Table 3.
Summary of studies examining effects of documented severe malnutrition in childhood on non-communicable disease (NCD) outcomes
| Study | Setting and population | Type/timing of severe malnutrition (SM) exposure | Outcomes | Key findings* | Risk-of-bias score (IV/EV)† |
| Case-control studies | |||||
| Chege15 |
Cases: patients with diabetes 61.8±10.9 years, Kenya (n=45) Controls: age and sex-matched non-diabetics from same area attending outpatient clinics (n=45) |
Self-reported episode of SM in childhood Exposure age not specified |
T2D risk factors | ↑ Childhood SM among diabetics | – / – |
| Fekadu et al16 |
Cases: insulin-requiring diabetics 18–40 years, Ethiopia (n=107) Controls: age and sex-matched patients attending other hospital clinics (n=110) |
Self-reported episode of childhood SM Exposure age not specified |
Insulin-requiring diabetes risk factors | ↑ Childhood SM in diabetics | ·/ – |
| Prospective cohort studies | |||||
| Benefice et al65 |
Ex-malnourished: children 5.5±0.5 years, Senegal (n=52) Chronic controls: chronically undernourished children (n=54) Well-nourished controls (WN): age-matched, well-nourished children (n=33) |
Marasmus Median age: 14 months |
Motor fitness, anthropometry | ↓ Handgrip in post-SM versus chronic controls ↓ Height/weight for age versus WN controls ↓ Distance throw, jump, agility/shuttle run versus WN controls ↔ Endurance run |
·/ – |
| Boulé et al52 |
Ex-malnourished: young men 22.0±3.6 years, Mexico (n=26) Controls: young men 26.5±2.1 years with no history of SM (n=27) |
Marasmus, kwashiorkor Age at admission: ≤1 years |
Insulin sensitivity, abdominal obesity | ↓ Insulin sensitivity w/ high abdominal fat versus fat-matched controls | · / – |
| Bourdon et al77 |
Ex-malnourished: children 9.6±1.6 years, Malawi (n=69) Sibling controls: closest in age to case child with no history of SM (n=44) Community controls: age and sex-matched (n=37) |
Marasmus and kwashiorkor Median age at admission: 21.5 months |
Cardiometabolic disease markers | ↔ Metabolites | · / – |
| Cook23 |
Ex-malnourished: children 6.7–14.9 years, Uganda (n=31) Controls: children raised in similar environment as cases with no history of SM (n=21) |
Kwashiorkor Mean age at admission: 1.9 years |
Carbohydrate tolerance | ↓ Glucose clearance ↑ Blood glucose 2 hours post oral glucose tolerance test (OGTT) |
· / – |
| Francis-Emmanuel et al53 |
Ex-malnourished: adult marasmus survivors (MS) (n=42) and kwashiorkor survivors (KS) (n=38) 17–50 years, Jamaica Community controls: age, sex, BMI-matched (n=70) Birthweight-matched controls: age-matched (n=40) |
Marasmus and kwashiorkor Age at admission: 6–18 months |
Glucose metabolism | ↔ Fasting plasma glucose ↑ Glucose intolerance (MS versus KS) ↓ Insulin sensitivity (MS versus KS) ↔ Insulin sensitivity (MS versus controls) ↓ Insulinogenic and oral disposition indices (MS vs all groups) |
·· / – |
| Gonzalez-Barranco et al42 |
Ex-malnourished: young men 20.2±3.6 years, Mexico (n=52) Controls: young men with no history of SM (n=50) |
Marasmus, kwashiorkor Mean age at admission: 4.5 months |
Glucose metabolism, lipid profile, blood pressure (BP) | ↑ Areas under the curves of glucose and insulin ↓ Insulin sensitivity, BP ↔ Fasting blood glucose, lipid profile |
·· / – |
| Idohou-Dossou et al20 |
Ex-malnourished: children 6–8 years, Senegal (n=24) Sibling controls (SC): closest in age to case child with no history of SM (n=24) Well-nourished controls (WN): age-matched healthy children from wealthier area (n=19) |
Marasmus Age at admission: 1–3 years |
Biochemical nutritional indicators, growth factors, anthropometry | ↓ Apolipoprotein A↔ versus WN controls, no difference between post-SM and SC ↓ Lean mass in post-SM and SC associated with low IGF-↔ |
· / – |
| Kajubi24 |
Ex-malnourished: adolescents 11–19 years, Uganda (n=15) Controls: adolescents with no history of SM (n=11) |
Kwashiorkor Age at admission: 1.5–3 years |
Pancreatic function | ↔ Blood glucose post-OGTT ↓ Fasting plasma insulin |
·/– |
| Lelijveld et al9 |
Ex-malnourished: children 9.6±1.6 years, Malawi (n=320) Sibling controls (SC): closest in age to case child with no history of SM (n=217) Community controls (CC): age and sex-matched with no history of SM (n=184) |
Marasmus, kwashiorkor Median age at admission: 24 months |
Blood markers of NCDs, physical capacity, anthropometry | ↔ Glucose tolerance, glycosylated haemoglobin, blood lipids, salivary cortisol ↑ Diastolic BP in post-SM versus SC ↓ Handgrip strength versus CC/SC ↓ Lean mass versus CC but similar to SC |
··/– |
| Moore et al25 | Rural adults (mean age 35.8 years), Gambia (n=145) | Low weight-for-age z-score (WAZ) WAZ measured at 18 months |
Cardiovascular disease (CVD) risk factors | ↓ Fasting plasma insulin in lower WAZ quartiles ↔ Fasting blood glucose, blood glucose or insulin post-OGTT, cortisol, BP |
··/– |
| Sheppard et al84 | Ex-malnourished: adult survivors of kwashiorkor (KS) 29.82±9.03 years (n=21) or marasmus (MS) 25.02±5.69 years (n=23), Jamaica | Marasmus, kwashiorkor Mean age at admission: 11 months |
Epigenetic profile in muscle tissue | ↕ Differences in DNA methylation of 63 genes related to, body size/composition, glucose metabolism, musculoskeletal growth, cardiovascular pathways between MS and KS | ·/– |
| Tennant et al43 |
Ex-malnourished: adult survivors of childhood kwashiorkor (n=62) 27.2±7.8 years and marasmus (n=54) 29.2±8.4 years, Jamaica Community controls: age and sex matched with no history of SM (n=45) |
Marasmus, kwashiorkor Mean age at admission: 12 months |
Cardiovascular structure/function | ↓ Left ventricular outflow tract parameter, stroke volume, cardiac output, pulse wave velocity ↑ Diastolic BP ↔ Systolic BP ↑ Systemic vascular resistance ↑ Heart rate in MS versus KS ↔ Large vessel, cardiac remodelling |
··/– |
Acceptable IV and EV  . Poor IV or EV
. Poor IV or EV  . Poor IV and EV
. Poor IV and EV 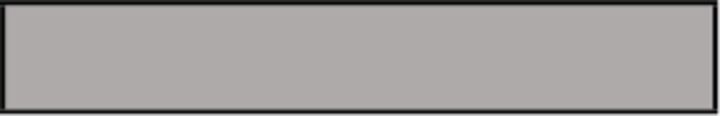 .
.
*Symbols for effect direction: ↑ increased; ↓ decreased; ↕ mixed (indicate statistically significant results were reported, defined as p<0.05); ↔ none (indicates no statistically significant result was reported). If no age group is indicated beside the finding, then all age groups were affected.
†The scoring system used in the risk-of-bias assessment is described in the Methods section.
T2D, type 2 diabetes.
