An 85‐year‐old woman was referred to our department for a painful, bleeding, ulcerated red to violaceus plaque, measuring 12 × 4 cm, located on the pretibial surface of right leg. The lesion was surrounded by red to violaceus satellite macules and plaques (Figure 1). The patient also presented a long‐standing condition of chronic lymphoedema in the lower limbs. Her medical history was positive for urothelial carcinoma (pTa G1) treated with transurethral resection and intravescical chemotherapy with epirubicin in 2011, type II diabetes with chronic obstructive arteriopathy, hypertensive cardiopathy, sigmoid diverticola, intestinal polyposis, and chronic kidney disease. Dermoscopic examination showed blue, dark red, and violaceus areas; a whitish veil; and white lines (Figure 2). Histology showed dermal proliferation of vascular structures with a high mitotic index and atypical mytosis. A diagnosis of Stewart–Treves syndrome (STS) was made.
Figure 1.

Painful, bleeding, ulcerated red to violaceus plaque located on the pretibial surface of right leg
Figure 2.
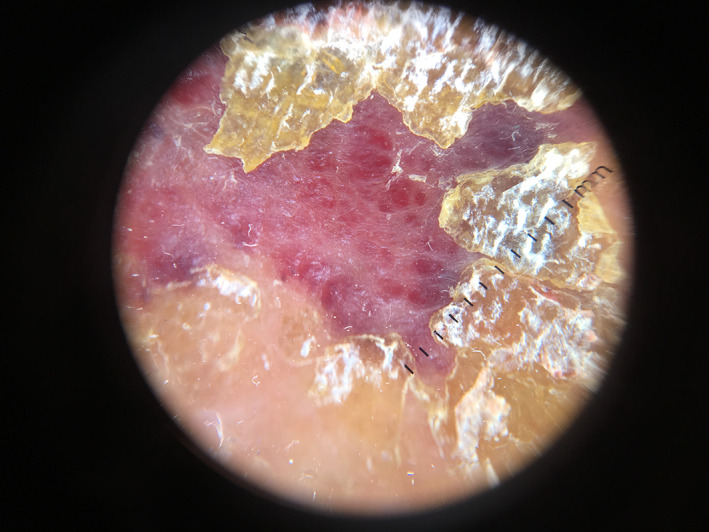
Dermoscopic examination showed blue, dark red, and violaceus areas; a whitish veil; and white lines
STS refers to a cutaneous angiosarcoma, a rare and aggressive malignant tumour accounting for 1% to 2% of all soft tissue sarcomas, arising in the setting of chronic lymphoedema of any origin, particularly following mastectomy.1 Several authors have proposed the underlying pathophysiology of STS: first, the lymphatic blockage may encourage neoplastic transformation; second, the local immunodeficiency may promote vascular oncogenesis.2 Radiotherapy does not appear to have a role in the pathogenesis of the disease; nevertheless, axillary irradiation may enhance the risk of post‐treatment lymphoedema. Clinically, a palpable subcutaneous mass is usually the first lesion, developing in the area of the chronic lymphoedema. Subsequently, multiple violaceous macules or nodules may occur, with surrounding satellite lesions. Eventually, extensive cutaneous nodules and metastatic disease may develop. Indeed, according to Ruocco et al, when the local mechanisms of immune surveillance begin to fail, the lymphoedematous region becomes an immunologically vulnerable area, predisposed to malignancy.3, 4 Histologically, proliferating vascular channels that dissect the dermal collagen may be found in the STS. Sometimes, the epidermis could be hyperkeratotic, acanthotic, or atrophic. Immunochemistry is frequently needed to establish the diagnosis: angiosarcomas may typically express CD31, CD34, D2‐40, and ERG.5 Dermoscopic examination may help the dermatologist showing the classic colours of vascular lesions: a graduation of red, purple, and blue.6, 7, 8 Various colour gradation could be an important dermoscopic feature of this kind of tumour as it is not found in other vascular lesions, such as common purpura and ecchymosis.7 Moreover, cutaneous angiosarcoma is usually characterised by the absence of well‐defined vascular structures, such as lacunae/lagoons and vessels. This is helpful for the differential diagnosis with amelanotic melanoma or with psoriasis.9 Furthermore, whitish veil areas with a white or skin‐coloured central area and a strengthening of the purple colour at the periphery of the lesion may be found in cutaneous angiosarcoma.10 An early dermatological evaluation and appropriate dermoscopic examination may help avoid a delayed diagnosis of STS. Therefore, dermoscopy should be considered an useful tool to differentiate cutaneous angiosarcoma from other benign vascular lesions in such patients, when no lacunae are seen and ecchymotic colours and colour variegation are present and do not resolve over time, thus leading to an early correct diagnosis and an improvement in the prognosis. As several therapies, such as chemotherapy do not significantly improve overall survival, early amputation or wide local excision can create the best chance for long‐term survival.11
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
REFERENCES
- 1. Cozen W, Bernstein L, Wang F, Press MF, Mack TM. The risk of angiosarcoma following primary breast cancer. Br J Cancer. 1999;81:532‐536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ruocco V, Schwartz RA, Ruocco E. Lymphedema: an immunologically vulnerable site for development of neoplasms. J Am Acad Dermatol. 2002;47:124‐127. [DOI] [PubMed] [Google Scholar]
- 3. Sharma A, Schwartz RA. Stewart–Treves syndrome: pathogenesis and management. J Am Acad Dermatol. 2012;67:1342‐1348. [DOI] [PubMed] [Google Scholar]
- 4. Marasca C, Annunziata MC, Cantelli M, Marasca D, Fabbrocini G. Marjolin's ulcer in a paraplegic man: a further example of the immunocompromised district. Int Wound J. 2019;16(2):574‐575. 10.1111/iwj.13022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Young RJ, Brown JN, Reed MW, Hughes D, Woll PJ. Angiosarcoma. Lancet Oncol. 2010;11:983‐991. 10.1016/S1470-2045(10)70023-1. [DOI] [PubMed] [Google Scholar]
- 6. Cozzani E, Chinazzo C, Ghigliotti G, Pastorino C, Gasparini G, Parodi A. Cutaneous angiosarcoma: the role of dermoscopy to reduce the risk of a delayed diagnosis. Int J Dermatol. 2018;57(8):996‐997. 10.1111/ijd.13966. [DOI] [PubMed] [Google Scholar]
- 7. Oiso N, Matsuda H, Kawada A. Various color gradations as a dermatoscopic feature of cutaneous angiosarcoma of the scalp. Australas J Dermatol. 2013;54:36‐38. [DOI] [PubMed] [Google Scholar]
- 8. Lallas A, Moscarella E, Argenziano G, et al. Dermoscopy of uncommon skin tumors. Australas J Dermatol. 2014;55:53‐62. [DOI] [PubMed] [Google Scholar]
- 9. Minagawa A, Koga H, Okuyama R. Vascular structure absence under dermoscopy in two cases of angiosarcoma on the scalp. Int J Dermatol. 2014;53:350‐352. [DOI] [PubMed] [Google Scholar]
- 10. De Giorgi V, Grazzini M, Rossari S, et al. Dermoscopy pattern of cutaneous angiosarcoma. Eur J Dermatol. 2011;21:113‐114. [DOI] [PubMed] [Google Scholar]
- 11. Berebichez‐Fridman R, Deutsch YE, Joyal TM, et al. Stewart–Treves syndrome: a case report and review of the literature. Case Rep Oncol. 2016;9:205‐211. [DOI] [PMC free article] [PubMed] [Google Scholar]


