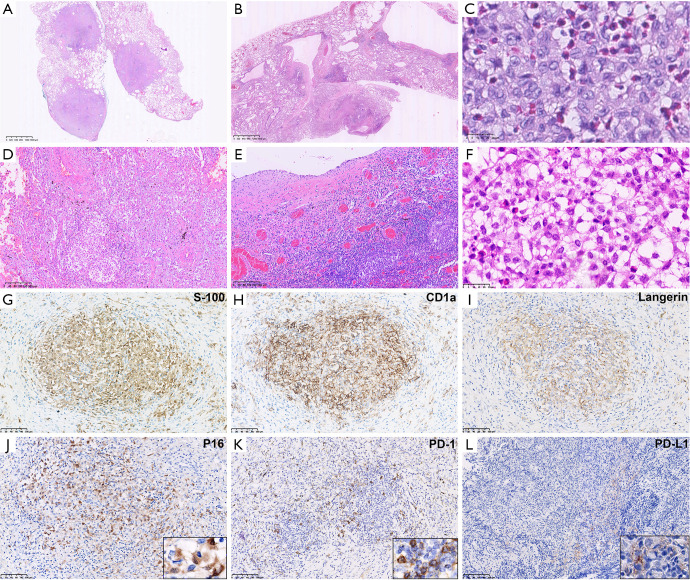
Figure 2.
Microscopic pathological features of Adult PLCHs. Adult PLCHs showed either nodular Roche automatic immunohistochemical staining (A) or cystic lesions (B) at low magnification (HE, magnification ×12.5). Commonly, Langerhans cells clustered around the bronchioles and destroyed the bronchial wall, but were recognized by presence of small artery. In the cystic lesions, Langerhans cells accumulated in the walls of variable-sized cysts. (C) High magnification revealed Langerhans cells with unclear cell boundaries, irregular nuclear membranes, visible furrows, and moderate amounts of slightly eosinophilic cytoplasm (HE, magnification ×800). The extrapulmonary recidivism group presented more significant interstitial fibrosis either in nodular (D) or cystic (E) (HE, magnification ×100), combined with infiltration by numerous eosinophils, lymphocytes, and plasma cells. (F) Extrapulmonary involvement was demonstrated by rib invasion presenting with infiltration of Langerhans cells between trabeculae (HE, magnification ×100). Traditional diagnostic markers, S100, langerin, and CD1a were positive in all 6 cases, which confirmed the diagnosis (EnVision, G,H,I, magnification ×200). (J) P16 was overexpressed in Langerhans cells with a cytoplasm positive pattern (EnVision, magnification ×200). Adult PLCH was found to have high PD-1 (K) expression in tumor immune cells and low PD-L1 (L) expression in Langerhans cells (EnVision, magnification ×200). PLCH, pulmonary Langerhans cell histiocytosis; PD-1, programmed cell death 1; PD-L1, programmed cell death-ligand 1.