to examine putative genetic sharing between PD and blood levels of 370 lipid species and lipid-related molecules. We found a shared genetic etiology between PD and blood levels of 25 lipids. We then used data from a much-extended GWAS of PD to try and corroborate our findings. Across both analyses, we found genetic overlap between PD and blood levels of eight lipid species, namely two polyunsaturated fatty acids (PUFA 20:3n3-n6 and 20:4n6), four triacylglycerols (TAG 44:1, 46:1, 46:2, and 48:0), phosphatidylcholine aa 32:3 (PC aa 32:3) and sphingomyelin 26:0 (SM 26:0). Analysis of the concordance—the agreement in genetic variant effect directions across two traits—revealed a significant negative concordance between PD and blood levels of the four triacylglycerols and PC aa 32:3 and a positive concordance between PD and blood levels of both PUFA and SM 26:0. Taken together, our analyses imply that genetic variants associated with PD modulate blood levels of a specific set of lipid species supporting a key role of these lipids in PD etiology.
Subject terms: Genomics, Parkinson's disease
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disease, with a lifetime risk of 2% for men and 1.3% for women1,2. PD is characterized by a progressive loss of dopaminergic neurons that project from the substantia nigra (SN) to the striatum, the formation of so-called Lewy bodies (abnormal protein aggregates containing α-synuclein), and microgliosis3. The molecular mechanisms underlying these pathological hallmarks have predominantly been studied in familial forms of PD—which account for only 5–10% of the cases—or in animal models of toxin-induced PD (e.g., use of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), rotenone, or 6-hydroxydopamine)4–7. The etiology and pathophysiology of sporadic PD have not been elucidated, which hampers the development of effective, disease-modifying treatments. To acquire understanding of the mechanisms linked to (sporadic) PD, we previously used the results from genome-wide association studies (GWASs) and other (genetic) data from familial and sporadic PD patients to build a molecular landscape of the disease8. This unbiased, hypothesis-generating approach not only confirmed the processes and pathways that have been previously implicated in PD pathology (i.e., oxidative stress, endosomal–lysosomal function, endoplasmic reticulum stress, and a disturbed immune response) but also revealed that lipids play a central role in these processes and hence in PD etiology.
Lipids are mainly known for their role in energy storage9,10, but they are also the main constituent of cellular membranes, and part of membrane rafts and anchors as well as signaling and transport molecules11–15. According to LIPID MAPS, lipids are classified into eight different classes, namely fatty acyls, glycerolipids, glycerophospholipids, sphingolipids, sterols, prenols, saccharolipids, and polyketides16. This classification of lipids is based on their chemical and biochemical properties. In light of the data availability, we focus in this study on the lipids belonging to the first five classes, of which the structural characteristics are shown in Supplementary Fig. 1.
In short, fatty acyls are lipids synthesized by chain elongation of acetyl-CoA and are the building blocks of complex lipids. They include saturated fatty acids (such as palmitic acid), monounsaturated fatty acids (MUFA, such as oleic acid), polyunsaturated fatty acids (PUFAs, such as linoleic acid and docosahexaenoic acid), and fatty acid esters (such as acylcarnitines(AC)). Glycerolipids are composed of mono-, di-, and tri-substituted glycerols, such as monoacylglycerols (MAG), diacylglycerol (DAG), and triacylglycerol (TAG).
Glycerophospholipids (or phospholipids) have a glycerol backbone and a polar headgroup that allows the distinction of several subclasses, including phosphatidylcholine (PC), lysophosphatidylcholine (LPC), and lysophosphatidylethanolamine (LPE). Sphingolipids, such as sphingomyelin (SM), have a sphingoid base backbone synthesized from serine. Lastly, sterols are molecules with a fused four-ring core structure, and they include lipids such as cholesterol and cholesterol esters (CE).
Blood and cellular composition and levels are regulated by multiple factors, such as lipid intake17–19, gut microbiota20, microRNAs (e.g., miR-33 and miR-122)21, and regulatory proteins, e.g., sterol regulatory element-binding proteins, liver X receptors, p53, and AMPK22,23. Further, plasma transport of lipids like TAG, phospholipids, cholesterol, and CE occurs in complexes with apolipoproteins, creating lipoproteins, which can be classified into high-density lipoproteins (HDL), intermediate-density lipoproteins (IDL), low-density lipoproteins (VDL), and very-low-density lipoproteins (VLDL)24. In addition, the transport of fatty acids occurs in association with other proteins, such as albumin25. Therefore, variation in the genes encoding lipid-associated proteins may have a large effect on lipid regulation and disease outcome.
In order to examine the genetic overlap between PD and blood lipid levels, we used polygenic risk score (PRS)-based analysis to determine the extent of shared genetic etiology between PD and the blood levels of 370 lipids and lipid-related molecules, including fatty acyls, glycerolipids, glycerophospholipids, sphingolipids, sterols, and lipoproteins.
Results
Shared genetic etiology analyses
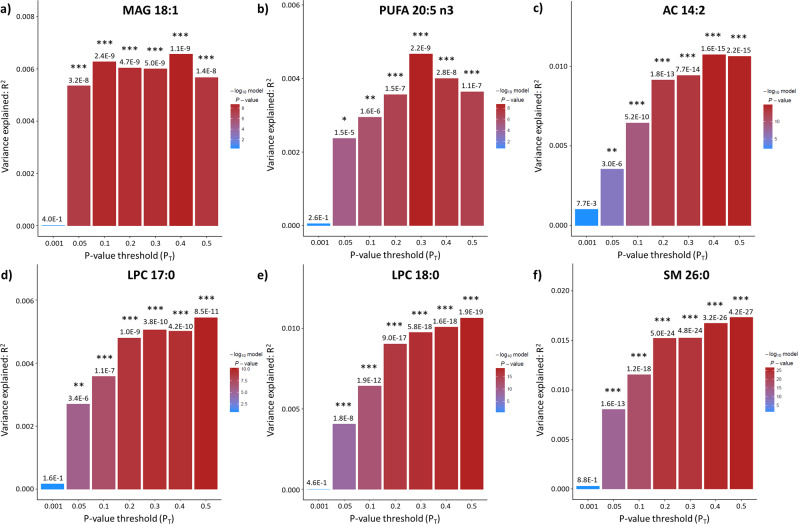
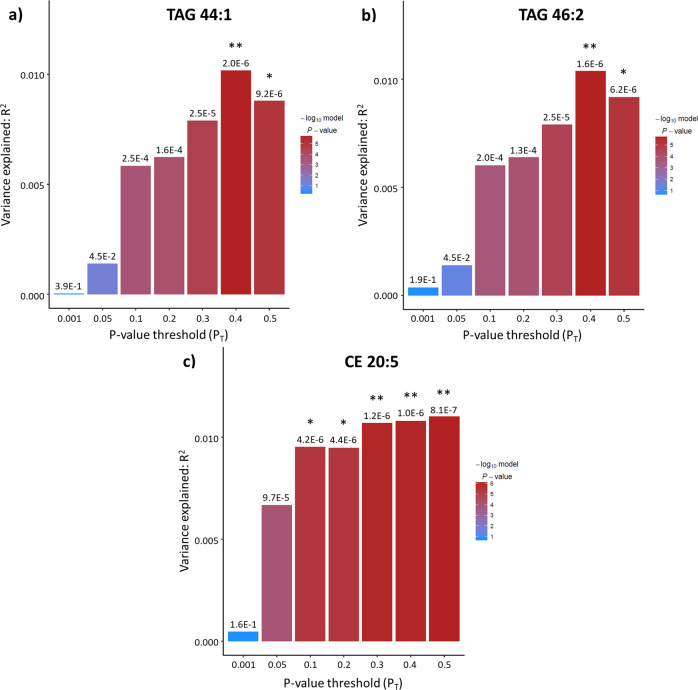
In this study, we determined the presence and extent of shared genetic etiology between PD and the blood levels of 370 lipids and lipid-related molecules. In phase I, we detected genetic overlap (at least one PT showing statistical significance after Bonferroni correction, i.e., P < 1.93E-05) between PD and the plasma levels of 25 lipids (Table 1). A complete overview of the results of all PRS-based analyses is shown in Supplementary Data 1. Of note, we found prominent genetic sharing between PD and the blood levels of six specific lipids (MAG 18:1, PUFA 20:5n3, AC 14:2, LPC 17:0, LPC 18:0, and SM 26:0) as each of these lipids showed significance—after Bonferroni correction—at all PTs, except for the lowest one (PT = 0.001) (Fig. 1). Further, genetic variants associated with PD explain at least 1% of the variation in blood levels of six lipids, i.e., the aforementioned AC 14:2, LPC 18:0, and SM 26:0, as well as TAG 44:1, TAG 46:2, and CE 20:5 (Figs. 1 and 2).
Table 1.
Summary of the results of the phase I PRS-based analyses of the genetic sharing between PD and the blood levels of 370 lipids and lipid-related molecules.
| Lipid class | Lipid sub-class | Total number of lipids | Number of lipids with P < 1.93E-05 | Number of lipids with R2 > 1% |
|---|---|---|---|---|
| Fatty acyls | Fatty acids | 60 | 4 | 0 |
| AC | 23 | 4 | 1 | |
| Glycerolipids | Metabolism | 2 | 0 | 0 |
| MAG | 4 | 1 | 0 | |
| DAG | 4 | 0 | 0 | |
| TAG | 47 | 4 | 2 | |
| Glycerophospholipids | PC aa | 37 | 1 | 0 |
| PC ae | 36 | 3 | 0 | |
| LPC | 14 | 3 | 1 | |
| LPE | 6 | 0 | 0 | |
| LPI | 3 | 0 | 0 | |
| Inositol metabolism | 3 | 0 | 0 | |
| Sphingolipids | SM | 10 | 2 | 1 |
| Sterols | CE | 11 | 1 | 1 |
| Cholesterol | 3 | 0 | 0 | |
| Other | 12 | 1 | 0 | |
| Lipoproteins | HDL | 24 | 1 | 0 |
| IDL | 6 | 0 | 0 | |
| LDL | 16 | 0 | 0 | |
| VLDL | 32 | 0 | 0 | |
| Apolipoproteins | 2 | 0 | 0 | |
| Others | Bile acid metabolism | 11 | 0 | 0 |
| Others | 4 | 0 | 0 |
AC acylcarnitine, MAG monoacylglycerol, DAG diacylglycerol, TAG triacylglycerol, PC phosphatidylcholine, PD Parkinson’s disease, aa diacyl, ae acyl-alkyl, LPC lysophosphatidylcholine, LPE lysophosphatidylethanolamine, LPI lysophosphatidylinositol, SM sphingomyelin, CE cholesterol ester, HDL high-density lipoprotein, IDL intermediate-density lipoprotein, LDL low-density lipoprotein, VDLD very-low-density lipoprotein.
Listed are the total number of lipid species examined per lipid class, the number of lipids that show Bonferroni-corrected significant genetic sharing (P < 1.93E-05) with PD for at least one SNP P value threshold (PT), and the number of lipids for which genetic variants associated with PD explain >1% of the variance (R2) in blood levels. In total, we found 25 lipids displaying significant genetic sharing with PD.
Fig. 1. Shared genetic etiology between Parkinson’s disease (PD) and blood levels of MUFA 18:1, PUFA 20:5n3, AC 14:2, LPC 17:0, LPC 18:0, and SM 26:0.
Bar plots for shared genetic etiology between PD and the blood levels of monounsaturated fatty acid 18:1 (a), polyunsaturated fatty acid 20:5n3 (b), acylcarnitine (AC) 14:2 (c), lysophosphatidylcholine (LPC) 17:0 (d), lysophosphatidylcholine (LPC) 18:0 (e), and sphingomyelin (SM) 26:0 (f) showing the variance explained (R2) and the SNP P value threshold (PT). The asterisks above the bars indicate the Bonferroni-corrected significance of the genetic overlap between PD and the blood lipid levels; * denotes P < 0.05/2590 tests (7 thresholds × 370 blood lipid levels) = 1.93E-05, ** denotes P < 0.01/2590 = 3.86E-06; *** denotes P < 0.001/2590 = 3.86E-07.
Fig. 2. Shared genetic etiology between Parkinson’s disease (PD) and blood levels of TAG 44:1, TAG 46:2, and CE 20:5.
Bar plots for shared genetic etiology between PD and the blood levels of triacylglycerol (TAG) 44:1 (a), triacylglycerol (TAG) 46:2 (b), and cholesterol ester (CE) 20:5 (c) showing the variance explained (R2) and the SNP P value threshold (PT). The asterisks above the bars indicate the Bonferroni-corrected significance of the genetic overlap between PD and the blood lipid levels; * denotes P < 0.05/2590 tests (7 thresholds × 370 blood lipid levels)=1.93E-05, ** denotes P < 0.01/2590 = 3.86E-06; *** denotes P < 0.001/2950 = 3.86E-07.
We then aimed to corroborate our results using a larger PD GWAS study as “base sample”. In phase II, we confirmed a significant shared genetic etiology—after Bonferroni correction, i.e., P < 0.05/175 tests (7 thresholds × 25 blood lipid levels) = 2.86E-04)—between PD and the blood levels of eight out of the 25 lipid species that we identified in phase I: PUFA 20:3n3 or n6, PUFA 20:4n6, TAG 44:1, TAG 46:1, TAG 46:2, TAG 48:0, PC aa 32:3, and SM 26:0 (Table 2).
Table 2.
Corroboration of the genetic overlap between PD and the blood levels of 25 lipids displaying significant genetic sharing with PD in phase I.
| Phase I | Phase II | |||||
|---|---|---|---|---|---|---|
| PT | P value | R2 | PT | P value | R2 | |
| 18:4n3 | 0.3 | 1.34E-07 | 3.60E-03 | 0.4 | 4.82E-02 | 3.77E-04 |
| 20:3n3 or n6 | 0.2 | 4.12E-07 | 3.30E-03 | 0.5 | 3.38E-05 | 2.16E-03 |
| 20:4n6 | 0.3 | 4.51E-06 | 2.67E-03 | 0.5 | 1.33E-06 | 2.99E-03 |
| 20:5n3 | 0.3 | 2.19E-09 | 4.66E-03 | 0.5 | 1.17E-03 | 1.26E-03 |
| AC 2:0 | 0.2 | 6.73E-06 | 2.53E-03 | 0.5 | 1.70E-02 | 6.01E-04 |
| AC 8:1 | 0.2 | 1.14E-05 | 2.40E-03 | 0.5 | 1.25E-02 | 6.72E-04 |
| AC 14:2 | 0.4 | 1.61E-15 | 1.07E-02 | 0.1 | 3.20E-03 | 1.29E-03 |
| AC 18:0 | 0.4 | 1.11E-06 | 3.30E-03 | 0.1 | 3.04E-02 | 5.20E-04 |
| MAG 18:1 | 0.4 | 1.08E-09 | 6.57E-03 | 0.1 | 4.78E-04 | 2.01E-03 |
| TAG 44:1 | 0.4 | 2.01E-06 | 1.02E-02 | 0.4 | 1.02E-05 | 1.01E-02 |
| TAG 46:1 | 0.4 | 1.37E-05 | 8.43E-03 | 0.3 | 1.18E-05 | 9.90E-03 |
| TAG 46:2 | 0.4 | 1.62E-06 | 1.04E-02 | 0.3 | 1.03E-05 | 1.00E-02 |
| TAG 48:0 | 0.4 | 1.91E-05 | 8.13E-03 | 0.4 | 1.42E-06 | 1.21E-02 |
| PC aa 32:3 | 0.4 | 1.85E-05 | 2.27E-03 | 0.5 | 1.23E-04 | 1.80E-03 |
| PC ae 32:2 | 0.4 | 1.52E-06 | 2.91E-03 | 0.05 | 2.58E-03 | 1.05E-03 |
| PC ae 38:1 | 0.5 | 5.14E-06 | 2.97E-03 | 0.3 | 2.19E-03 | 1.24E-03 |
| PC ae 44:6 | 0.4 | 8.19E-06 | 2.48E-03 | 0.05 | 2.79E-02 | 4.90E-04 |
| LPC 16:0 | 0.3 | 8.82E-07 | 3.05E-03 | 0.001 | 3.59E-03 | 9.67E-04 |
| LPC 17:0 | 0.5 | 8.52E-11 | 5.44E-03 | 0.3 | 9.83E-04 | 1.28E-03 |
| LPC 18:0 | 0.5 | 1.95E-19 | 1.06E-02 | 0.001 | 3.39E-03 | 9.80E-04 |
| SM 26:0 | 0.5 | 4.21E-27 | 1.73E-02 | 0.3 | 3.00E-05 | 2.45E-03 |
| SM 26:1 | 0.4 | 5.32E-06 | 2.59E-03 | 0.001 | 6.22E-04 | 1.39E-03 |
| CE 20:5 | 0.5 | 8.10E-07 | 1.10E-02 | 0.5 | 1.33E-02 | 2.73E-03 |
| 4-androsten-3beta,17beta-diol disulfate 1 | 0.5 | 3.75E-07 | 3.32E-03 | 0.3 | 1.12E-03 | 1.27E-03 |
| HDL-C | 0.2 | 1.02E-05 | 0.000841378 | 0.05 | 1.09E-01 | 7.01E-05 |
AC acylcarnitine, MAG monoacylglycerol, TAG triacylglycerol, PC phosphatidylcholine, PD Parkinson’s disease, aa diacyl, ae acyl-alkyl, LPC lysophosphatidylcholine, SM sphingomyelin, CE cholesterol ester, HDL high-density lipoprotein.
Comparison of the most significant P value threshold (PT), P value, and explained variance (R2) for the results obtained in phases I and II. Significant results after Bonferroni correction (phase I: P < 1.93E-05; phase II: P < 2.86E-04), are highlighted in bold. In total, eight lipids show significant genetic sharing with PD in both phase I and II.
Further, SECA analyses yielded significant evidence—after Bonferroni correction—of genetic pleiotropy (i.e., the same genetic variants affecting two traits) between PD and the blood levels of the eight lipids that were corroborated in phase II.
In addition, in both phase I and II, we found a significant negative genetic concordance between PD and the blood levels of TAG 44:1, TAG 46:1, TAG 46:2, TAG 48:0, and PC aa 32:3, which implies that genetic variants associated with PD contribute to decreased blood levels of these lipids. Conversely, we found a positive concordance between PD and the blood levels of PUFA 20:3n3 or n6, PUFA 20:4n6, and SM 26:0 (Table 3).
Table 3.
Comparison of the pleiotropy and concordance results generated using SNP effect concordance analysis (SECA) for the eight lipids for which we found significant genetic sharing in both phases I and II.
| Phase I | Phase II | |||||
|---|---|---|---|---|---|---|
| P value pleiotropy | P value concordance | Direction | P value pleiotropy | P value concordance | Direction | |
| 20:3n3 or n6 | 1 | <0.001 | + | <0.001 | <0.001 | + |
| 20:4n6 | <0.001 | <0.001 | + | <0.001 | <0.001 | + |
| TAG 44:1 | <0.001 | <0.001 | − | <0.001 | <0.001 | − |
| TAG 46:1 | <0.001 | <0.001 | − | <0.001 | <0.001 | − |
| TAG 46:2 | <0.001 | <0.001 | − | <0.001 | <0.001 | − |
| TAG 48:0 | <0.001 | <0.001 | − | <0.001 | <0.001 | − |
| PC aa 32:3 | <0.001 | <0.001 | − | <0.001 | <0.001 | − |
| SM 26:0 | <0.001 | <0.001 | + | <0.001 | <0.001 | + |
TAG triacylglycerol, PC phosphatidylcholine, aa diacyl, SM sphingomyelin, CE cholesterol ester.
The P values for genetic pleiotropy (same genetic variants affecting two traits) and concordance (agreement in genetic variant effect directions across two traits) are shown. In addition, for the concordances, the direction of the relationship is indicated by “+” (positive concordance) or “−” (negative concordance). All results except one (pleiotropy between PD and blood levels of 20:3n3 or n6 in phase I) reach Bonferroni-corrected significance (i.e., P < 0.05/32 tests (eight tests for pleiotropy and eight tests for concordance in both phase I and II) = 1.56E-03).
Discussion
Our PRS-based analyses using GWAS data of PD and the blood levels of 370 different lipids yielded a strong genetic link between PD and the blood levels of eight specific lipid species. More specifically, we determined genetic sharing and a positive genetic concordance between PD and the blood levels of two PUFA, namely PUFA 20:3n3 or n6 (also known as eicosatrienoic acid or dihomo-gamma-linoleic acid) and PUFA 20:4n6 (also known as arachidonic acid, AA). Increased levels of AA and dihomo-gamma-linoleic acid have been detected in the cerebrospinal fluid (CSF) of PD patients26. Furthermore, PD is associated with an increased intake of AA27, although not consistently28, and AA is not only linked to increased oxidative stress and neuroinflammation29,30 but it also induces α-synuclein aggregation31, which are three processes that have been implicated in PD etiology.
We further observed a negative concordance between PD and the blood levels of TAG 44:1, TAG 46:1, TAG 46:2, and TAG 48:0. Although there is no information regarding PD concerning these four specific TAG species, decreased blood levels of TAGs have been repeatedly observed in PD patients compared to controls32–37, high blood levels of TAGs have been reported as a protective factor for PD38,39, and A53T α-synuclein overexpression leads to decreased serum TAGs levels in animal models40. In addition, since TAG is positively correlated with body mass index (BMI)41, our results could indicate that PD patients may be genetically predisposed to a lower BMI. This agrees with a previous study that used GWAS data of PD and BMI and, applying Mendelian randomization, found that a higher BMI leads to a lower risk of PD42. Similarly, our results are in agreement with a study that used the same methodology but analyzed >5000 risk factors/phenotypic traits and found an inverse relationship between PD risk and adiposity43.
However, although we found overlap between PD and blood levels of specific TAGs, we did not observe genetic sharing between PD and total TAG blood levels. This could be partially due to the fact that the blood levels of TAGs are modulated by environmental factors44–46, such as diet and microbiome composition which have both been found to differ between PD patients and controls47,48.
In addition, we found a negative genetic concordance between PD and the blood levels of PC aa 32:3. PC has an anti-inflammatory role49 and it is the most abundant glycerophospholipid in eukaryotic membranes where it is involved in lipid homeostasis50. Blood levels of PC aa 32:3 have not been studied in PD but decreased levels of other PC species have been observed in plasma from PD patients51. This is in keeping with our finding that genetic variants associated with PD contribute to decreased levels of a specific PC species.
The strongest evidence of genetic sharing that we found was between PD and blood levels of SM 26:0. Furthermore, we found a positive concordance between PD and SM 26:0 blood levels, implying that genetic variants associated with PD contribute to increased levels of this lipid. SM is one of the constituents of the cellular membrane, and it is a source of bioactive lipids that play a role in processes such as autophagy52 and cell death53. Although it is not known what the blood levels of SM 26:0 in PD are, mutations in SMPD1, a gene encoding a sphingomyelin phosphodiesterase, which results in SM accumulation, are a risk factor for PD54–56. In addition, increased plasma levels of SM 26:0 have been described in the neurodegenerative disease X-linked adrenoleukodystrophy57. Interestingly, several molecular links between PD and X-linked adrenoleukodystrophy have been identified, including α-synuclein accumulation and oxidative stress58,59. Hence, elucidation of the physiological and pathological roles of SM 26:0 may contribute to the understanding of the molecular mechanisms underlying multiple neurodegenerative diseases.
Given the above, the genetic overlap between PD and the blood levels of specific lipids can be exploited for the identification of novel diagnostic biomarkers and for the elucidation of the molecular mechanisms underlying PD.
However, the current knowledge on the role of lipids in PD is fragmented60, which hinders drawing firm conclusions about the possible links between the disease and blood levels of the eight lipid species for which we found genetic sharing. Moreover, it should be noted that the blood lipid analysis did not make a distinction between lipid isobars (molecules with the same nominal mass) and lipid isomers (molecules with the same molecular formula, but a different chemical structure). For example, TAG 44:1 may correspond to 16 different species, such as TAG 12:0/12:0/20.1, TAG 14:0/14:0/16:1, or TAG 12:0/16:0/16:1. Therefore, the annotated species PUFA 20:3n3 or n6, PUFA 20:4n6, TAG 44:1, TAG 46:1, TAG 46:2, TAG 48:0, PC aa 32:3, and SM 26:0 may correspond to various isobars and isomers, and their exact identity of the species associated with PD thus remains to be determined. In addition, the lack of publicly available data regarding multiple lipid subclasses, such as ceramide-derived lipids and cardiolipin, prevented their inclusion in this study. It should also be noted that the authors cannot be certain that the publicly available data that were used in this study (i.e., the GWASs of blood lipid levels) do not have any overlap with the PD GWAS of phase II, which includes data from participants of the 23andMe consortium. The existence of this overlap could bias the obtained results.
The molecular mechanisms underlying PD have been mainly studied from a genetic, transcriptomic, and/or proteomic perspective, but little is known about the role of the metabolome, and in particular lipids, while our molecular PD landscape indicated a crucial role for lipids in the development of this neurodegenerative disease8. In this study, we found genetic sharing between PD risk and blood levels of eight lipids. In future studies, these lipids—including their isobars and isomers—should be further explored before they can possibly be used for the development of, e.g., lipid-directed dietary interventions or lipid-modifying drugs as treatment options to slow or perhaps even stop disease progression.
Methods
Shared genetic etiology analyses
In phase I, we used PRSice61 to determine the level of shared genetic etiology between PD and the blood levels of 370 different lipids and lipid-related molecules in the population.
As “base sample” for the polygenic risk score (PRS)-based analyses in PRSice (version 1.25), we used summary statistics data for 9581 PD cases and 33,245 matched controls from the PD GWAS reported by Nalls et al.62. These data were provided by the University of Tübingen, Germany, and contained data from all participants in phase I of the GWAS, except the participants of the 23andMe consortium. As “target samples” for the PRS-based analyses, we used summary statistics from the GWASs of 370 unique, different blood lipid levels, i.e., GWASs of 74 blood lipid levels from up to 2076 participants from Rhee et al.63, GWASs of 89 blood lipid levels from up to 7824 participants from Shin et al.64, GWASs of 106 blood lipid levels from up to 7478 participants from Draisma et al.65, and GWASs of 101 blood lipid levels from up to 24,925 participants from Kettunen et al.66. Before calculating shared genetic etiology, PRSice performed clumping using PLINK (version 1.90)67 to select independent index SNPs for each linkage disequilibrium (LD) block in the genome. Subsequently, we used the same approach that we, e.g., applied previously to determine the extent of genetic sharing between autism and autistic traits in the general population68. First, based on the significance level of the SNPs in the base sample, the index SNPs were selected and form clumps of all other SNPs that are within 500 kb and are in LD (r2 > 0.25)68. Second, based on the clumped summary statistics of the PD GWAS, PRSice then generated polygenic risk scores that are the sum of genome-wide SNPs associated with PD weighted by their effect sizes estimated from the PD GWAS, from which only the SNPs exceeding seven broad P value thresholds (PTs) were included. The seven thresholds that were used are 0.001, 0.05, 0.1, 0.2, 0.3, 0.4, and 0.561. Subsequently, PRSice calculated P values of shared genetic etiology—i.e., the extent to which the combined SNPs from each of the seven PT-linked polygenic risk scores for PD predict each of the target phenotypes (370 blood lipid levels)—between PD on one hand and each of the 370 blood lipid levels on the other hand. P values were considered significant if they exceeded the Bonferroni-corrected threshold accounting for the number of phenotypes tested (P < 0.05/2590 tests (7 thresholds × 370 blood lipid levels) = 1.93E-05). Subsequently and using the methodology described above, we tried to corroborate the significant findings from the phase I—i.e., the blood lipid levels for which we found Bonferroni-corrected significant P values of shared genetic etiology with PD—through conducting PRS-based analyses with summary statistics from a much larger GWAS of PD as “base sample” and summary statistics from the GWASs of the significant blood lipid levels as “target samples”. For phase II, we used data from the largest GWAS of PD reported thus far that contains all participants (PD cases and controls) in phases I and II from the 2014 GWAS by Nalls et al.62 (see above), including the 23andMe participants), as well as a large number of so-called “PD proxy-cases”—defined as those with a first degree relative with PD but no ICD-10 diagnosis or self-report of PD—and multiple new case–control samples. This resulted in GWAS data for a total of 37,688 PD cases, 18,618 PD proxy-cases, and 1,417,791 controls that were provided by the 23andMe consortium69.
SNP effect concordance analyses
We then performed SNP Effect Concordance analysis (SECA) for the corroborated findings from the PRS-based analyses. In SECA (http://neurogenetics.qimrberghofer.edu.au/SECA; see ref. 70 for more details), association results rather than individual genotyped data are analyzed to test for genetic pleiotropy (the same SNPs affecting both traits) and concordance (the agreement in SNP effect directions across both traits) between two genetically determined traits.
We used SECA to calculate empirical P values for pleiotropy and concordance between all blood lipid levels that emerged from the PRS-based analyses as having a significant shared genetic etiology with PD in both phases I and II. SECA P values lower than the Bonferroni-corrected threshold accounting for the number of tests that we performed were considered significant.
Reporting summary
Further information on experimental design is available in the Nature Research Reporting Summary linked to this paper.
Supplementary information
Acknowledgements
We are grateful to Dr. Manu Sharma and Professor Thomas Gasser from the University of Tubingen, Germany for providing us with the summary statistics GWAS data for selected PD cases and controls from the PD GWAS reported by Nalls et al. in 201462. Furthermore, we thank Dr. Mike Nalls and the 23andMe consortium for providing access to the summary statistics from the largest GWAS of PD reported to date69.
Author contributions
Study conception and design: H.X., C.K., M.M., G.M., and G.P.; analysis and interpretation of the data: H.X., C.K., W.D.W., M.M., G.M., and G.P.; drafting and/or revising the paper: H.X., C.K., W.D.W., M.M., G.M., and G.P. All authors reviewed and approved the final version of this paper.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
The code and scripts are available from the corresponding author upon reasonable request.
Competing interests
Authors H.X., C.K., and W.D.W. have no competing interests. M.M. is an employee and G.M. is a director of NeuroDrug Research, Ltd., and G.P. is a director of Drug Target ID, Ltd. However, the activities of M.M., G.M., and G.P. at these companies do not constitute competing interests with regard to this paper.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41531-021-00168-9.
References
- 1.Ascherio A, Schwarzschild MA. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol. 2016;15:1257–1272. doi: 10.1016/S1474-4422(16)30230-7. [DOI] [PubMed] [Google Scholar]
- 2.Elbaz A, Carcaillon L, Kab S, Moisan F. Epidemiology of Parkinson’s disease. Rev. Neurol. 2016;172:14–26. doi: 10.1016/j.neurol.2015.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Dexter DT, Jenner P. Parkinson disease: from pathology to molecular disease mechanisms. Free Radic. Biol. Med. 2013;62:132–144. doi: 10.1016/j.freeradbiomed.2013.01.018. [DOI] [PubMed] [Google Scholar]
- 4.Vila M, Przedborski S. Targeting programmed cell death in neurodegenerative diseases. Nat. Rev. Neurosci. 2003;4:365–375. doi: 10.1038/nrn1100. [DOI] [PubMed] [Google Scholar]
- 5.Simola N, Morelli M, Carta AR. The 6-hydroxydopamine model of Parkinson’s disease. Neurotox. Res. 2007;11:151–167. doi: 10.1007/BF03033565. [DOI] [PubMed] [Google Scholar]
- 6.Cicchetti F, Drouin-Ouellet J, Gross RE. Environmental toxins and Parkinson’s disease: what have we learned from pesticide-induced animal models? Trends Pharmacol. Sci. 2009;30:475–483. doi: 10.1016/j.tips.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Kumaran R, Cookson MR. Pathways to Parkinsonism redux: convergent pathobiological mechanisms in genetics of Parkinson’s disease. Hum. Mol. Genet. 2015;24:R32–R44. doi: 10.1093/hmg/ddv236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klemann CJHM, et al. Integrated molecular landscape of Parkinson’s disease. npj Park. Dis. 2017;3:14. doi: 10.1038/s41531-017-0015-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horton TJ, et al. Fat and carbohydrate overfeeding in humans: different effects on energy storage. Am. J. Clin. Nutr. 1995;62:19–29. doi: 10.1093/ajcn/62.1.19. [DOI] [PubMed] [Google Scholar]
- 10.Lass A, Zimmermann R, Oberer M, Zechner R. Lipolysis—a highly regulated multi-enzyme complex mediates the catabolism of cellular fat stores. Prog. Lipid Res. 2011;50:14–27. doi: 10.1016/j.plipres.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holthuis JCM, Menon AK. Lipid landscapes and pipelines in membrane homeostasis. Nature. 2014;510:48–57. doi: 10.1038/nature13474. [DOI] [PubMed] [Google Scholar]
- 12.Fernandis AZ, Wenk MR. Membrane lipids as signaling molecules. Curr. Opin. Lipidol. 2007;18:121–128. doi: 10.1097/MOL.0b013e328082e4d5. [DOI] [PubMed] [Google Scholar]
- 13.Bieberich E. It’s a lipid’s world: bioactive lipid metabolism and signaling in neural stem cell differentiation. Neurochem. Res. 2012;37:1208–1229. doi: 10.1007/s11064-011-0698-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Welte MA, Gould AP. Lipid droplet functions beyond energy storage. Biochim. Biophys. Acta - Mol. Cell Biol. Lipids. 2017;1862:1260–1272. doi: 10.1016/j.bbalip.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Welte MA, et al. Expanding roles for lipid droplets. Curr. Biol. 2015;25:R470–R481. doi: 10.1016/j.cub.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fahy E, et al. Update of the LIPID MAPS comprehensive classification system for lipids. J. Lipid Res. 2009;50:S9–S14. doi: 10.1194/jlr.R800095-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kris-Etherton PM, et al. The effect of diet on plasma lipids, lipoproteins, and coronary heart disease. J. Am. Diet. Assoc. 1988;88:1373–1400. [PubMed] [Google Scholar]
- 18.Lamarche B, Couture P. Dietary fatty acids, dietary patterns, and lipoprotein metabolism. Curr. Opin. Lipidol. 2015;26:42–47. doi: 10.1097/MOL.0000000000000139. [DOI] [PubMed] [Google Scholar]
- 19.Ordovas JM. Gene-diet interaction and plasma lipid response to dietary intervention. Curr. Atheroscler. Rep. 2001;3:200–208. doi: 10.1007/s11883-001-0062-3. [DOI] [PubMed] [Google Scholar]
- 20.Ghazalpour A, Cespedes I, Bennett BJ, Allayee H. Expanding role of gut microbiota in lipid metabolism. Curr. Opin. Lipidol. 2016;27:141–147. doi: 10.1097/MOL.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernández-Hernando C, Suárez Y, Rayner KJ, Moore KJ. MicroRNAs in lipid metabolism. Curr. Opin. Lipidol. 2011;22:86–92. doi: 10.1097/MOL.0b013e3283428d9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldstein I, Rotter V. Regulation of lipid metabolism by p53—fighting two villains with one sword. Trends Endocrinol. Metab. 2012;23:567–575. doi: 10.1016/j.tem.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Angin Y, Beauloye C, Horman S, Bertrand L. Regulation of carbohydrate metabolism, lipid metabolism, and protein metabolism by AMPK. Exp. Suppl. 2016;107:23–43. doi: 10.1007/978-3-319-43589-3_2. [DOI] [PubMed] [Google Scholar]
- 24.Ramasamy I. Recent advances in physiological lipoprotein metabolism. Clin. Chem. Lab. Med. 2014;52:1695–1727. doi: 10.1515/cclm-2013-0358. [DOI] [PubMed] [Google Scholar]
- 25.van der Vusse GJ. Albumin as fatty acid transporter. Drug Metab. Pharmacokinet. 2009;24:300–307. doi: 10.2133/dmpk.24.300. [DOI] [PubMed] [Google Scholar]
- 26.Willkommen D, et al. Metabolomic investigations in cerebrospinal fluid of Parkinson’s disease. PLoS ONE. 2018;13:e0208752. doi: 10.1371/journal.pone.0208752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miyake Y, et al. Dietary fat intake and risk of Parkinson’s disease: a case-control study in Japan. J. Neurol. Sci. 2010;288:117–122. doi: 10.1016/j.jns.2009.09.021. [DOI] [PubMed] [Google Scholar]
- 28.Chen H, Zhang SM, Hernán MA, Willett WC, Ascherio A. Dietary intakes of fat and risk of Parkinson’s disease. Am. J. Epidemiol. 2003;157:1007–1014. doi: 10.1093/aje/kwg073. [DOI] [PubMed] [Google Scholar]
- 29.Ayala A, Muñoz MF, Argüelles S. Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell. Longev. 2014;2014:360438. doi: 10.1155/2014/360438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosenberger TA, et al. Rat brain arachidonic acid metabolism is increased by a 6-day intracerebral ventricular infusion of bacterial lipopolysaccharide. J. Neurochem. 2004;88:1168–1178. doi: 10.1046/j.1471-4159.2003.02246.x. [DOI] [PubMed] [Google Scholar]
- 31.Broersen K, Ruiperez V, Davletov B. Structural and aggregation properties of alpha-synuclein linked to phospholipase A2 action. Protein Pept. Lett. 2018;25:368–378. doi: 10.2174/0929866525666180326120052. [DOI] [PubMed] [Google Scholar]
- 32.Chan RB, et al. Elevated GM3 plasma concentration in idiopathic Parkinson’s disease: a lipidomic analysis. PLoS ONE. 2017;12:e0172348. doi: 10.1371/journal.pone.0172348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guo X, et al. The serum lipid profile of Parkinson’s disease patients: a study from China. Int. J. Neurosci. 2015;125:838–844. doi: 10.3109/00207454.2014.979288. [DOI] [PubMed] [Google Scholar]
- 34.Gregório ML, et al. Impact of genetic variants of apolipoprotein E on lipid profile in patients with Parkinson’s disease. Biomed. Res. Int. 2013;2013:641515. doi: 10.1155/2013/641515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wei Q, et al. Reduced serum levels of triglyceride, very low density lipoprotein cholesterol and apolipoprotein B in Parkinson’s disease patients. PLoS ONE. 2013;8:e75743. doi: 10.1371/journal.pone.0075743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cereda E, et al. Low cardiometabolic risk in Parkinson’s disease is independent of nutritional status, body composition and fat distribution. Clin. Nutr. 2012;31:699–704. doi: 10.1016/j.clnu.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Scigliano G, et al. Reduced risk factors for vascular disorders in Parkinson disease patients: a case-control study. Stroke. 2006;37:1184–1188. doi: 10.1161/01.STR.0000217384.03237.9c. [DOI] [PubMed] [Google Scholar]
- 38.Sääksjärvi K, Knekt P, Männistö S, Lyytinen J, Heliövaara M. Prospective study on the components of metabolic syndrome and the incidence of Parkinson’s disease. Parkinsonism Relat. Disord. 2015;21:1148–1155. doi: 10.1016/j.parkreldis.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 39.Vikdahl M, Bäckman L, Johansson I, Forsgren L, Håglin L. Cardiovascular risk factors and the risk of Parkinson’s disease. Eur. J. Clin. Nutr. 2015;69:729–733. doi: 10.1038/ejcn.2014.259. [DOI] [PubMed] [Google Scholar]
- 40.Guerreiro PS, et al. Mutant A53T α-synuclein improves rotarod performance before motor deficits and affects metabolic pathways. Neuromol. Med. 2017;19:113–121. doi: 10.1007/s12017-016-8435-5. [DOI] [PubMed] [Google Scholar]
- 41.Shamai L, et al. Association of body mass index and lipid profiles: evaluation of a broad spectrum of body mass index patients including the morbidly obese. Obes. Surg. 2011;21:42–47. doi: 10.1007/s11695-010-0170-7. [DOI] [PubMed] [Google Scholar]
- 42.Noyce AJ, et al. Estimating the causal influence of body mass index on risk of Parkinson disease: a Mendelian randomisation study. PLoS Med. 2017;14:e1002314. doi: 10.1371/journal.pmed.1002314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Noyce AJ, et al. The Parkinson’s disease Mendelian randomization research portal. Mov. Disord. 2019;34:1864–1872. doi: 10.1002/mds.27873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang Z, et al. Comparison of plasma triacylglycerol levels in vegetarians and omnivores: a meta-analysis. Nutrition. 2013;29:426–430. doi: 10.1016/j.nut.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 45.Mittendorfer B, Sidossis LS. Mechanism for the increase in plasma triacylglycerol concentrations after consumption of short-term, high-carbohydrate diets. Am. J. Clin. Nutr. 2001;73:892–899. doi: 10.1093/ajcn/73.5.892. [DOI] [PubMed] [Google Scholar]
- 46.Fu J, et al. The gut microbiome contributes to a substantial proportion of the variation in blood lipids. Circ. Res. 2015;117:817–824. doi: 10.1161/CIRCRESAHA.115.306807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barichella M, et al. Dietary habits and neurological features of Parkinson’s disease patients: implications for practice. Clin. Nutr. 2017;36:1054–1061. doi: 10.1016/j.clnu.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 48.Scheperjans F, et al. Gut microbiota are related to Parkinson’s disease and clinical phenotype. Mov. Disord. 2015;30:350–358. doi: 10.1002/mds.26069. [DOI] [PubMed] [Google Scholar]
- 49.Treede I, et al. Anti-inflammatory effects of phosphatidylcholine. J. Biol. Chem. 2007;282:27155–27164. doi: 10.1074/jbc.M704408200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lagace TA. Phosphatidylcholine: greasing the cholesterol transport machinery. Lipid Insights. 2015;8:65–73. doi: 10.4137/LPI.S31746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang J, Zhang X, Wang L, Yang C. High performance liquid chromatography-mass spectrometry (LC-MS) based quantitative lipidomics study of ganglioside-NANA-3 plasma to establish its association with Parkinson’s disease patients. Med. Sci. Monit. 2017;23:5345–5353. doi: 10.12659/MSM.904399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tommasino C, Marconi M, Ciarlo L, Matarrese P, Malorni W. Autophagic flux and autophagosome morphogenesis require the participation of sphingolipids. Apoptosis. 2015;20:645–657. doi: 10.1007/s10495-015-1102-8. [DOI] [PubMed] [Google Scholar]
- 53.Kiraz Y, Adan A, Kartal Yandim M, Baran Y. Major apoptotic mechanisms and genes involved in apoptosis. Tumour Biol. 2016;37:8471–8486. doi: 10.1007/s13277-016-5035-9. [DOI] [PubMed] [Google Scholar]
- 54.Gan-Or Z, et al. The p.L302P mutation in the lysosomal enzyme gene SMPD1 is a risk factor for Parkinson disease. Neurology. 2013;80:1606–1610. doi: 10.1212/WNL.0b013e31828f180e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Foo J-N, et al. Rare lysosomal enzyme gene SMPD1 variant (p.R591C) associates with Parkinson’s disease. Neurobiol. Aging. 2013;34:e13–e15. doi: 10.1016/j.neurobiolaging.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 56.Mao C-Y, et al. SMPD1 variants in Chinese Han patients with sporadic Parkinson’s disease. Parkinsonism Relat. Disord. 2017;34:59–61. doi: 10.1016/j.parkreldis.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 57.Aveldaño MI, Donnari D. Plasma phospholipid fatty acids in X-linked adrenoleukodystrophy. Clin. Chem. 1996;42:454–461. doi: 10.1093/clinchem/42.3.454. [DOI] [PubMed] [Google Scholar]
- 58.Suzuki K, et al. Neuronal and glial accumulation of alpha- and beta-synucleins in human lipidoses. Acta Neuropathol. 2007;114:481–489. doi: 10.1007/s00401-007-0264-z. [DOI] [PubMed] [Google Scholar]
- 59.Galea E, et al. Oxidative stress underlying axonal degeneration in adrenoleukodystrophy: a paradigm for multifactorial neurodegenerative diseases? Biochim. Biophys. Acta. 2012;1822:1475–1488. doi: 10.1016/j.bbadis.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 60.Xicoy H, Wieringa B, Martens GJM. The role of lipids in Parkinson’s disease. Cells. 2019;8:27. doi: 10.3390/cells8010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Euesden J, Lewis CM, O’Reilly PF. PRSice: polygenic risk score software. Bioinformatics. 2015;31:1466–1468. doi: 10.1093/bioinformatics/btu848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nalls MA, et al. Large-scale meta-analysis of genome-wide association data identifies six new risk loci for Parkinson’s disease. Nat. Genet. 2014;46:989–993. doi: 10.1038/ng.3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rhee EP, et al. A genome-wide association study of the human metabolome in a community-based cohort. Cell Metab. 2013;18:130–143. doi: 10.1016/j.cmet.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shin S-Y, et al. An atlas of genetic influences on human blood metabolites. Nat. Genet. 2014;46:543–550. doi: 10.1038/ng.2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Draisma HHM, et al. Genome-wide association study identifies novel genetic variants contributing to variation in blood metabolite levels. Nat. Commun. 2015;6:7208. doi: 10.1038/ncomms8208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kettunen J, et al. Genome-wide study for circulating metabolites identifies 62 loci and reveals novel systemic effects of LPA. Nat. Commun. 2016;7:11122. doi: 10.1038/ncomms11122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Purcell S, et al. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 2007;81:559–575. doi: 10.1086/519795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bralten J, et al. Autism spectrum disorders and autistic traits share genetics and biology. Mol. Psychiatry. 2018;23:1205–1212. doi: 10.1038/mp.2017.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nalls MA, et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 2019;18:1091–1102. doi: 10.1016/S1474-4422(19)30320-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nyholt DR. SECA: SNP effect concordance analysis using genome-wide association summary results. Bioinformatics. 2014;30:2086–2088. doi: 10.1093/bioinformatics/btu171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The code and scripts are available from the corresponding author upon reasonable request.