The COVID-19 pandemic has taken a heavy toll on the adult population.1 In the US, out of 1.4 million diagnosed with COVID-19, 154 children have died.2 In a large cohort study of 135 794 children tested for COVID-19, the infection rate was low (4%), many positive children remained asymptomatic, and if signs of illness were present, disease symptoms were typically mild. The case fatality rate in this group was 0.2%.3 In Europe, early studies showed a low fatality rate of 0.69% in children who tested positive for COVID-19, and 4% developed severe illness.4 Low mortality and morbidity rates due to COVID-19 in European children during the pandemic were confirmed by the statistical office of the European Union.5
However, despite the available evidence suggesting that the direct impact of COVID-19 on child and adolescent mortality and morbidity is somehow limited, child services suffered important indirect effects, owing mainly to discontinuities seen throughout Europe by many local health systems strained by the pandemic.6 The disruptions to care-seeking and preventive interventions in the majority of European countries, including checks for healthy children, vaccination plans, and mental disorders programs, were extensive and concerned the European pediatric societies.7 The aim of this commentary, jointly authored by the European Confederation of Primary Care Pediatricians (ECPCP) and EPA-UNEPSA, is to raise awareness of the indirect consequences caused by the pandemic on pediatric primary care practice in Europe and the risks for child health and well-being.
Indirect Impact of COVID-19 on Pediatric Primary Care Practice in Europe
European countries have seen a two-wave pattern in reported cases of COVID-19 in 2020, with a first wave during the months of March to July, followed by a second wave in late summer and autumn of the same year. The first wave caused a pronounced indirect impact on health services for children and changes in the daily practice of pediatric primary care. Considerable disruption of essential health services occurred in many countries.7, 8, 9 The measures taken by governments to contain the crisis often raised criticism from the European pediatric societies because of their frequent changes and the overall negative impact on children's physical and mental health and their education.10, 11, 12
In summer 2020, the ECPCP performed a study involving the majority of its member societies. Data from primary care pediatricians working in 17 European countries during the first wave of the COVID-19 pandemic were collected by a questionnaire, with the aim of obtaining information about the consequences of the pandemic on pediatric primary care practices in different locales and the risks for child health.13 , 14 The study showed that significant adjustments in daily pediatric practice took place during the generalized lockdown accompanying the first pandemic wave of COVID-19. Several changes in routine clinical practice were made by pediatricians to minimize the transmission of COVID-19 from patient to patient and among office staff. At the beginning of the pandemic, a serious shortage of protective equipment endangered health workers worldwide,15 particularly in ambulatory settings.16 , 17 However, 95% of European primary care pediatricians reported systematic use of personal protective clothing and face masks within a short time from the onset of the pandemic, and 92% expressed their commitment to maintaining this practice beyond its end.13
With the intent to compensate for potentially infectious encounters, in-person visits were significantly reduced and replaced with phone and, to a lesser extent, video consultations. Slightly more than one-half (55%) of primary care pediatricians reported that during the pandemic period March-August 2020, in-person consultations rates dropped by 40% to >80% compared to previous periods. However, an effort was made to continue to offer the option of pediatrician–patient encounters by applying the “ECPCP empty waiting room policy” characterized by well-planned appointment schedules, which helped minimize waiting times and discouraged unscheduled walk-in visits.13 In most European countries, primary care pediatricians followed the directions recommended by local public health departments and World Health Organization health officials and limited the number of accompanying persons during visits in private settings, such that children could be accompanied by only 1 caretaker.18 , 19 As a result, crowding of patients in waiting rooms was significantly reduced.13 Providing separate rooms and separate consulting hours for infectious and noninfectious patients was another important safety measure, although it was not possible in all circumstances.
However, the changes applied to routine practice because of the pandemic and fearful attitudes by parents caused unintended and sometimes negative consequences.13 As reported by 40% of pediatricians participating in the ECPCP study, at the beginning of the epidemic, a considerable number of patients with minor illnesses were discouraged to come to doctor's offices, which had the unintended effect of some delays in recognizing serious conditions, thereby increasing the risk of complications.13 A large proportion of the pediatricians involved in the study (86%) reported that due to the restricted access to emergency services, in many cases, family members of their patients admitted failing to report or delaying reporting to local health authorities serious health conditions or life-threatening diseases besides COVID-19 involving their children. The most commonly unreported conditions included diabetic ketoacidosis, hematologic and oncologic diseases, appendicitis, peritonitis, child abuse, severe bacterial infections (eg, urinary tract infection), meningitis, pneumonia, and acute cardiac problems.13 Similar data were reported in the US20 and Israel.21 A study involving 53 Italian diabetes centers revealed that COVID-19 significantly worsened the presentation of type 1 diabetes in children.8
Decline in Vaccinations During COVID 19
In the summer of 2020, the World Health Organization and UNICEF warned of an alarming decline in the number of children receiving life-saving vaccines worldwide.22 According to data collected in collaboration with the US Centers for Disease Control, the Sabin Vaccine Institute, and Johns Hopkins Bloomberg School of Public Health, three- quarters of the 82 countries involved in a preliminary study reported significant COVID-19–related disruptions in their immunization programs by May 2020.22
Similar alarming data were recorded by the ECPCP study, as primary care pediatricians reported a decrease in vaccination coverage in the various European countries, which ranged from 11% to >50%, in children <2 years and >2 years of age. A major obstacle to the implementation of vaccination programs reported by European pediatricians is families’ fear of leaving home during lockdown and the hesitation to vaccinate their children during the pandemic.22 , 23
Negative Iimpact of COVID 19 Lockdown on Children's Social Interactions and Well-Being
Social distancing during COVID-19 has caused a drastic upheaval in how people work and socialize. Many children have been uprooted from their places of education and care, and it may be difficult for them to understand why their routine has been disrupted. Not much is known about the long-term mental health effects of large-scale disease outbreaks on children and adolescents.24 However, monitoring young people's mental health status over the long term, and studying how prolonged school closures, strict social distancing measures, and the changes in lifestyle caused by the pandemic affect the well-being of children and adolescents would be greatly useful.24 Although during school closure parents had the chance to dedicate more valuable time to their children, in many cases COVID-19 has contributed to increased external stressors and lowered the quality of social relationships and family cohesion.25 In families that spend longer periods together, COVID-19 may exacerbate preexisting vulnerabilities, including depression and anxiety, which can harm the stability of relationships and increase the risks of abuse and violence.25 , 26 The European societies of primary care pediatrics have advised the EU public health authorities about these risks and stressed the importance of a coordinated approach by pediatricians and mental health service providers to properly manage the whole range of conditions affecting the mental well-being of children caused by the pandemic.9
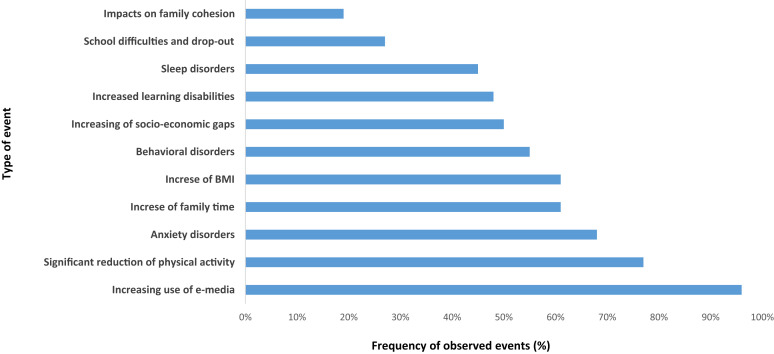
The lockdown due to COVID 19 has also exacerbated socioeconomic inequalities, including worsened educational performance of children from poor socioeconomic backgrounds, who could not be adequately supported by their parents during home schooling (Figure; available at www.jpeds.com). In Europe, 76% of ECPCP members interviewed endorsed the statement that children should go back to school to further their social development, as the benefits may outweigh the risks if all official public health requirements are observed and under the condition that adequate personal protection for the school staff could be guaranteed.
Figure.
Most frequent events observed in children and their families by European primary care pediatricians in their practices during the COVID-19 pandemic (year 2020).
Conclusions
Coordinated efforts among healthcare professionals27 will help ensure optimum health care for both sick and healthy children during the future course of the pandemic. To maintain a high quality level of pediatric primary care practice in Europe, legislators, health authorities and professional pediatric societies should collaborate closely.28 In view of the challenges posed by the pandemic, the data provided by the ECPCP suggest that it will be essential to implement a strategy aimed at preserving the continuity of preventive services and vaccination programs and focusing on the free, fearless access of all children to health services.
Footnotes
The authors declare no conflicts of interest.
Appendix
References
- 1.Koh H.K., Geller A.C., VanderWeele T.J. Deaths from COVID-19. JAMA. 2021;325:133–134. doi: 10.1001/jama.2020.25381. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics Children and COVID-19: state-level data report. https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/
- 3.Bailey L.C., Razzaghi H., Burrows E.K., Bunnell T., Camacho P.E.F., Christakis D.A., et al. Assessment of 135794 paediatric patients tested for severe acute respiratory syndrome coronavirus 2 across the United States. JAMA Pediatr. 2021;175:176–184. doi: 10.1001/jamapediatrics.2020.5052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Götzinger F., Santiago-García B., Noguera-Julián A., Lanaspa M., Lancella L., Calò Carducci F.I., et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4:653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.European Statistical Office (eurostat) COVID-19: statistics serving Europe. https://ec.europa.eu/eurostat/web/covid-19/overview
- 6.Bensoussan E., Ouldali N., Ashkenazi S., Angoulvant F., Cohen R., Levy C. Impact of coronavirus disease 2019 (COVID-19) pandemic on pediatric infectious disease research. J Pediatr. 2021;230:279–281.e2. doi: 10.1016/j.jpeds.2020.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Somekh I., Somech R., Pettoello-Mantovani M., Somekh E. Changes in routine pediatric practice in light of coronavirus 2019 (COVID-19) J Pediatr. 2020;224:190–193. doi: 10.1016/j.jpeds.2020.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rabbone I., Schiaffini R., Cherubini V., Maffeis C., Scaramuzza A. Diabetes Study Group of the Italian Society for Pediatric Endocrinology and Diabetes. Has COVID-19 delayed the diagnosis and worsened the presentation of type 1 diabetes in children? Diabetes Care. 2020;43:2870–2872. doi: 10.2337/dc20-1321. [DOI] [PubMed] [Google Scholar]
- 9.Spencer N., Nathawad R., Arpin E., Johnson S. Pandemics, epidemics and inequities in routine childhood vaccination coverage: a rapid review. BMJ Paediatr Open. 2020;4:e000842. doi: 10.1136/bmjpo-2020-000842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrara P., Franceschini G., Corsello G., Mestrovic J., Giardino I., Vural M., et al. The dark side of the web—a risk for children and adolescents challenged by isolation during the novel coronavirus 2019 pandemic. J Pediatr. 2021;228:324–325.e2. doi: 10.1016/j.jpeds.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoey H., Mestrovic J., Vural M., Baranova L.N., Somekh E., Pettoello–Mantovani M. Children facing natural, economic and public health crisis in Europe: the risks of a predictable unpredictability. Turk Pediatri Ars. 2020;55(Suppl 1):4–9. doi: 10.14744/TurkPediatriArs.2020.55553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.European Confederation of Primary Care Pediatricians How did the COVID-19 pandemic change paediatric primary care? Results of a European primary care survey. https://www.ecpcp.eu/fileadmin/pdf_doc_ppt/Data_results_of_the_PCP_survey__for_Websites_ECPCP_and_EPA-_UNEPSA.pdf
- 14.Huss G., Magendie C., Pettoello-Mantovani M., Jaeger-Roman E. The implications of the COVID-19 pandemic for pediatric primary care practice in Europe. J Pediatr. 2021 doi: 10.1016/j.jpeds.2021.03.004. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.UN News We can’t stop COVID-19 without protecting health workers: WHO chief. 2020. https://news.un.org/en/story/2020/03/1058581
- 16.American Academy of Paediatrics, AAP News AAP issues guidance to ensure continued care for children during pandemic. https://www.aappublications.org/news/2020/04/14/ambulatory041420
- 17.Walker D., Chandir S. COVID-19és lost generation of unvaccinated children. Lancet Glob Health. 2021;9:e250. doi: 10.1016/S2214-109X(20)30535-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agostiniani R., Bozzola E., Staiano A., Del Vecchio A., Mazzone T., Greco L., et al. Providing pediatric well-care and sick visits in the COVID-19 pandemic era: the recommendations of the Italian Pediatric Society. Ital J Pediatr. 2020;46:133. doi: 10.1186/s13052-020-00899-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization (WHO) Maintaining essential health services during the COVID-19 outbreak. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/related-health-issues [DOI] [PMC free article] [PubMed]
- 20.Gerall C.D., DeFazio J.R., Kahan A.M., Fan W., Fallon E.M., Middlesworth W., et al. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg. 2020 doi: 10.1016/j.jpedsurg.2020.10.008. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosenberg Danziger C., Krause I., Scheuerman O., Luder A., Yulevich A., Dalal I., et al. Pediatrician, watch out for corona-phobia. Eur J Pediatr. 2021;180:201–206. doi: 10.1007/s00431-020-03736-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization WHO and UNICEF warn of a decline in vaccinations during COVID-19. https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19
- 23.McIntosh E.D.G., Janda J., Ehrich J.H.H., Pettoello-Mantovani M., Somekh E. Vaccine hesitancy and refusal. J Pediatr. 2016;175:248–249.e1. doi: 10.1016/j.jpeds.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 24.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herbert J.S., Mitchell A., Brentnall S.J., Bird A.L. Identifying rewards over difficulties buffers the impact of time in COVID-19 lockdown for parents in Australia. Front Psychol. 2020;11:606507. doi: 10.3389/fpsyg.2020.606507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ferrara P., Caporale O., Cutrona C., Sbordone A., Amato M., Spina G., et al. Femicide and murdered women's children: which future for these children orphans of a living parent? Ital J Pediatr. 2015;41:68. doi: 10.1186/s13052-015-0173-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ehrich J.H.H., Kerbl R., Pettoello-Mantovani M., Lenton S. Opening the debate on pediatric subspecialties and specialist centers: opportunities for better care or risks of care fragmentation? J Pediatr. 2015;167:1177–1178.e2. doi: 10.1016/j.jpeds.2015.07.060. [DOI] [PubMed] [Google Scholar]
- 28.Villani A., Giuliani M., Raponi M., Ladogana S., Cristalli P., Sacco M., et al. Child healthcare services offered by the Vatican City State in its national territory and in extra-territorial neighboring Italian areas. Turk Pediatri Ars. 2020;55(Suppl 1):105–111. doi: 10.14744/TurkPediatriArs.2020.23690. [DOI] [PMC free article] [PubMed] [Google Scholar]