Abstract
Many treatments have been described for pilonidal disease, but recurrence cannot be completely eliminated. The aim of this study was to perform a meta‐analysis of randomised, controlled trials comparing flap repair vs the laying open technique and/or excision and direct closure techniques in the treatment of chronic pilonidal sinus disease. The primary outcome measure was the recurrence rate. Secondary outcomes were complete wound‐healing time, duration of the incapacity to work, quality of life and patient satisfaction, postoperative pain, wound infection, bleeding or haematoma, skin wound complications, and duration of hospital stay. Seventeen studies were included. The meta‐analysis demonstrated a lower risk of recurrence, a shorter duration of incapacity to work, a lower risk of wound infections, a lower risk of skin wound complications, and a shorter duration of hospitalisation in favour of flap vs direct closure. A shorter time to complete wound healing and a shorter duration of incapacity to work for flap vs the laying open technique were observed.
Superiority of flap repair vs direct closure in pilonidal sinus treatment was demonstrated in this meta‐analysis. These results suggest avoiding primary direct closure in clinical practice. Compared with the laying open technique, flaps result in faster healing and a shorter time to return to activities.
Keywords: direct suture, laying open technique, meta‐analysis, piloninal sinus, surgical flaps
1. INTRODUCTION
Pilonidal sinus is an acquired condition that mainly affects young people. The concept of an acquired disease was developed by Patey and Scarff not long after the Second World War on the basis of the high incidence of recurrences and the sporadic onset of the disease in other areas of the body (inter‐digital folds in the barber's hand).1, 2, 3, 4 During the Second World War, the disease gained significant importance because it occurred in many soldiers, nicknamed the “Jeep disease”.5 The main morbidity is frequent and disabling sinus infections that lead to severe pain and purulent discharge in healthy patients with an active professional life. Many eradication treatments have been described, ranging from open excision,6 de‐roofing,7, 8 marsupialisation,5, 9 and phenolisation10, 11, 12, 13 to excision and primary suture techniques and either median direct suture14, 15 or reconstruction of loss substances by local flaps.16, 17, 18, 19, 20, 21, 22, 23, 24 However, no procedure can completely eradicate it. Laying open and direct suture are common surgical strategies used. They allow complete excision of the sinus, are easy to perform, and do not require special surgical training. The use of flap repair after the excision of pilonidal sinus has increased in recent decades. This makes it possible to place the suture outside the median line, the focus of the disease. This is particularly useful in cases of multi‐recurrent and multi‐fistular diseases. Nonetheless, it requires training in plastic and reconstructive surgery procedures.
Well‐conducted, randomised, controlled, prospective studies comparing different techniques for this pathology are rare.25, 26, 27, 28 However, they are essential for the surgeon to make a decision on how to treat the disease, the primary aim being to avoid recurrence and generate the least possible perioperative morbidity.
The aim of this study was to perform a meta‐analysis of published, randomised, controlled trials comparing flap repair after pilonidal sinus excision vs the laying open technique with secondary healing or vs median direct closure techniques in patients suffering from chronic pilonidal sinus disease.
2. METHODS
2.1. Search strategy
Two independent reviewers (C.B. and B.C.) conducted a systematic review of related articles in the PubMed, Cochrane Library, and EMBASE databases. The reviewed articles were published between November 1998 and February 2018. The following association of keywords was used: “pilonidal” or “pilonidal disease” or “pilonidal sinus” or “pilonidal cyst” or “sacrococcygeal disease” with “flap” or “reconstruction” and with “randomised.”
We also did a manual search using citations from trials that were included and reviewed similar articles. There was no restriction regarding the countries in which the trial was performed. We also searched for ongoing trials using clinicaltrials.gov and the CenterWatch Clinical Trials listing service. The online search was supplemented with the bibliographies of identified articles to retrieve any other relevant published material.
2.2. Inclusion criteria
Study selection was based on an initial screen of titles and abstracts, followed by a further screening of full texts. Eligible studies were English‐language randomised controlled studies comparing flap reconstruction vs the laying open technique and/or direct closure for the treatment of chronic pilonidal sinus, with de novo and/or recurrent presentation, in patients aged 14 years or older. We excluded non‐randomised studies, retrospective studies, studies concerning pilonidal abscess, and those on the paediatric population. Studies were included if they provided data on the recurrence rate (the primary endpoint of the meta‐analysis).
We excluded studies that compared one type of flap or procedure vs another.
Descriptive data including study features (methods, participants, interventions, outcomes) and data on primary or secondary outcomes were then extracted independently. If original data were missing, we contacted the authors by email (twice). Reviewers' discrepancies were resolved after discussion and reaching consensus with the methodologist (E.B.).
2.3. Outcome measures
The primary outcome measure was the recurrence rate. It was defined as the reappearance of symptoms after complete healing and an asymptomatic period. Secondary outcome measures were complete wound‐healing time, duration of the incapacity to work, quality of life and/or patient satisfaction, postoperative pain, wound infection, bleeding or haematoma, skin wound complications, and duration of hospital stay. Wound‐healing time was defined as the period of complete epidermisation with the stopping of wound care in case of an open excision and time for the removal of stitches in case of direct closure or flap repair. The duration of the incapacity to work was expressed in postoperative days and corresponds to the time to return to work. Skin wound complications included any disruption of sutures and total or partial skin necrosis.
2.4. Data extraction and quality assessment
Data extraction was performed using a standard data collection form. These data included: age and gender distribution, number of patient included in each group, number of losses to follow up, inclusion and exclusion criteria, primary and secondary endpoints, type of flap used, and follow‐up data. For the subgroup analysis, Limberg flap, Z‐plasty, Y‐Y advancement, and rotation flap were considered transposition flaps, whereas the Karydakis flap was considered an advancement flap.
The risk of bias of the studies that were included was scored using the Review Manager programme (Rev Manager 5.3) according the Cochrane tool (Figure 1).
Figure 1.
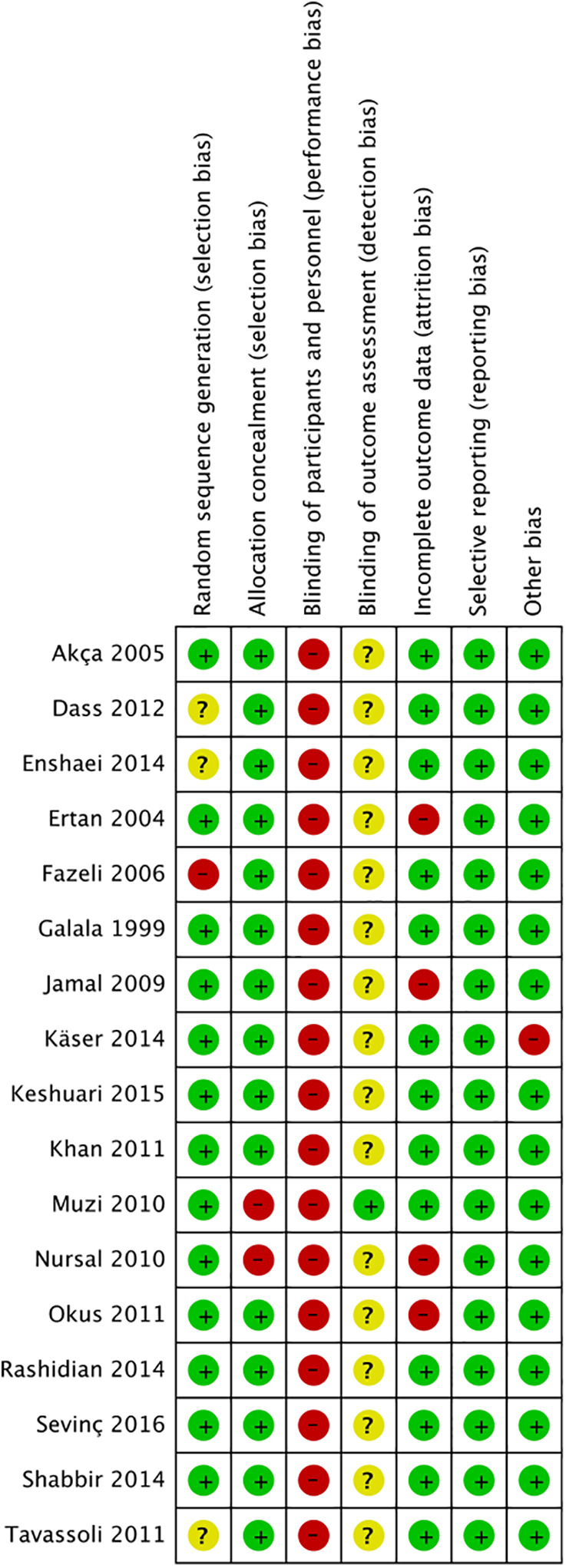
Summary of the risk of bias
2.5. Statistical analysis
Study results were tabulated with the total number of subjects in flap vs the laying open technique or direct closure (using intention to treat or full analysis set), number of events for recurrence or postoperative complications, and mean together with SD for continuous endpoints. Missing SDs were assessed according to the sample size and means for reported P‐values.29 We calculated the risk ratio (RR) of recurrence (and postoperative complications) with flap vs the laying open technique or direct closure according to the inverse variance (IV) approach with their 95% confidence intervals (95% CI). When the number of postoperative complications was equal to zero in each group, it was imputed to 1 in order to estimate the RR. We estimated the mean differences between flaps and the laying open technique or direct closure for continuous endpoints according to the IV approach using their 95% CI. We also estimated the standardised mean differences (SMD) assessing quality of life or patient satisfaction.
To assess heterogeneity across studies, we used forest plots, as well as Cochran's heterogeneity statistic and Higgins I 2 coefficients.30 A P‐value <.1 or I 2 > 50% was considered suggestive of statistical heterogeneity, prompting random‐effects modelling.31 To minimise heterogeneity of the studies, when it was possible, subgroup analyses were also performed. We produced funnel plots to assess publication bias.32We used the Review Manager 5.3 analysis software (The Cochrane Collaboration, Copenhagen, Denmark) for all analyses.
3. RESULTS
The literature search is illustrated in the flow chart of study selection (Figure 2). We included a total of 17 studies in the systematic review.
Figure 2.
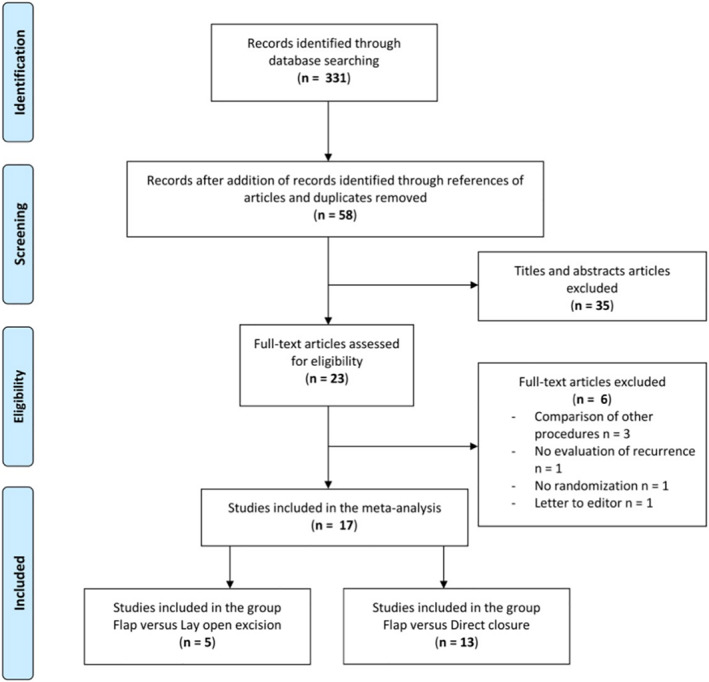
Flow chart of the study selection
3.1. Characteristics of the studies included
Seventeen randomised controlled studies,33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49 involving 2215 cases, were included in the systematic review, and their characteristics are shown in Tables 1 and 2.
Table 1.
Characteristics of the studies that were included: flap vs laying open technique
| Study | No. of patients | Lost to follow up | Type of flap | Ratio flap: other | Inclusion criteria | Exclusion criteria | Primary endpoint | Secondary endpoints | Type of randomisation | Blinding | Follow up | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Comparison flap vs laying open technique | Keshvari et al35 | 321 | 0 | Karidakis flap | 161:160 | PSD | Pain, time to complete wound healing, time to return to work, patient satisfaction, recurrence rate, complications | Computer generated | Patient | Median 49 months | ||
| Käser et al34 | 102 | 5 | Limberg flap | 51:51 | PSD | Acute abscess, recurrent PSD, age < 18 years, lack of consent, immunodeficiency, pregnancy, dermatological disease | Time to return to work | Pain, complications, recurrence rate, patient satisfaction | Computer generated | No | 12 months | |
| Fazeli et al36 2006 | 144 | 6 | Z‐plasty | 72:72 | Acute abscess | Pain, duration of hospital stay, time to return to work, complications, time to complete wound healing, recurrence rate | No | Mean 22 months | ||||
| Jamal et al33 | 49 | 4 | Limberg flap | 24:25 | PSD | Lost to follow up | Pain, duration of hospital stay, complications, recurrence rate | Mean 18 months | ||||
| Rashidian et al37 | 60 | 0 | Limberg flap | 20:40 | Primary PSD | Acute abscess, recurrent PSD | Duration of hospital stay, time to return to work, time to complete wound healing, recurrence rate, complications | Block randomisation | Mean 18 months | |||
Abbreviations: DC, direct closure; PSD, pilonidal sinus disease.
Table 2.
Characteristics of included studies: flap vs direct closure
| Study | No. of patients | Lost to follow up | Type of flap | Ratio flap: other | Inclusion criteria | Exclusion criteria | Primary end‐point | Secondary end‐points | Type of randomisation | Blinding | Follow up | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Comparison flap vs direct closure | Ertan et al38 | 100 | 35 | Limberg flap | 50:50 | PSD | Acute abscess | Duration of hospital stay, time to complete wound healing, time to return to work, complications, recurrence rate, quality of life and patient satisfaction, pain | Mean 19 months | |||
| Nursal et al39 | 238 | 45 | V‐Y advancement flap | 77:161 | PSD | Acute abscess | Complications, recurrence rate, patient satisfaction, time to return to work | Mean 29.7 months | ||||
| Muzi et al40 | 272 | 12 | Limberg flap | 130:130 | PSD | BMI > 35, diabetes, epilepsy, severe allergy to medication, social‐familiar reasons, drug addiction | Time to complete wound healing | Pain, duration of hospital stay, time to return to work, complications, recurrence rate | Computer generated | No | Mean flap 45.74 months/DC 47.83 months | |
| Sevinç et al41 | 150 | 0 | Limberg flap,karydakis flap | 100:50 | Primary PSD | Recurrent PSD | Complications, recurrence rate | Closed envelopes | Patient | Median 24.2 months | ||
| Tavassoli et al42 | 100 | 0 | Limberg flap | 50:50 | PSD | Acute abscess, recurrent PSD, immunodeficiency, diabetes, age < 15 years or > 45 years, severe hirsutism in women, psychiatric disease or poor hygiene | Complications, pain, time to return to work, time to complete wound healing, recurrence rate, patient satisfaction | 6 monthss | ||||
| Okuş et al43 | 93 | 0 | Limberg flap | 49:44 | PSD | Complications, recurrence rate | Closed envelopes | Median 29.5 months | ||||
| Galala et al44 | 46 | 0 | Limberg flap | 24:22 | PSD | Acute abscess, recurrent PSD | Complications, time to return to work, duration of hospital stay, recurrence rate | Closed envelopes | Mean 18 months | |||
| Akca et al45 | 200 | 0 | Limberg flap | 100:100 | PSD | Recurrent PSD, contraindications of general anaesthesia | Pain, duration of hospital stay, complications, time to return to work, recurrence rate | Computer generated |
Median Flap 28 months/DC 29 months |
|||
| Shabbir et al46 | 60 | 0 | Limberg flap | 30:30 | PSD | Recurrent PSD, age < 13 years | Complications, recurrence rate, duration of hospital stay, time to return to work | 12 months | ||||
| Dass et al47 | 80 | 0 | Limberg flap | 40:40 | PSD | Recurrent PSD, acute abscess | Complications, pain, time to return to work, duration of hospital stay, recurrence rate | 36 months | ||||
| Khan et al48 | 120 | 0 | Limberg flap | 60:60 | Primary PSD | Duration of hospital stay, complications, time to return to work, recurrence rate | Computer generated | 24 months | ||||
| Enshaei et al49 | 80 | 0 | Rotation flap | 40:40 | Primary PSD | Acute abscess, recurrent PSD, diabetes, or obesity | Duration of hospital stay, pain, complications, recurrence rate, time to complete wound healing | 6 months | ||||
| Rashidian 37 | 60 | 0 | Limberg flap | 20: 40 | Primary PSD | Acute abscess, recurrent PSD | Duration of hospital stay, time to return to work, time to complete wound healing, recurrence rate, complications | Block randomisation | Mean 18 months | |||
Abbreviations: DC, direct closure; PSD, pilonidal sinus disease.
The population in all studies comprised patients presenting with chronic pilonidal sinus. Among them, 1083 patient underwent a flap procedure, 328 patients underwent a laying open procedure, and 804 patients underwent median direct closure. A total of 114 patients (5.1%) were lost to follow up. Because of reported protocol violations, 14 cases were excluded from the study of Nursal et al.39 No other violations of the study protocols were reported.
Methods of randomisation were detailed for most studies and included computer‐generated randomisation or sealed envelopes and block randomisation. Blinding was not attempted for most studies.
Follow‐up data from the studies ranged from 6 to 49 months.
The characteristics of the population that was included are presented in Table 3.
Table 3.
Characteristics of the populations that were included
| Study | Type of surgery | Median age (years) | Gender | ||||
|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Range | Male (%) | Female (%) | ||
| Keshvari et al35 | All | 24 | 16‐60 | 77.90% | 22.10% | ||
| Fazeli et al36 | All | ||||||
| Käser et al34 | Flap | 26 | 18‐25 | 84% | 16% | ||
| Open | 24 | 18‐52 | 78% | 22% | |||
| Jamal et al33 | Flap | 26.04 | 19‐37 | 87.50% | 12.50% | ||
| Open | 26.84 | 19‐37 | 96% | 4% | |||
| Rashidian et al37 | All | 27.61 | 14‐49 | 78.30% | 21.70% | ||
| Ertan et al38 | Flap | 28 | ± 7.7 | 92% | 8% | ||
| Direct closure | 26.3 | ± 6.8 | 90% | 10% | |||
| Nursal et al39 | All | 26.2 | ± 8.2 | 79.40% | 20.60% | ||
| Muzi et al40 | Flap | 25.05 | ± 7.53 | 88% | 12% | ||
| Direct closure | 25.01 | ± 8.58 | 84% | 12% | |||
| Sevinç et al41 | All | 24 | 18‐47 | 82% | 18% | ||
| Tavassoli et al42 | All | 24 | ± 4.35 | 16‐36 | 80% | 20% | |
| Okuş et al43 | Flap | 24 | 17‐33 | 97.90% | 2.10% | ||
| Direct closure | 25.5 | 17‐43 | 90.90% | 9.10% | |||
| Galala et al44 | Flap | 23 | 17‐30 | 80% | 20% | ||
| Direct closure | 21 | 18‐34 | 80% | 20% | |||
| Akca et al45 | Flap | 26 | 15‐60 | 85% | 15% | ||
| Direct closure | 28 | 17‐43 | 83% | 17% | |||
| Shabbir et al46 | Flap | 90% | 10% | ||||
| Direct closure | 93.30% | 6.70% | |||||
| Dass et al47 | All | 28.4 | ± 8.6 | 16‐48 | 92.50% | 7.50% | |
| Khan et al48 | Flap | 24 | 17‐42 | 88.30% | 11.70% | ||
| Direct closure | 26 | 16‐40 | 85% | 15% | |||
| Enshaei et al49 | Flap | 24.17 | ± 6.05 | 15‐40 | 72.50% | 28% | |
| Direct closure | 55% | 45% | |||||
3.2. Disease recurrence
All studies reported data on disease recurrence. The meta‐analysis showed a trend towards a lower incidence of recurrent disease for flaps vs the laying open technique, with a risk ratio of 0.50, which, however, was not statistically significant (P = .23, 95% CI [0.16‐1.56]) (Figure 3). Because of heterogeneity across the studies (I 2 52%), we carried out a subgroup analysis (Figure 4). This demonstrated a benefit in favour of advancement flaps vs the laying open technique (RR 0.17 [0.04‐0.73], P = .02). However, it involved only the results of the study by Keshvari et al.4 There was no significant difference between the transposition flap and the laying open technique (P = .75). The meta‐analysis showed a lower risk of recurrence in favour of flaps vs direct closure, with an RR of 0.42 [0.21‐0.85] (P = .02) (Figure 3).
Figure 3.
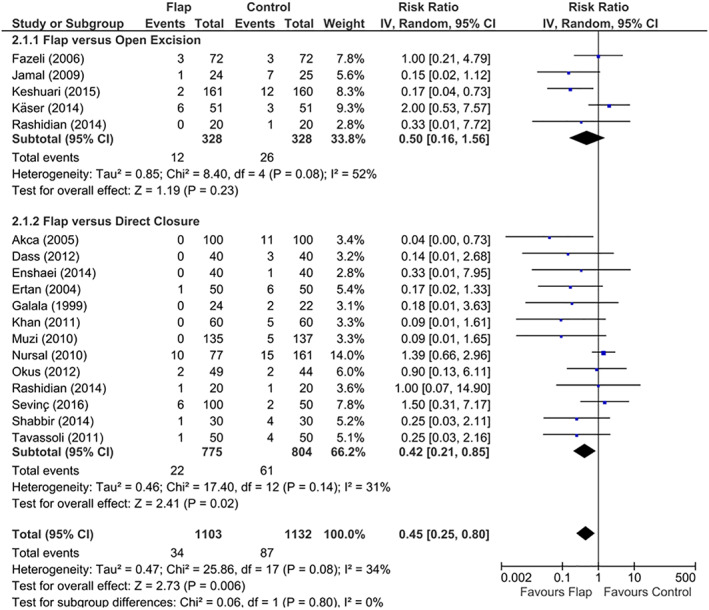
Forest plot of the recurrence rate
Figure 4.
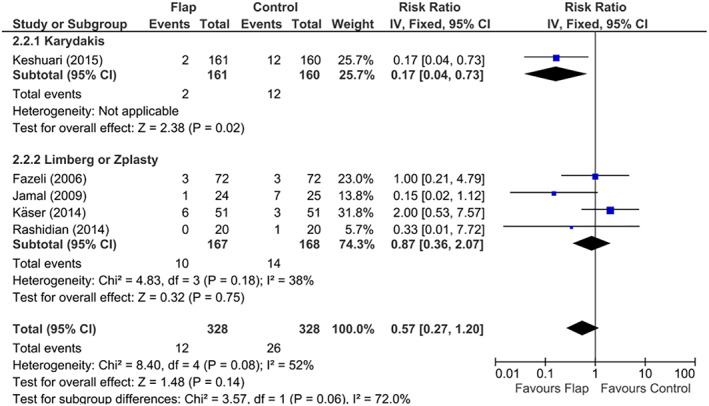
Forest plot of the recurrence rate by flap (for flap vs open excision)
3.3. Time to complete wound healing
Results were given by the number of postoperative days. The meta‐analysis demonstrated a significantly lower wound‐healing time for flaps vs the laying open technique, with a mean benefit of 43.69 [72.60‐14.79] days (P = .003) but no significant difference between flaps and direct closure (P = .27) (Figure 5).
Figure 5.
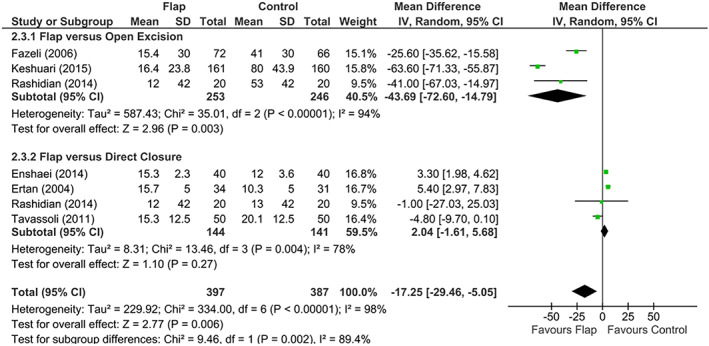
Forest plot of the time to complete wound healing (in days)
3.4. Duration of the incapacity for work
The meta‐analysis demonstrated a significant difference in favour of flap vs other procedures (P ≤ .00001), with a mean difference of 5.63 [10.87‐0.40] days (P = .03), vs the laying open technique and 4.21 [6.26‐2.16] days (P < .0001) vs direct closure (Figure 6).
Figure 6.
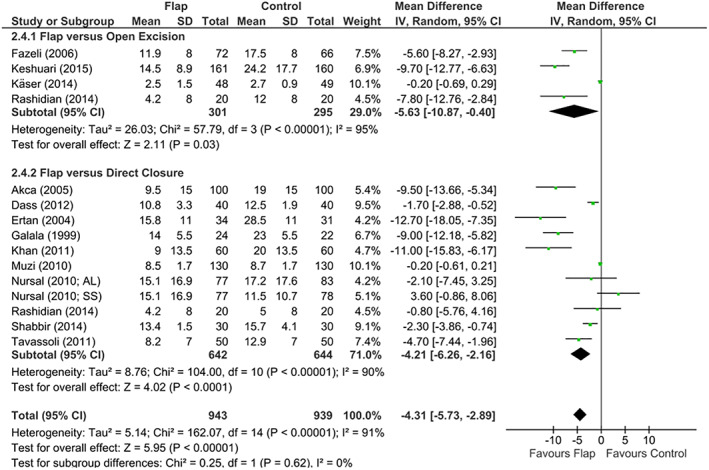
Forest plot of the duration of the incapacity to work (in days). In Nursal et al39, AL is all layers and SS is subcutaneous suture
3.5. Quality of life and patient satisfaction
The meta‐analysis showed no significant difference between flap and the laying open technique in terms of patient satisfaction (P = .32) (Figure 7). The meta‐analysis showed a trend towards a better quality of life and patient satisfaction for flap vs direct closure, with a mean difference of 0.19 [«−0.02» – 0.39], which, however, was not statistically significant (P = .07) (Figure 8).
Figure 7.
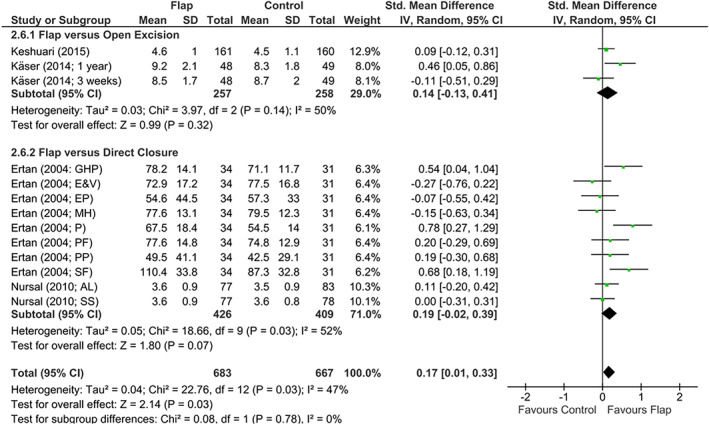
Forest plot of the quality of life and patient satisfaction. For quality of life evaluated using Cardiff Wound Impact Schedule scores (Ertan et al38) : GHP, general health perception; PF, physical functioning; SF, social functioning; PP, role limitation because of physical problems; EP, role limitation because of emotional problems; P, pain; E&V, energy and vitality; MH, mental health. In Nursal et al39, AL, all layers; SS, subcutaneous suture
Figure 8.
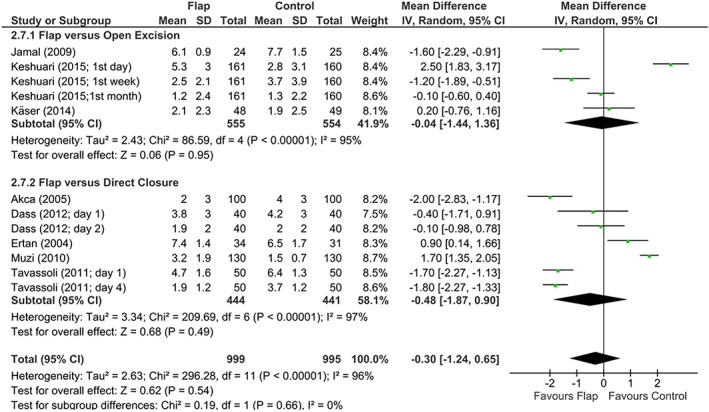
Forest plot of the postoperative pain (Visual Analogue Scale)
3.6. Postoperative pain
The meta‐analysis showed no significant difference between flap and other procedures in terms of postoperative pain (P = .54) (Figure 8).
3.7. Complications
General rate of complications
The meta‐analysis showed a significantly lower general rate of complications in favour of the flap vs the laying open group (RR = 0.57 [0.39‐0.83], P = .004) but no significant difference between flap and direct closure (P = .65)(Figure 9).
Wound infection
Figure 9.
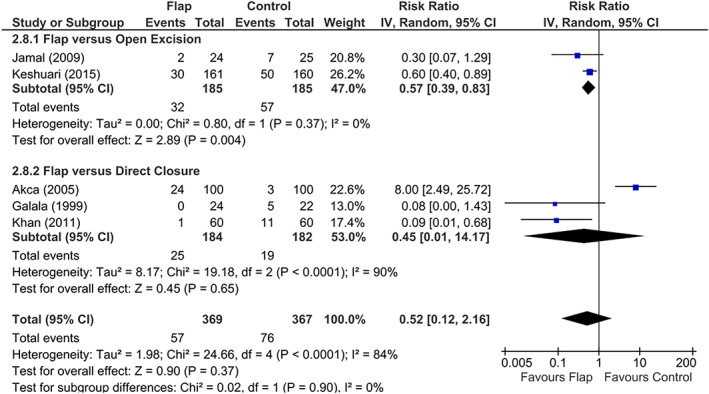
Forest plot of the general rate of complications
The meta‐analysis showed no significant difference between flap and the laying open technique (P = .57) but a significant reduction in the risk of wound infections in favour of flap vs direct closure with a risk ratio of 0.37 [0.25‐0.55] (P < .00001) (Figure 10).
Bleeding and haematoma
Figure 10.
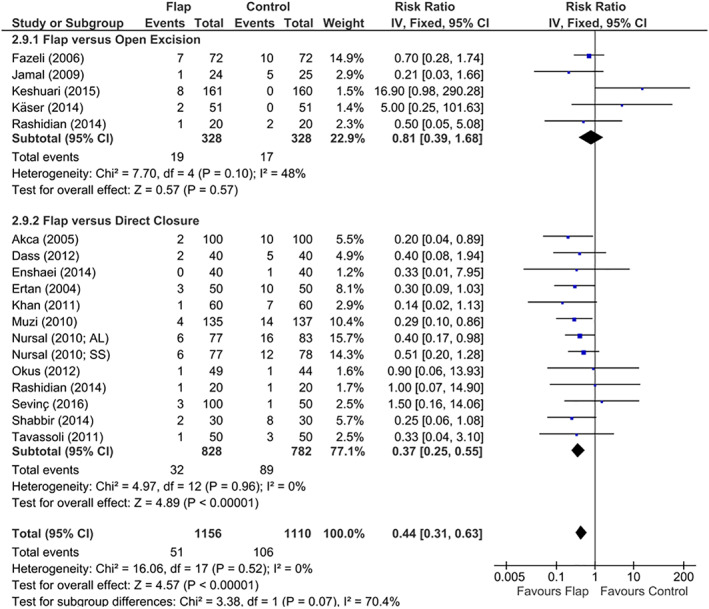
Forest plot of wound infections
The meta‐analysis showed no significant difference between flap and other procedures in terms of the rate of haemorrhagic events (P = .96) (Figure 11).
Skin wound complications: dehiscence and skin necrosis
Figure 11.
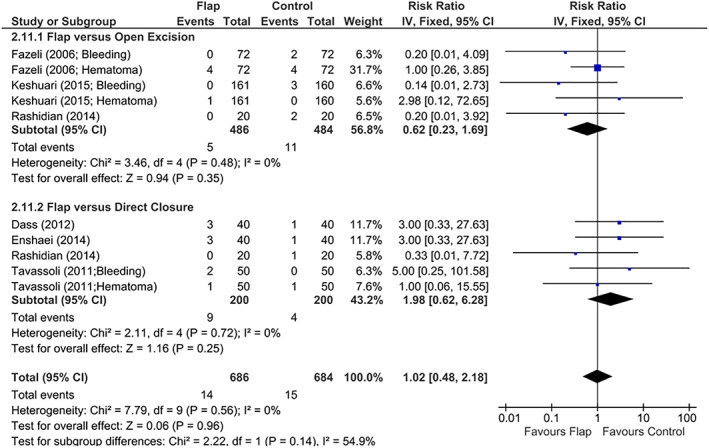
Forest plot of bleeding or haematoma
The meta‐analysis demonstrated a significantly higher risk of dehiscence and skin necrosis for flap vs the laying open technique (RR = 8.83 [1.98‐39.29] (P = .004) (Figure 12). The subgroup analysis for flap vs open excision showed a significantly higher risk of wound complications for advancement flaps (RR = 12.72 [1.55‐104.35], P = .02)4 and a trend towards an increase in wound complication rate for transposition flaps (RR = 6.09 [0.73‐50.72], P = .09) (Figure 13). The meta‐analysis demonstrated a significantly lower risk of wound complications for flap vs direct closure with a risk ratio of 0.43 [0.28‐0.66] (P = .0001) (Figure 13).
Figure 12.
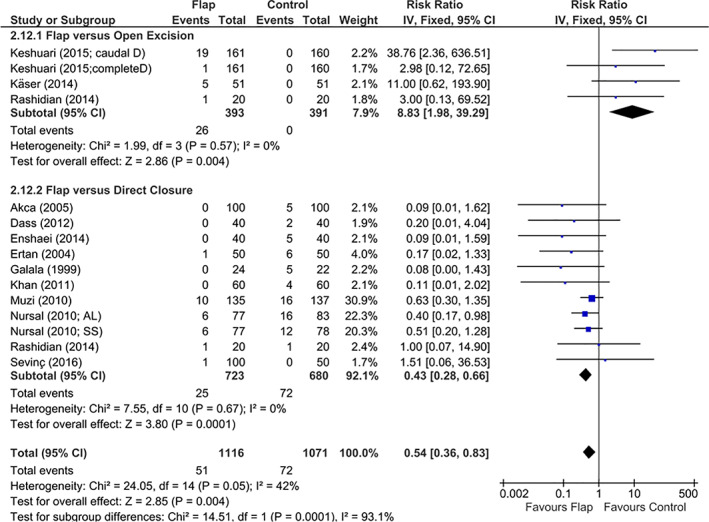
Forest plot of skin wound complications
Figure 13.
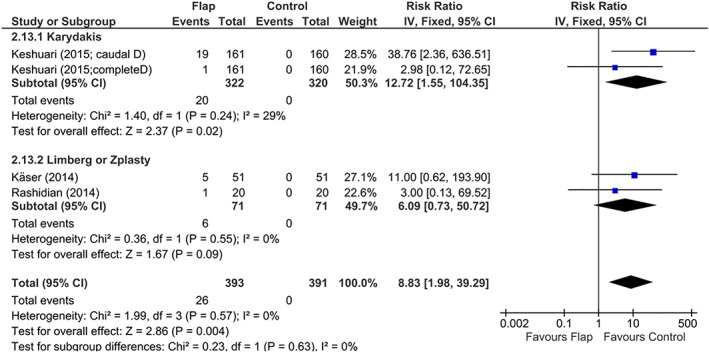
Forest plot of skin wound complications by flap (for flap vs open excision)
3.8. Duration of hospital stay
The meta‐analysis showed a longer duration of hospitalisation for flap vs the laying open technique, with a mean difference of 0.98 [0.28‐1.68] days (P = .006) but a shorter duration of hospitalisation vs direct closure with a benefit of 1.87 [2.88–0.85] days (P = .0003) (Figure 14).
Figure 14.
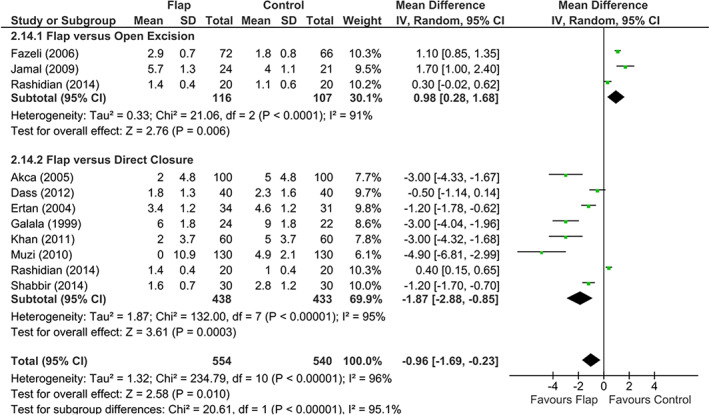
Forest plot of the duration of hospital stay (in days)
3.9. Study bias
Funnel plots showed no evidence of publication bias in this meta‐analysis.
4. DISCUSSION
After surgery for pilonidal disease, the risk of disease recurrence is lower with flap repair than with direct midline closure. The same results were found 10 years ago in the meta‐analysis conducted by McCallum et al., including five trials that compared midline closure (corresponding to direct closure in our study) and off‐midline closure (corresponding to flap repair in our study).25 We included 13 studies that compared flap vs direct closure, which is three times higher than the number of studies included McCallum, and we confirmed their results. These results can be compared with those of two other meta‐analyses that contrasted different modalities of closure, especially midline versus off‐midline: that of Enriquez et al. in 2014 with 10 randomised prospective studies26 and that of Horwood et al. in 2011 with 6 studies.27 The findings were a significant decrease for one and a non‐significant decreasing trend for the other in terms of the risk of recurrence in favour of the off‐midline procedure.
We found no significant difference but rather a trend towards fewer recurrences in favour of flaps vs open excision. With only five randomised prospective studies comparing these two techniques, it is possible that we were underpowered to demonstrate a benefit in favour of flap repair. The same results were shown by McCallum et al. in 2008.25 The lack of randomised prospective studies comparing the laying open technique vs flap repair makes it difficult to rule in favour of either of these two surgical techniques. Nevertheless, our subgroup analysis showed a benefit in favour of advancement flap vs the laying open technique. Although It involved only results of one study,35 it included a significant number of patients (321 patients), which gives it a significant statistical importance.
The wound‐healing time was shorter in flap procedure vs open excision, but there was no significant difference vs direct closure. These results appear logical because open excision involves a secondary intention healing by granulation, which is much slower than the usual healing time for a closed scar. Healing by secondary intention can take up to several months.
The general rate of complications was reduced in case of flap reconstruction vs open excision. This result appears incongruous with regard to the lack of increase in haemorrhage, infectious or skin/wound complications for the laying open technique vs flap. It can be explained by the fact that two studies33, 45 evaluating this global rate took into account delayed healing of the skin over 3 months at this rate.
We found a lower risk of wound infection after flap than after direct closure. These results are similar to the three previous meta‐analyses for this outcome.25, 26, 27
Wound complications were significantly higher for advancement flaps vs open excision. This underlies the risk of suture disruption that is also present in case of flap reconstruction, even though this risk is much lower in comparison with direct closure. This can be explained by excessive tension on the suture in case of direct closure, whereas flap procedure tension is more homogeneously distributed with the recruitment of adjacent trophic tissues. Once again, all these results encourage the cessation of the direct closure technique in the surgical management of pilonidal disease.
Patients who had flap reconstruction returned to work more quickly, in a mean of 3 to 6 days earlier, than those with direct closure or the laying open technique. This implies that the invalidity caused by flaps was reduced in comparison with other procedures, allowing an earlier return to a professional activity and to other activities of daily living. According to Enriquez et al.26 and Horwood et al.,27 who compared off‐midline closure with median midline closure, the same results were found in favour of the flap technique. We carried out the first meta‐analysis that showed significantly less time to return to work in case of flap vs the laying open technique. Through extrapolation, we can assume that costs associated with sick leave following surgery are reduced in case of flaps in comparison with other procedures. This could be a public health benefit.
The duration of hospitalisation was reduced in case of flaps vs direct closure. These data are difficult to explain because a flap often requires more monitoring. However, because of some excessive tension that could be generated by direct closure, greater caution was taken when surveying and discharging the patient. Frequent suture disruption and infections after direct closure are also likely to increase the duration of hospitalisation.
More recently, Stauffer et al. have proposed a meta‐analysis, merged data analysis, and comprehensive study on the recurrence of pilonidal sinus disease treated by common surgical procedures.28 The strength of this study is the number of procedures and patients included, which gives a global picture of the rate and time of recurrence according to the procedure used. Its limitation is that non‐randomised controlled trials have been included, reducing the statistical impact of the findings. For example, at five postoperative years, Bascom and Karydakis flaps have been found to lead to less recurrence than the laying open technique, which leads to less recurrence than primary midline closure, in their analysis of randomised controlled trials. Regarding the analysis of non‐randomised controlled studies, there was also less recurrence with Karydakis, Bascom, and Limberg flap reconstruction in comparison with open and limited excision techniques, which in turn resulted in less recurrence than the direct closure. Many other common procedures are also compared, finding overall higher rates of early and late recurrence for other surgery than flap reconstruction or laying open excision.
5. LIMITATIONS
We included studies comparing different types of flaps to open excision and direct closure. Each type of flap has its own rate of complication and failure, with some flaps more reliable than others, particularly in terms of skin wound complications (skin necrosis and skin dehiscence). In addition, flap reconstruction is more successful in some surgeons' hands than others. Reconstructive surgeons have specific and adequate training in flap reconstruction. However, pilonidal disease is mostly managed by general surgeons who are less experienced in flap surgery. Lack of training can lead to a higher complication rate than in the studies that were included.
Mean follow up was heterogeneous among the studies, with the longest follow up at 49 months and the shortest at 6 months. Late recurrence was poorly represented in the studies, and the late recurrence rate may be underestimated.
Most included studies exclude recurrences. Only two studies33, 36 in the laying open technique group and three studies38, 39, 40 in the flap group vs direct closure did not exclude recurrences. Most other included studies excluded recurrences, and for three studies,35, 43, 48 no precise information was provided on exclusion factors. Thus, the population of patients with a recurrent pilonidal cyst may have been under‐represented in our meta‐analysis. As the recurrence itself is a risk factor for further recurrence, the recurrence rates we obtained may have potentially been underestimated.
The heterogeneity was high among the studies included in our meta‐analysis, particularly in terms of the number of patients included, duration of follow up, exclusion criteria, and scales of quality‐of‐life assessment. It could represent a limit in the interpretation of our results.
We have excluded pilonidal abscess because complete removal of the cyst should not be performed during the inflammatory phase. Oedema and acute inflammation would impede the exhaustive delimitation of the wall region concerned, particularly paramedian fistulas. Surgical drainage of the abscess will allow the reduction of acute inflammation in a few weeks, allowing better identification of the fistula system during excision surgery, which will be performed at distance from any abscess.50 Some authors recommend placing the incision in a paramedian axis51 or associating curettage of the cyst52, 53 in order to limit the risk of recurrence. Here, again, treatment is not consensual and could be studied.
5.1. Implications for current practices
In view of the recurrence rate and postoperative morbidity, direct closure should be avoided.
Flap repair had significant advantages over laying open excision, especially in terms of faster wound healing and shorter return to work. This technique could be favoured, and surgeons should be trained to perform flap surgery.
5.2. Implications for research
Pilonidal disease affects a young and active population, incurring costs in terms of hospitalisation, sick leave, and home nursing care. Economic studies that take into account the costs of hospital stay, duration of home care, and duration of sick leave are necessary to choose between flap repair and the laying open technique.
6. CONCLUSION
In light of superiority of flap repair vs direct closure in terms of a lower recurrence rate and fewer postoperative wound infections, we should completely avoid the direct primary closure technique. Compared with the laying open technique, the superiority of flap repair has not yet been proven. However, it had the advantages of faster healing and a shorter time to return to work and normal activities.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
Berthier C, Bérard E, Meresse T, Grolleau J‐L, Herlin C, Chaput B. A comparison of flap reconstruction vs the laying open technique or excision and direct suture for pilonidal sinus disease: A meta‐analysis of randomised studies. Int Wound J. 2019;16:1119–1135. 10.1111/iwj.13163
REFERENCES
- 1. Patey DH. A reappraisal of the acquired theory of sacrococcygeal pilonidal sinus and an assessment of its influence on surgical practice. Br J Surg. 1969;56:463‐466. [DOI] [PubMed] [Google Scholar]
- 2. Patey DH, Scarff RW. Pathology of postanal pilonidal sinus; its bearing on treatment. Lancet. 1946;2:484‐486. [DOI] [PubMed] [Google Scholar]
- 3. Patey DH, Scarff RW. Pilonidal sinus in a barber's hand with observations on postanal pilonidal sinus. Lancet. 1948;2:13. [DOI] [PubMed] [Google Scholar]
- 4. Bascom J. Pilonidal disease : origin from follicules of hairs and results of follicule removal as treatment. Surgery. 1980;87:567‐572. [PubMed] [Google Scholar]
- 5. Buie L. Jeep Disease. American Society of Colon and Rectal Surgeons. Dis Col & Rect. 1982;25:384‐390. [Google Scholar]
- 6. Yamashita Y, Nagae H, Hashimoto I. Ambulatory surgery for pilonidal sinus: tract excision and open treatment followed by at‐home irrigation. J Med Invest. 2016;63:216‐218. [DOI] [PubMed] [Google Scholar]
- 7. Garg P. Laying open (deroofing) and curettage under local anesthesia for pilonidal disease: an outpatient procedure. World J Gastrointestinal Surg. 2015;7:214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Garg P, Menon GR, Gupta V. Laying open (deroofing) and curettage of sinus as treatment of pilonidal disease: a systematic review and meta‐analysis: lay open and curettage for pilonidal sinus. ANZ J Surg. 2016;86:27‐33. [DOI] [PubMed] [Google Scholar]
- 9. Lee SL, Tejirian T, Abbas MA. Current management of adolescent pilonidal disease. J Pediatr Surg. 2008;43:1124‐1127. [DOI] [PubMed] [Google Scholar]
- 10. Emiroglu M, Karaali C, Esin H, Akpinar G, Aydin C. Treatment of pilonidal disease by phenol application. Turkish J Surg. 2017;33:5‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kayaalp C, Olmez A, Aydin C, Piskin T, Kahraman L. Investigation of a one‐time phenol application for pilonidal disease. Med Princ Pract. 2010;19:212‐215. [DOI] [PubMed] [Google Scholar]
- 12. Dag A, Colak T, Turkmenoglu O, Sozutek A, Gundogdu R. Phenol procedure for pilonidal sinus disease and risk factors for treatment failure. Surgery. 2012;151:113‐117. [DOI] [PubMed] [Google Scholar]
- 13. Aygen E, Arslan K, Dogru O, Basbug M, Camci C. Crystallized phenol in nonoperative treatment of previously operated, recurrent pilonidal disease. Diseases of the Colon & Rectum. 2010;53:932‐935. [DOI] [PubMed] [Google Scholar]
- 14. Dalenback J, Magnusson O, Wedel N, Rimback G. Prospective follow‐up after ambulatory plain midline excision of pilonidal sinus and primary suture under local anaesthesia – efficient, sufficient, and persistent. 2004; 6. [DOI] [PubMed] [Google Scholar]
- 15. Serour E, Somekh F, Krutman B, Gorenstein A. Excision with primary closure and suction drainage for pilonidal sinus in adolescent patients. Pediatr Surg Int. 2002;18:159‐161. [DOI] [PubMed] [Google Scholar]
- 16. Karydakis GE. New approach to the problem of pilonidal sinus. Lancet. 1973;302:1414‐1415. [DOI] [PubMed] [Google Scholar]
- 17. Bascom J. Pilonidal sinus. Current Therapy in Colon and Rectal Surgery. 1990;1:1‐8. [Google Scholar]
- 18. Tekin A. Pilonidal sinus: experience with the Limberg flap. Colorectal Dis. 1999;1:29‐33. [DOI] [PubMed] [Google Scholar]
- 19. Milito G, Cortese F, Casciani CU. Rhomboid flap procedure for pilonidal sinus: results from 67 cases. Int J Colorectal Dis. 1998;13:113‐115. [DOI] [PubMed] [Google Scholar]
- 20. Middleton MD. Treatment of pilonidal sinus by Z‐plasty. Br J Surg. 1968;55:516‐518. [DOI] [PubMed] [Google Scholar]
- 21. Schoeller T, Wechselberger G, Otto A, Papp C. Definite surgical treatment of complicated recurrent pilonidal disease with a modified fasciocutaneous V‐Y advancement flap. Surgery. 1997;121:258‐263. [DOI] [PubMed] [Google Scholar]
- 22. Saray A, Dirlik M, Caglikulekci M, Turkmenoglu O. Gluteal V‐Y advancement fasciocutaneous flap for treatment of chronic pilonidal sinus disease. Scand J Plast Reconstr Surg Hand Surg. 2002;36:80‐84. [DOI] [PubMed] [Google Scholar]
- 23. Onishi K, Maruyama Y. Sacral adipofascial turn‐over flap for the excisional defect of pilonidal sinus. Plast Reconstr Surg. 2001;108:2006‐2010. [DOI] [PubMed] [Google Scholar]
- 24. Başterzi Y, Canbaz H, Aksoy A, Sar A, Türkmenoğlu MÖ, Çağlkülekçi M. Reconstruction of extensive pilonidal sinus defects with the use of S‐GAP flaps. Ann Plast Surg. 2008;61:197‐200. [DOI] [PubMed] [Google Scholar]
- 25. McCallum IJD, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta‐analysis. BMJ. 2008;336:868‐871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Enriquez‐Navascues JM, Emparanza JI, Alkorta M, Placer C. Meta‐analysis of randomized controlled trials comparing different techniques with primary closure for chronic pilonidal sinus. Tech Coloproctol. 2014;18:863‐872. [DOI] [PubMed] [Google Scholar]
- 27. Horwood J, Hanratty D, Chandran P, Billings P. Primary closure or rhomboid excision and Limberg flap for the management of primary sacrococcygeal pilonidal disease? A meta‐analysis of randomized controlled trials: meta‐analysis of randomized controlled trials. Colorectal Dis. 2012;14:143‐151. [DOI] [PubMed] [Google Scholar]
- 28. Stauffer VK, Luedi MM, Kauf P, et al. Common surgical procedures in pilonidal sinus disease: A meta‐analysis, merged data analysis, and comprehensive study on recurrence. Scientific Rep. 2018;8:3058. Available from: http://www.nature.com/articles/s41598-018-20143-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45:769‐773. [DOI] [PubMed] [Google Scholar]
- 30. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ. 2003;327:557‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. DerSimonian R, Laird N. Meta‐analysis in clinical trials revisited. Contemp Clin Trials. 2015;45:139‐145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour‐enhanced meta‐analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol. 2008;61:991‐996. [DOI] [PubMed] [Google Scholar]
- 33. Jamal A, Shamim M, Hashmi F, Qureshi MI. Open excision with secondary healing versus rhomboid excision with Limberg transposition flap in the management of Sacrococcygeal pilonidal disease. J Pak Med Assoc. 2009;59:4. [PubMed] [Google Scholar]
- 34. Käser SA, Zengaffinen R, Uhlmann M, Glaser C, Maurer CA. Primary wound closure with a Limberg flap vs. secondary wound healing after excision of a pilonidal sinus: a multicentre randomised controlled study. Int J Colorectal Dis. 2015;30:97‐103. [DOI] [PubMed] [Google Scholar]
- 35. Keshvari A, Keramati MR, Fazeli MS, Kazemeini A, Meysamie A, Nouritaromlou MK. Karydakis flap versus excision‐only technique in pilonidal disease. J Surg Res. 2015;198:260‐266. [DOI] [PubMed] [Google Scholar]
- 36. Fazeli MS, Adel MG, Lebaschi AH. Comparison of outcomes in z‐plasty and delayed healing by secondary intention of the wound after excision of the sacral pilonidal sinus: results of a randomized, clinical trial. Diseases of the Colon & Rectum. 2006;49:1831‐1836. [DOI] [PubMed] [Google Scholar]
- 37. Rashidian N, Vahedian‐Ardakani J, Baghai‐Wadji M, et al. How to repair the surgical defect after excision of sacrococcygeal pilonidal sinus: a dilemma. J Wound Care. 2014;23:630‐633. [DOI] [PubMed] [Google Scholar]
- 38. Ertan T, Koc M, Gocmen E, Aslar AK, Keskek M, Kilic M. Does technique alter quality of life after pilonidal sinus surgery? Am J Surg. 2005;190:388‐392. [DOI] [PubMed] [Google Scholar]
- 39. Nursal TZ, Ezer A, Çalışkan K, Törer N, Belli S, Moray G. Prospective randomized controlled trial comparing V–Y advancement flap with primary suture methods in pilonidal disease. Am. J Surg. 2010;199:170‐177. [DOI] [PubMed] [Google Scholar]
- 40. Muzi MG, Milito G, Cadeddu F, et al. Randomized comparison of Limberg flap versus modified primary closure for the treatment of pilonidal disease. Am J Surg. 2010;200:9‐14. [DOI] [PubMed] [Google Scholar]
- 41. Sevinç B, Karahan Ö, Okuş A, Ay S, Aksoy N, Şimşek G. Randomized prospective comparison of midline and off‐midline closure techniques in pilonidal sinus surgery. Surgery. 2016;159:749‐754. [DOI] [PubMed] [Google Scholar]
- 42. Tavassoli A, Noorshafiee S, Nazarzadeh R. Comparison of excision with primary repair versus Limberg flap. Int J Surg. 2011;9:343‐346. [DOI] [PubMed] [Google Scholar]
- 43. Okuş A, Sevinç B, Karahan Ö, Eryılmaz MA. Comparison of Limberg flap and tension‐free primary closure during pilonidal sinus surgery. World J Surg. 2012;36:431‐435. [DOI] [PubMed] [Google Scholar]
- 44. Galala KHA, Salam IMA, Samaan KRA, et al. Treatment of pilonidal sinus by primary closure with a transposed rhomboid flap compared with deep suturing: a prospective randomised clinical trial. Eur J Surg. 1999;165:468‐472. [DOI] [PubMed] [Google Scholar]
- 45. Akca T, Colak T, Ustunsoy B, Kanik A, Aydin S. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. Br J Surg. 2005;92:1081‐1084. [DOI] [PubMed] [Google Scholar]
- 46. Shabbir F, Ayyaz M, Farooka MW, Toor AA, Sarwar H, Malik AA. Modified Limberg's flap versus primary closure for treatment of pilonidal sinus disease: a comparative study. J Pak Med Assoc. 2014;64:4. [PubMed] [Google Scholar]
- 47. Dass TA, Zaz M, Rather A, Bari S. Elliptical excision with midline primary closure versus rhomboid excision with Limberg flap reconstruction in Sacrococcygeal pilonidal disease: a prospective, randomized study. Indian J Surg. 2012;74:305‐308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Khan PS, Hayat H, Hayat G. Limberg flap versus primary closure in the treatment of primary Sacrococcygeal pilonidal disease; a randomized clinical trial. Indian J Surg. 2013;75:192‐194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Enshaei A, Motearefi S. Comparison of two surgical methods, primary closure and rotational flap, in patients with chronic pilonidal sinus. Glob J Health Sci. 2014;6:18‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gidwani AL, Murugan K, Nasir A, Brown R. Incise and lay open: an effective procedure for coccygeal pilonidal sinus disease. Ir J Med Sci. 2010;179:207‐210. [DOI] [PubMed] [Google Scholar]
- 51. Webb PM, Wysocki AP. Does pilonidal abscess heal quicker with off‐midline incision and drainage? Tech Coloproctol. 2011;15:179‐183. [DOI] [PubMed] [Google Scholar]
- 52. Vahedian J, Nabavizadeh F, Nakhaee N, Vahedian M, Sadeghpour A. Comparison between drainage and curettage in the treatment of acute pilonidal abcess. Saudi Med J. 2005;26:553‐555. [PubMed] [Google Scholar]
- 53. Millar DM, Lord PH. The treatment of acute postanal pilonidal abscess. Br J Surg. 1967;54:598‐599. [DOI] [PubMed] [Google Scholar]


