Abstract
Introduction:
We described our rationale and experiences with the use of cutting jigs for vertical ostectomy in cases of terminal maxillary dentition when edentulation and an additively manufactured subperiosteal jaw implant (AMSJI®) are planned.
Material and Methods:
Our experience covers 15 patients treated by four clinicians. We tabulated our criteria for planning and manufacturing vertical and horizontal ostectomy guides.
Results:
In order to guarantee accurate osteotomy, titanium guides are preferable to guides made of polymer. The most important consideration is to avoid acute angles in the buccal arms of the AMSJI®. It is up to the surgeon whether to screw-fix the ostectomy guides or to use handles to maintain their position.
Discussion:
Guided ostectomy has the potential to extend the use of AMSJI® to cases where teeth have yet to be removed or where the contours of the residual bone are not favorable. The use of guided ostectomy in such cases lessens the time between edentulation and implantation and improves the design of the implants.
Keywords: Alveolar bone loss, cutting guide, maxilla, printing, three-dimensional
INTRODUCTION
For the treatment of edentulous patients with advanced maxillary bone atrophy, we consider following options: tilted implants, bone grafting and conventional endosseous implants, zygomatic implants, and the additively manufactured subperiosteal implant (AMSJI®). The maxilla can be divided into molar, premolar, and anterior zones.[1] The quantity and quality of bone and the residual ridge morphology available for implants is checked in each zone. If the bone and ridge morphology are deficient only in the molar zone, then tilted implants can be used to avoid involvement of the maxillary sinuses, or else a sinus-floor augmentation procedure can be used. If the bone quantity and ridge morphology are deficient in the molar zone and the premolar zone, then bone grafts associated with sinus lifting or zygomatic implants with standard implants in the anterior area are indicated. Finally, when the deficiency in bone quantity and residual ridge morphology extends to the anterior zone, patients require either full-arch bone grafting associated with sinus augmentation[2] or four zygomatic implants.[3] Recently, we began using the additively manufactured subperiosteal jaw implant (AMSJI®)[4,5] for patients with advanced, Cawood and Howell[6] Class V to VIII, atrophy. The AMSJI® is a three-dimensionally (3D) printed, titanium, patient-matched, subperiosteal implant that can be applied through a minimally invasive procedure, requiring local anesthesia only. Another major advantage of the AMSJI® is that it allows for immediate masticatory, esthetic, and phonetic function.
Many patients have residual dentition in a state of advanced periodontal/endodontic disease that can no longer be used prosthetically and must be removed. In those cases, part of the alveolar bone will remain after the teeth are extracted, which over time will undergo disuse and misuse atrophy.[7,8] When the alveolus has not yet been completely resorbed, there is no immediate indication for an AMSJI®, because the main structure (Mainframe) of the subperiosteal implant leans on the alveolus, and after resorption of the alveolus, the arms of the implant become exposed, and peri-implantitis can strike.
The basal bone does not change shape significantly after edentulation, whereas the alveolus changes shape horizontally and vertically. In the anterior and posterior maxilla, bone loss occurs both vertically and horizontally from the buccal aspect.[9] Therefore, in cases where dental elements still have to be removed or were recently removed, there may still be a quantity of alveolus present. To install an AMSJI®, we would need to wait for resorption of the alveolar bone to occur, which exposes a paradoxical situation: there is not enough bone for other implant-prosthetic solutions, whereas there is not yet sufficiently advanced bone atrophy for the AMSJI® to be considered. The following protocol extends the possibility of using the AMSJI® for patients with Cawood and Howell class IV atrophy.[6]
MATERIALS AND METHODS
Ethics
The procedures followed were in accordance with the Helsinki Declaration of 1975, as revised in 2000. All patients consented to expose anonymized date from their medical records.
Setting
University Hospital, General Hospital, Private Clinics.
General protocol
Computerized tomography (CT) Digital Imaging and Communications in Medicine data were translated into stereolithographic files using Mimics Innovation Suite (Materialise, Heverlee, Belgium). Virtual edentulation was performed through different density thresholds with Geomagic Freeform Plus (3D-systems GmbH, USA) [Figure 1]. Then, the natural postextraction bone resorption process was simulated, and the bone of the virtual alveoli after resorption was gauged. A vertical ostectomy guide (VOG) was then designed using Geomagic Freeform Plus so that the part of the alveolus that would be most subject to atrophy after edentulation could be surgically reduced rather than allowed to remodel naturally over time. Studies of postextraction bone atrophy[9] showed that in the upper jaw, atrophy takes place predominantly in the centripetal direction, resulting in marked resorption of the buccal bone. Therefore, a horizontal ostectomy guide (HOG) was designed for buccal reduction. The VOG and HOG were then 3D printed in titanium alloy (SLM Solutions, Lübeck, Germany). The use of the ostectomy guides provided a way to surgically anticipate the natural postextraction bone resorption process, significantly reducing the time after edentulation that patients must wait for an AMSJI® to be installed. In some cases, simultaneous resection and reconstruction was possible. The bone that became available after the ostectomies could be grafted in defects or around the posts of the AMSJI® to simulate the well-known endosseous implant situation.
Figure 1.
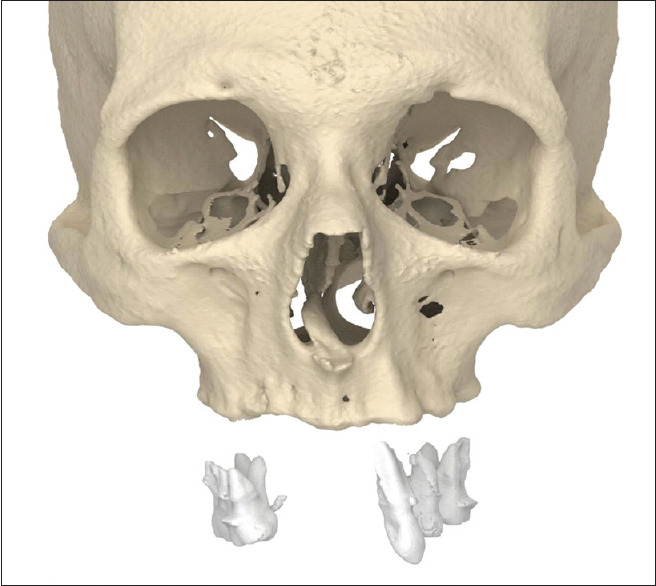
Virtual edentulation
We distinguished two different clinical situations. The first was when the alveolar bone to be resected was outside the area that supported the AMSJI®. The second was when the alveolar bone to be resected was within the area that will support the AMSJI®. The determination of which situation applied was made in the predesign phase of the AMSJI® implantation procedure and determined the timing. In the first situation, the AMSJI® could be installed at the same time that the bone was resected. In the second situation, it was sometimes possible to simultaneously remove part of the residual alveolar bone and install the AMSJI®, whereas in other cases, it was better to wait several months after the ostectomy before installing the AMSJI®. The presence of infections and the distance between the planned ostectomy and the infected area were key factors in the decision of whether to perform the ostectomy and install the AMSJI® simultaneously or consecutively. In cases, where the ostectomy could not completely eliminate the areas of infection, the procedures were performed consecutively with an intervening period for natural remodeling.
An AMSJI® was sometimes requested after a previous implant or prosthetic fails, in which case it was necessary to remove osseointegrated implants before the AMSJI® was installed. Zygomatic implants are sometimes used in the treatment of atrophic jaws, and when they fail, their removal can leave extensive bone defects in the zygomatic buttresses, which were one of the main fixation zones for the AMSJI®. In such cases, the placement of the AMSJI® was deferred until natural remodeling occurred after the previous implant was removed. When the root tips reached inside the maxillary sinuses, or the thickness of the sinus floor was reduced, we believed that it was best to wait for bone healing before installing an AMSJI®. In that case, the waiting period allowed for a more stable bone support surface and less posttraumatic remodeling after implantation. The type of anesthesia required, local or general, depended more on the psychology of the patient than on the choice between a simultaneous or consecutive approach.
Technical guidelines
Our major recommendations after experiences with 15 cases of simultaneous reductive osteotomy and AMSJI® implantation are summarized as follows:
Envision buccal mucoperiosteal flaps up to the midline with a central vertical relaxation incision [Figure 2]
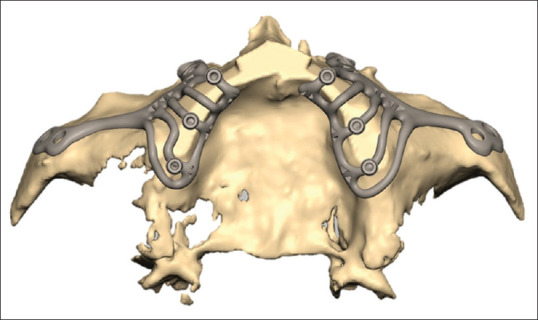
Vertical alveolar bone reduction is guided by the caudal platform of the VOG [Figure 3]
Provide two crestal support arms in the posterior zone and one under the anterior nasal spine (VOG) [Figure 4]
Leave 3 mm of bone below the maxillary sinuses (VOG) [Figure 5]
Only resect horizontally in the area where the implant arms will be designed (HOG) [Figure 6]
Avoid sharp angles in the arms [Figure 2]. Bevel the ostectomy sides (HOG)
Have the VOG and HOG made in titanium (so it is possible to hammer them in place using a punch)
Consider the design of the handle (direction, knee VOG and HOG [Figure 7]). It should not interfere with the shaft of the handpiece (reciprocating saw or piezo surgery)
The preference for screw fixation, which requires one extra hand, or a manually positioned handle, depends on the surgeon [Figures 7 and 8].
Figure 2.
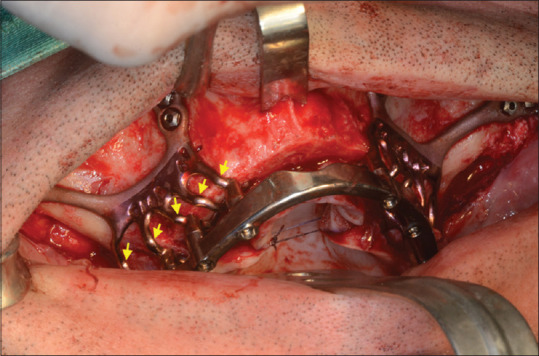
Sharp knees are to be avoided (yellow arrows)
Figure 3.
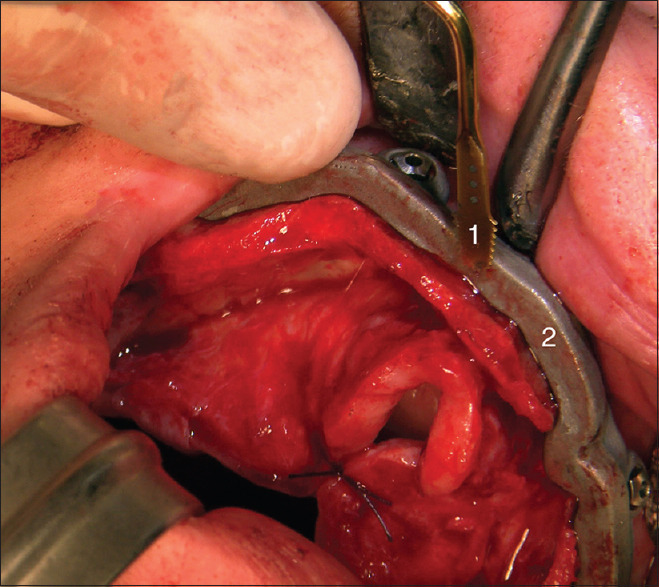
Vertical ostectomy guide, screw fixated 1. Piezoelectric blade 2. Caudal platform of the vertical ostectomy guide
Figure 4.
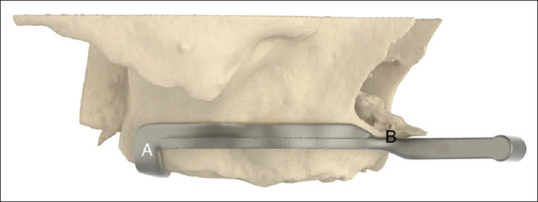
Vertical ostectomy guide with right-sided crestal arm (A) and anterior support at the anterior nasal spine (B)
Figure 5.
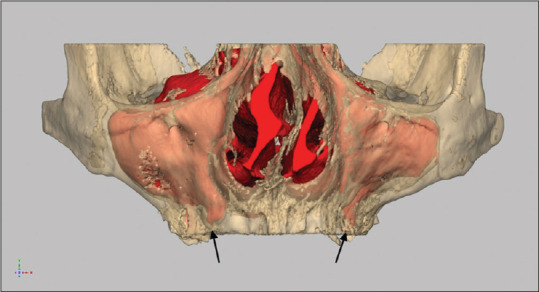
Leave minimally 3 mm of crestal bone under the alveolar maxillary sinus recess (black arrows)
Figure 6.
Horizontal resection using horizontal ostectomy guide only in areas where arms or mainframe will be located
Figure 7.
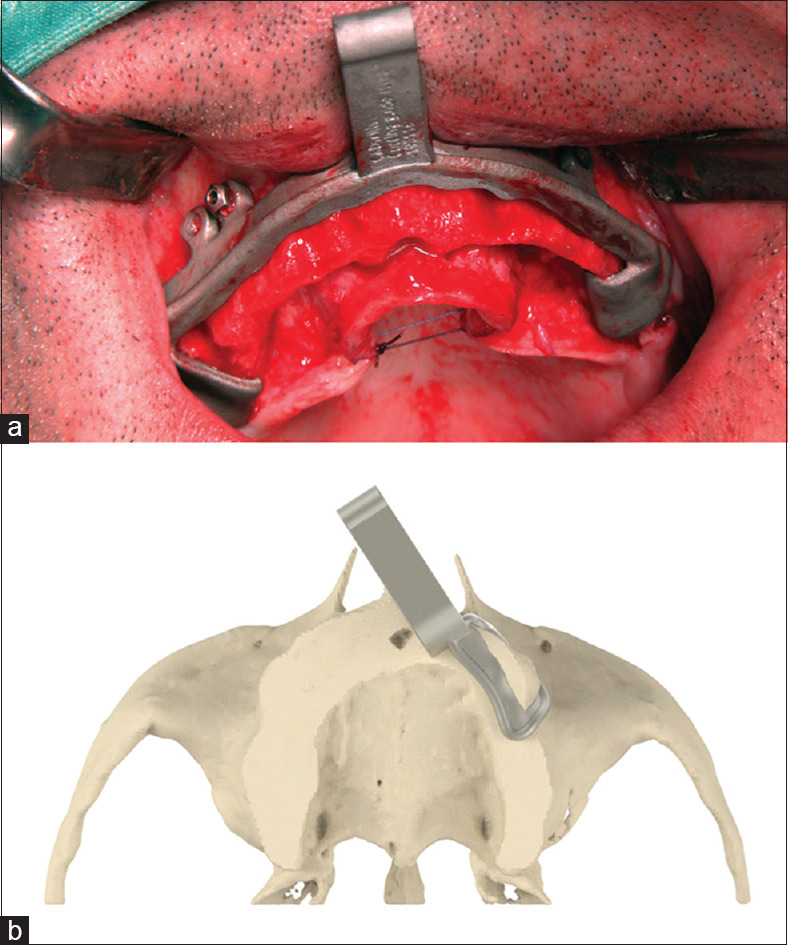
Handles freeing assisting hands (a) The anterior handle of this vertical ostectomy guide retracts the upper lip. Note the screw fixation (b) The angulated handle of this horizontal ostectomy guide does not interfere with the reciprocating saw or piezo handpiece
Figure 8.
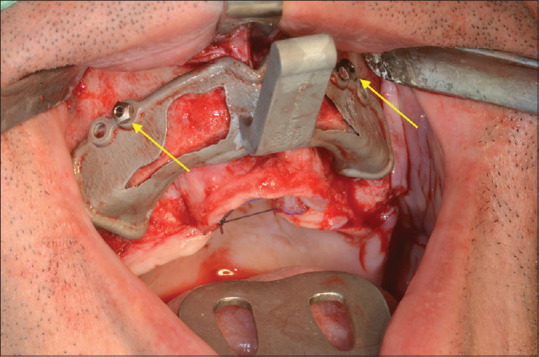
The horizontal ostectomy guide held in place by screw fixation (yellow arrow) in the same holes as the vertical ostectomy guide before
RESULTS
We performed simultaneous AMSJI® placement and dental extraction with surgical ridge reduction using VOGs and HOGs in 15 patients (8 females, 7 males; mean age 61 years) between February 2019 and March 2020. Follow-up ranged from 8 to 19 months. Two of the patients experienced exposure of a knee in one of the arms of the AMSJI® within 1 and 8 months after the AMSJI® was installed. One dehiscence closed spontaneously. In the other patient, the buccal arm was disconnected from the post, and the wound primarily closed.
DISCUSSION
The systematic review by Van der Weijden et al.[9] of dimensional changes of the alveolar bone after dental extractions indicates that resorption is very rapid in the first 6 months and subsequently continues at a very slow rate throughout life. The main bone loss occurs in the horizontal dimension, especially in the buccal part of the maxilla.[10,11,12] The bone loses more in thickness (3.87 mm) than in height (1.67–2.03 mm), causing the alveolar bone crest to move to a more palatal position.
When there are prominent roots of the front teeth under a thin buccal bone plate, the postextractive bone resorption mainly affects the buccal bone wall.[13] It has also been reported that, when teeth are present, a buccal bone plate with thickness >2 mm is predictive of greater stability of the buccal bone surface.[14] In addition, many other systemic and local factors influence the extent of postextraction bone resorption, such as smoking and the patient's overall state of health. Many candidates for AMSJI® implantation already have removable, total, or partial prostheses. The reduction of residual alveolar bone is much faster during the 1st year of removable prosthesis use[15] and much slower thereafter.
There are many types of removable prostheses. Their correct adaptation is important for the transmission of the masticatory load to the underlying bone. Skeletal prostheses (frames) are frequently connected to precision crowns on natural teeth. In those cases, it is possible to have bone resorption in the saddle areas, leaving some quantity of residual bone where the teeth are still present. Such a situation is a typical example of where it is recommended to use resection guides and remove the alveolar bone left after edentulation. Roux[16] suggested that bone loss following tooth extraction is caused by disuse atrophy. Wolff's law states that bone adapts its structure in relation to mechanical demands. According to the Utah paradigm of skeletal physiology,[7] the state of bone adaptation between disuse and overload is maintained with a range of forces between 1000 and 1500 microstrain.[17] Rubin et al.[18] observed that the maximum bone strains measured in various animal species were between 2000 and 3500 microstrain, corresponding to bone remodeling. Those strains are about 50% of the yield strain of cortical bone, indicating that nature applies a safety factor of two. To avoid stress shielding due to incorrect distribution of forces, the AMSJI® structure must be perfectly adherent to the underlying bone so that it is maintained in a state of adaptation. Finite element analysis determines the necessary resiliency of the AMSJI® structure.
The scan prosthesis should represent the fixed prosthesis of the supporting titanium structure that will be manufactured together with the AMSJI®. A duplicate of the existing removable prosthesis does not always provide a good representation for the design of the new fixed prosthesis. If there is residual dentition in the molar or premolar zones, a partial scan prosthesis is made using a wax-up of the front teeth, and the new dental arch is designed, keeping the molar and premolar zones as a reference for a the new 3D-printed provisional prosthesis, but with improved aesthetics and positioning in the anterior zone. In that way, the choice between a hybrid or double structure and a Dolder bar-retained prosthesis can be made on the basis of access for personal hygiene. A double structure with removable denture might better support the lip and allow easier cleaning. If the existing frontal dentition can be considered the future ideal situation, a partial scan prosthesis is made using a wax-up in the premolar and molar zones. If the residual dentition in all zones is deficient, all teeth are removed virtually from an optical scan or manually from a gypsum model, and an ideal dental arch is made as a wax-up. Optical scans of the gypsum model containing the teeth to be removed and the model with the wax-up dental arch are used to overlap with the dentition visualized in the CT scan of the patient.[19] The new ideal dental situation is then related to the bony structures using the design software. A totally digital approach would even be possible using facial scanners and digital smile design.
We found that the bone morphology after osteotomy with a VOG influenced some of the design details of the prosthetic mainframe. In the design of the postposition (prosthetic connections), the teeth in the scan prosthesis are often not positioned exactly in the center of the bony crest. If an osteotomy is performed, the bone surface becomes flat, and consequently, the structure designed to connect the post to the rest of the prosthesis is liable to form sharp corners that can cause soft tissue dehiscence. That happens especially if the posts are not in the center of the alveolar ridge. To overcome that problem, we prefer to use a HOG to create a more rounded bone profile and to place the posts in the center of the newly shaped alveolar crest.
The limitations of this technical note are that numerical data on outcome are not provided. Long-term bony regrowth or further resorption may create complications. A prospective radiological follow-up study with a 15-year span will not be feasible.
CONCLUSIONS
The use of ostectomy guides has the potential to extend the use of the AMSJI® to all cases in which there are still teeth to be removed, or where there are bony ridges yet to be resorbed. The shape of the bone after ostectomy directly influences the design of the AMSJI®. Therefore, it is important to avoid sharp corners in the implant structure using a HOG. Sharp corners can cause soft-tissue dehiscence over time. This approach can be used to reduce the time and invasiveness of the rehabilitation treatment and also to adapt the morphology of the bone, if it is not favorable, to the needs of the AMSJI®.
Financial support and sponsorship
Nil.
Conflicts of interest
Dr. Mommaerts is innovation ambassador and co-owner of the CADskills bv company.
Acknowledgments
The authors are indebted to Mr. Benoit de Smet, AMSJI® product manager at CADskills bv, for his invaluable help in the design iterations.
REFERENCES
- 1.Bedrossian E, Bedrossian EA. Systematic treatment planning protocol of the edentulous maxilla for an implant-supported fixed prosthesis. Compend Contin Educ Dent. 2019;40:20–5. [PubMed] [Google Scholar]
- 2.Neyt LF, De Clercq CA, Abeloos JV, Mommaerts MY. Reconstruction of the severely resorbed maxilla with a combination of sinus augmentation, onlay bone grafting, and implants. J Oral Maxillofac Surg. 1997;55:1397–401. doi: 10.1016/s0278-2391(97)90636-4. [DOI] [PubMed] [Google Scholar]
- 3.Davó R, David L. Quad Zygoma: Technique and Realities. Oral Maxillofac Surg Clin North Am. 2019;31:285–97. doi: 10.1016/j.coms.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Mommaerts MY. Additively manufactured sub-periosteal jaw implants. Int J Oral Maxillofac Surg. 2017;46:938–40. doi: 10.1016/j.ijom.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Mommaerts MY. Evolutionary steps in the design and biofunctionalization of the additively manufactured sub-periosteal jaw implant 'AMSJI' for the maxilla. Int J Oral Maxillofac Surg. 2019;48:108–14. doi: 10.1016/j.ijom.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17:232–6. doi: 10.1016/s0901-5027(88)80047-x. [DOI] [PubMed] [Google Scholar]
- 7.Frost HM. The Utah paradigm of skeletal physiology: An overview of its insights for bone, cartilage and collagenous tissue organs. J Bone Mineral Metab. 2000;18:305–16. doi: 10.1007/s007740070001. [DOI] [PubMed] [Google Scholar]
- 8.Carpenter RD, Carter DR. The mechanobiological effects of periosteal surface loads. Biomecham Model Mecanobiol. 2008;7:227–42. doi: 10.1007/s10237-007-0087-9. [DOI] [PubMed] [Google Scholar]
- 9.Van der Weijden F, Dell'Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J Clin Periodontol. 2009;36:1048–58. doi: 10.1111/j.1600-051X.2009.01482.x. [DOI] [PubMed] [Google Scholar]
- 10.Lekovic V, Kenney EB, Weinlaender M, Han T, Klokkevold P, Nedic M, et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction.Report of 10 cases. J Periodontol. 1997;68:563–70. doi: 10.1902/jop.1997.68.6.563. [DOI] [PubMed] [Google Scholar]
- 11.Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, et al. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol. 1998;69:1044–9. doi: 10.1902/jop.1998.69.9.1044. [DOI] [PubMed] [Google Scholar]
- 12.Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction.An experimental study in the dog. J Clin Periodontol. 2005;32:212–8. doi: 10.1111/j.1600-051X.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 13.Nevins M, Camelo M, De Paoli S, Friedland B, Schenk RK, Parma-Benfenati S, et al. A study of the fate of the buccal wall of extraction sockets of teeth with prominent roots. Int J Periodontics Restorative Dent. 2006;26:19–29. [PubMed] [Google Scholar]
- 14.Huynh-Ba G, Pjetursson BE, Sanz M, Cecchinato D, Ferrus J, Lindhe J, et al. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implants Res. 2010;21:37–42. doi: 10.1111/j.1600-0501.2009.01870.x. [DOI] [PubMed] [Google Scholar]
- 15.Antje T. The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years. J Prosthet Dent. 1972;27:120–32. doi: 10.1016/0022-3913(72)90188-6. [DOI] [PubMed] [Google Scholar]
- 16.Roux W. Der Kampf der Teile im Organismus.Ein Beitrag zur Vervollstandigung der Mechanischen Zweckmassigkeitslehre. Leipzig: Verlag von Wilhem Engelmann; 1881. [Google Scholar]
- 17.Hansson S, Halldin A. Alveolar ridge resorption after tooth extraction: A consequence of a fundamental principle of bone physiology. J Dent Biomech. 2012;3:1–8. doi: 10.1177/1758736012456543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rubin CT, Sommerfeldt DW, Judex S, Qin YX. Inhibition of osteopenia by low magnitude, High-frequency mechanical stimuli. Drug Discov Today. 2001;6:848–58. doi: 10.1016/s1359-6446(01)01872-4. [DOI] [PubMed] [Google Scholar]
- 19.Cantoni T, Giovanni P. Implant treatment planning in fresh extraction sockets: Use of a novel radiographic guide and CAD/CAM technology. Quintessence Int. 2009;40:773–81. [PubMed] [Google Scholar]


