Abstract
Cerebral venous thrombosis (CVT) is a rare clinical entity, with clinical presentations extending from headache and seizures to coma and death. For adults developing progressive neurological worsening despite adequate medical management, endovascular thrombolysis and/or mechanical thrombectomy may be considered as treatment options. We present one such patient with CVT who developed seizures and slipped into a coma, despite best medical management. A large-bore aspiration catheter was used as a standalone system for the endovascular procedure. The venous sinuses were successfully re-canalized. The patient was discharged a week later with a modified Rankin scale of 2. Studies show that endovascular thrombolysis used alone or in conjunction with thrombectomy for CVT has a higher risk of hemorrhagic complications. If we were to use mechanical thrombectomy devices (that are specifically designed for intracranial clot retrieval) as a stand-alone system, we would probably have better clinical outcomes with a lower risk of hemorrhagic complications.
Keywords: Cerebral veins, Thrombectomy, Stroke, Brain venous infarction
INTRODUCTION
Cerebral venous thrombosis (CVT) is a rare clinical entity and accounts for <1% of all strokes, with a wide array of clinical presentations from headache and seizures to coma and death [1-3]. For adults who develop progressive neurological worsening despite adequate medical management, endovascular thrombolysis and/or mechanical thrombectomy may be considered as treatment options [4]. When patients present with hemorrhagic venous infarcts, the treating physicians are often apprehensive to use endovascular thrombolytic agents, and there is limited evidence available about its effectiveness in such cases. We faced a similar dilemma, and we decided to use a large-bore aspiration catheter as a standalone system to successfully recanalize the cerebral venous system, which in turn resulted in a significant clinical improvement.
CASE REPORT
A patient in his late 30s presented to our institution with complaints of a recent headache. The headache had worsened and was severe at the time of presentation. He was coherent and had left-sided hemiparesis. We also noted bilateral papilledema. He underwent a computerized tomography scan which revealed hyperdensity along the right transverse and sigmoid sinuses. A provisional diagnosis of cerebral venous thrombosis was considered. The patient was admitted to the intensive care unit and was started on low molecular weight heparin. The following day, the patient developed focal seizures involving his left upper and lower limbs which progressed to epilepsia partialis continua. His sensorium started to deteriorate, and he was finally intubated, sedated, and paralyzed. Magnetic resonance imaging (MRI) of his brain revealed a bilateral venous infarct with hemorrhagic transformation and extensive thrombosis of superior sagittal sinus, inferior sagittal sinus, straight sinus, bilateral transverse sinus, right sigmoid sinus, and right internal jugular vein (Fig. 1 A, B). Since the patient was deteriorating despite best medical management, endovascular intervention was offered and informed consent was obtained.
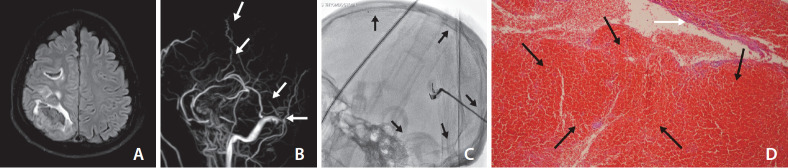
Fig. 1.
(A) Magnetic resonance imaging brain T2 FLAIR images showing hemorrhagic venous infarct in the right cerebral hemispheres. (B) Magnetic resonance imaging venogram shows non visualization (white arrows) of major sinus conduits. (C) Aspiration catheter (black arrows) in the venous system. (D) Photomicrograph of blood clot showed predominantly red blood cells (black arrows) and very little fibrin (white arrow).
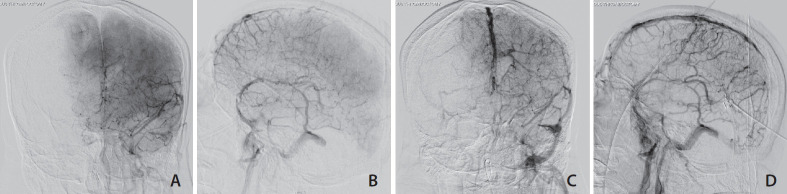
Right femoral arterial access was obtained and a guiding catheter was placed in the left internal carotid artery with a constant heparinized saline flush. This system was used to acquire roadmaps, wherein the acquisition was continued until we could see the venous drainage. A 7 French short sheath was introduced into the left internal jugular vein under ultrasound guidance. Through this, a REACT 71 aspiration catheter (6.5 Fr, length 132 cm; Medtronic, Irvine, CA, USA) was introduced over a Phenom 21 microcatheter (0.021 inner diameter, 150 cm; Medtronic) and Avigo microwire (0.014 diameter, 205 cm; Medtronic) system (Fig. 1C). The catheter was slowly guided into the left and right transverse sinus, straight sinus, and inferior and superior sagittal sinuses. Aspiration thrombectomy was performed multiple times until recanalization was visible (Fig. 2A-D). The venous clots that were aspirated were red blood cell-rich clots (Fig. 1D). Both puncture sites were closed by manual compression. The patient was continued on low molecular weight heparin. The following day, the patient’s seizures had stopped. He was slowly weaned off the ventilator and extubated. Seven days from mechanical thrombectomy, the patient was discharged with residual hemiparesis on the left side and a modified Rankin Score of 2. Extensive investigations for prothrombotic states including anti-nuclear antibody profile, antiphospholipid antibody tests, and screening for protein C, protein S, or antithrombin III deficiencies were negative. His homocysteine levels were normal. He was discharged with oral anticoagulants.
Fig. 2.
Pre (A, B) and post (C, D) venous mechanical thrombectomy.
DISCUSSION
CVT is an uncommon cause of stroke. According to the international study on cerebral vein and dural sinus thrombosis, despite best medical management 13.6% of patients still have bad outcomes with a mortality rate of 8.3% after an average follow-up of 16 months [5]. In such patients, endovascular therapy could be offered as a treatment option. The major indications for endovascular therapy in CVT include a) clinical deterioration or progression of intracerebral hemorrhage/venous infarction despite anticoagulation, b) severe stupor, comatose presentation, c) deep CVT, d) posterior fossa involvement, and e) major contraindication to anticoagulation such as bleeding disorders, thrombocytopenia (<100×109/L) or recent gastrointestinal hemorrhages [6]. Recently, a group of authors classified the configuration of CVT into 4 types: a) Type A: partial thrombosis of a sinus, b) Type B: complete thrombosis of the sinus without cortical vein involvement, c) Type C: cortical vein thrombosis only, and d) Type D: complete thrombosis of the sinus with cortical vein involvement [7]. Applying this classification, our patient had a Type D configuration CVT. According to this study, Type D patients have greater disease severity and poorer outcomes and mortality in the acute phase. Endovascular treatment as a salvage treatment was recommended for these patients [7]. When endovascular therapy is considered for CVT, 3 major treatment approaches have been followed: a) mechanical thrombectomy (using distal access catheter, thrombectomy devices, stent retrievers, or balloons), b) intravascular thrombolysis, or c) a combination of both. Studies indicate that endovascular treatment with thrombolytic agents has little benefit with an increased risk of hemorrhagic complications [8-10]. However when mechanical thrombectomy is used as the primary treatment modality for complicated CVT, the risk of hemorrhagic complications is lower, but with lower recanalization rates [11].
While it has been suggested that mechanical thrombectomy therapies may be superior to on-site thrombolytic therapy due to decreased risk of iatrogenic hemorrhage, the choice of mechanical thrombectomy method remains unclear. Stent retriever thrombectomy devices for treatment of CVT were first described by Froehler [12] in 2013. Although there are newer stent retrievers that are available for acute ischemic stroke, the use of these devices for CVT has not significantly affected outcomes or complete recanalization rates [13]. For diffuse CVT involving venous channels of different diameters, with varying lengths of occlusion, stent retrievers would not be an ideal device for thrombectomy [7]. In addition, deploying stent retrievers across each of the occluded sinuses, at various distances, and then retrieving them would significantly increase the intraoperative procedure time. Balloon angioplasty with or without stent deployment has also been tried in CVT, but then again there is very little literature in support of this method [14,15]. Balloon angioplasty would be helpful in disrupting clots, but would still require a distal aspiration system to assist thrombectomy.
Aspiration catheters have been successfully used for the treatment of CVT in the past. But there has been difficulty in tracking these devices up into the sinuses due to steep angles at various junctions [16]. In such instances, a stent retriever or a balloon can play the role of an anchor to assist in navigating these devices into the sinuses [16-18]. But the aspiration catheters used in these cases were older generation reperfusion catheters. Newer generation reperfusion catheters, with a larger inner diameter and better conformability have since then been used for acute ischemic stroke treatment (Table 1). However, their use in CVT has not yet been explored.
Table 1.
Comparison of various intracranial aspiration thrombectomy catheters
| Product name (company) | Length (cm) | Proximal OD (inch) | Distal OD (inch) | Distal ID (inch) |
|---|---|---|---|---|
| 5 max Reperfusion Catheter (Penumbra) | 132 | 0.080 | 0.065 | 0.054 |
| ACE 64 (Penumbra) | 132 | 0.080 | 0.075 | 0.064 |
| ACE 68 (Penumbra) | 132 | 0.080 | 0.080 | 0.068 |
| Jet 7 (Penumbra) | 132 | 0.085 | 0.075 | 0.072 |
| ARC (Medtronic) | 132 | 0.080 | 0.069 | 0.061 |
| Catalyst 6 (Stryker) | 132 | 0.079 | 0.071 | 0.060 |
| Catalyst 7 (Stryker) | 125/132 | 0.0825 | 0.082 | 0.068 |
| Sofia (Microvention) | 125 | 0.068 | 0.068 | 0.055 |
| Sofia Plus (Microvention) | 125/131 | 0.083 | 0.082 | 0.070 |
| React 68 (Medtronic) | 132 | 0.083 | 0.083 | 0.068 |
| React 71 (Medtronic) | 132 | 0.085 | 0.085 | 0.071 |
OD, outer diameter; ID, inner diameter.
Taking the above factors into consideration, we decided to use a larger aspiration catheter system that was specifically designed for intracranial thrombectomy (REACT 71 aspiration catheter 6.5 Fr, length 132 cm; Medtronic). REACT 71 has a large inner diameter of 0.071 inches and is the only aspiration catheter that is reinforced with nitinol coils and braids both in proximal and distal shafts (implying better conformability and trackability). We decided not to use thrombolytic agents, in view of the hemorrhagic nature of the patient’s venous infarct. This intervention resulted in recanalization of the veins as mentioned above. With regards to the catheter insertion site, we decided to puncture the jugular vein directly and introduce a short sheath. Various studies have previously indicated that the risk of catheter-related thrombosis is higher in the femoral venous system when compared with the jugular venous system [19-21]. This also resulted in reducing the distance from the sheath to the target and thereby eliminated the need for a longer catheter/sheath system.
To the best of our knowledge, this is the first case report describing the REACT 71 aspiration catheter being used in the treatment of cerebral vein thrombosis. More controlled studies analyzing the benefits of intracranial aspiration catheter devices as a standalone therapy for complicated CVTs are needed.
Footnotes
Fund
None.
Ethics Statement
Compliant with HIPAA guidelines.
Conflicts of Interest
The authors have no conflicts to disclose.
Author Contribution
Concept and design: KS. Analysis and interpretation: SP. Data collection: HH. Writing the article: JS. Critical revision of the article: SRC. Final approval of the article: SKP. Overall responsibility: KS.
REFERENCES
- 1.Cantú C, Barinagarrementeria F. Cerebral venous thrombosis associated with pregnancy and puerperium. Review of 67 cases. Stroke. 1993;24:1880–1884. doi: 10.1161/01.str.24.12.1880. [DOI] [PubMed] [Google Scholar]
- 2.Daif A, Awada A, al-Rajeh S, Abduljabbar M, al Tahan AR, Obeid T, et al. Cerebral venous thrombosis in adults. A study of 40 cases from Saudi Arabia. Stroke. 1995;26:1193–1195. doi: 10.1161/01.str.26.7.1193. [DOI] [PubMed] [Google Scholar]
- 3.Kashyap AS, Anand KP, Kashyap S. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005;353:314–315. [PubMed] [Google Scholar]
- 4.Ferro JM, Canhão P. Cerebral venous thrombosis: treatment and prognosis [Internet] Waltham: Uptodate [cited 2020 Jul 9]. Available from: https://www.uptodate.com/contents/cerebral-venous-thrombosis-treatment-and-prognosis?search=cvt&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2#H9. [Google Scholar]
- 5.Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F, ISCVT Investigators Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT) Stroke. 2004;35:664–670. doi: 10.1161/01.STR.0000117571.76197.26. [DOI] [PubMed] [Google Scholar]
- 6.Lee SK, Mokin M, Hetts SW, Fifi JT, Bousser MG, Fraser JF, Society of NeuroInterventional Surgery Current endovascular strategies for cerebral venous thrombosis: report of the SNIS Standards and Guidelines Committee. J Neurointerv Surg. 2018;10:803–810. doi: 10.1136/neurintsurg-2018-013973. [DOI] [PubMed] [Google Scholar]
- 7.Liao CH, Liao NC, Chen WH, Chen HC, Shen CC, Yang SF, et al. Endovascular mechanical thrombectomy and on-site chemical thrombolysis for severe cerebral venous sinus thrombosis. Sci Rep. 2020;10:4937. doi: 10.1038/s41598-020-61884-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coutinho JM, Ferro JM, Zuurbier SM, Mink MS, Canhão P, Crassard I, et al. Thrombolysis or anticoagulation for cerebral venous thrombosis: rationale and design of the TO-ACT trial. Int J Stroke. 2013;8:135–140. doi: 10.1111/j.1747-4949.2011.00753.x. [DOI] [PubMed] [Google Scholar]
- 9.Dentali F, Squizzato A, Gianni M, De Lodovici ML, Venco A, Paciaroni M, et al. Safety of thrombolysis in cerebral venous thrombosis. A systematic review of the literature. Thromb Haemost. 2010;104:1055–1062. doi: 10.1160/TH10-05-0311. [DOI] [PubMed] [Google Scholar]
- 10.Stam J, Majoie CB, van Delden OM, van Lienden KP, Reekers JA. Endovascular thrombectomy and thrombolysis for severe cerebral sinus thrombosis: a prospective study. Stroke. 2008;39:1487–1490. doi: 10.1161/STROKEAHA.107.502658. [DOI] [PubMed] [Google Scholar]
- 11.Siddiqui FM, Dandapat S, Banerjee C, Zuurbier SM, Johnson M, Stam J, et al. Mechanical thrombectomy in cerebral venous thrombosis: systematic review of 185 cases. Stroke. 2015;46:1263–1268. doi: 10.1161/STROKEAHA.114.007465. [DOI] [PubMed] [Google Scholar]
- 12.Froehler MT. Successful treatment of cerebral venous sinus thrombosis with the Solitaire FR thrombectomy device. J Neurointerv Surg. 2013;5:e45. doi: 10.1136/neurintsurg-2012-010517. [DOI] [PubMed] [Google Scholar]
- 13.Ilyas A, Chen CJ, Raper DM, Ding D, Buell T, Mastorakos P, et al. Endovascular mechanical thrombectomy for cerebral venous sinus thrombosis: a systematic review. J Neurointerv Surg. 2017;9:1086–1092. doi: 10.1136/neurintsurg-2016-012938. [DOI] [PubMed] [Google Scholar]
- 14.Chaloupka JC, Mangla S, Huddle DC. Use of mechanical thrombolysis via microballoon percutaneous transluminal angioplasty for the treatment of acute dural sinus thrombosis: case presentation and technical report. Neurosurgery. 1999;45:650–656. doi: 10.1097/00006123-199909000-00045. [DOI] [PubMed] [Google Scholar]
- 15.Hirata E, Higashi T, Iwamuro Y, Watanabe Y, Ando M, Arakawa Y, et al. Angioplasty and stent deployment in acute sinus thrombosis following endovascular treatment of dural arteriovenous fistulae. J Clin Neurosci. 2009;16:725–727. doi: 10.1016/j.jocn.2008.07.071. [DOI] [PubMed] [Google Scholar]
- 16.Taniguchi S, Harada K, Kajihara M, Fukuyama K. Combined use of stent-retriever and aspiration thrombectomy for cerebral venous sinus thrombosis involving the straight sinus: a case report. Interv Neuroradiol. 2017;23:605–608. doi: 10.1177/1591019917730335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bando T, Kuramoto Y, Shinoda N, Hori S, Mikami K, Shimo D, et al. Two cases of cerebral venous sinus thrombosis successfully recanalized by the concomitant use of an aspiration through the guiding catheter and stent thrombectomy device. J Neuroendovascular Ther. 2018;12:43–51. [Google Scholar]
- 18.Mascitelli JR, Pain M, Zarzour HK, Baxter P, Ghatan S, Mocco J, et al. Sinus thrombectomy for purulent cerebral venous sinus thrombosis utilizing a novel combination of the Trevo stent retriever and the Penumbra ACE aspiration catheter: the stent anchor with mobile aspiration technique. BMJ Case Rep. 2015;2015:bcr2015011782. doi: 10.1136/bcr-2015-011782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rajasekhar A, Streiff MB. How I treat central venous access device-related upper extremity deep vein thrombosis. Blood. 2017;129:2727–2736. doi: 10.1182/blood-2016-08-693671. [DOI] [PubMed] [Google Scholar]
- 20.Parienti JJ, Mongardon N, Megarbane B. Intravascular complications of central venous catheterization by insertion site. J Vasc Surg. 2016;63:846. doi: 10.1056/NEJMoa1500964. [DOI] [PubMed] [Google Scholar]
- 21.Wall C, Moore J, Thachil J. Catheter-related thrombosis: a practical approach. J Intensive Care Soc. 2016;17:160–167. doi: 10.1177/1751143715618683. [DOI] [PMC free article] [PubMed] [Google Scholar]