Abstract
The aim of this study was to determine the rate of venous ulcer recurrence and the level of compliance in patients wearing European class 1 or class 2 compression stockings. A total of 100 patients with healed venous leg ulcers were recruited, and were randomised to either class 1 (n = 50) or class 2 (n = 50) compression stockings. Follow‐up was at 1 week, 3, 6, 9 and 12 months to monitor ulcer recurrence and compliance. Patients had a duplex scan to identify the source of venous incompetence. The rate of ulcer recurrence after 12 months was 16·1%, and the difference in recurrence rate between classes was not statistically significant (P = 0·287) although greater numbers in class 1 developed a recurrence. Participants (88·9%) were compliant; non‐compliant patients were at a significantly greater risk of recurrence (P≤ 0·0001). Thirteen patients had both superficial and deep incompetence; those randomised to class 1 stockings (n = 4) developed ulcer recurrence. Patients with a history of multiple episodes of ulceration were more likely to develop a recurrence (P = 0·001). The lowest venous ulcer recurrence rates were seen in patients who were compliant with hosiery regardless of the compression level. Patients with both superficial and deep incompetence had a lower rate of recurrence with class 2 compression.
Keywords: Compliance, Compression hosiery, Recurrence, Venous leg ulcers
Introduction
Venous leg ulceration is a debilitating, chronic condition affecting 1–2% of the older population; healing venous ulcers can be slow and labour intensive 1, 2. The negative impact of leg ulceration on patients' quality of life and on health care costs is well recognised 3, 4, 5. Multi‐layer compression bandaging remains the gold standard in treating venous leg ulcers 5, 6, 7; however, 12‐month recurrence rates of 26–36% have been reported in the literature 8, 9, 10, 11. The emphasis therefore must be on the most appropriate method of preventing ulcer recurrence. Conservative prevention measures focus on lifelong wearing of compression hosiery and educating the patient to comply with this treatment. The most effective method of preventing ulcer recurrence is superficial venous surgery that has been shown to greatly reduce the incidence of recurrence when combined with compression in those who are suitable and willing to consider surgery 11, 12.
It is accepted that wearing stockings can prove difficult; patients may find them challenging to don and remove, they may not like the sensation of the compression and may not like the appearance of the stockings. It has been the authors' experience that in practice if patients cannot wear/tolerate the prescribed compression stocking then the philosophy of ‘something is better than nothing’ is applied and a reduced level of compression stocking is employed.
Previously published studies investigated the effectiveness of class 2 (18–24 mmHg at the ankle) and class 3 (25–35 mmHg at the ankle) British standard compression stockings in preventing ulcer recurrence 8, 9; however, no study to our knowledge has examined the effectiveness of European hosiery which is the standard compression hosiery used in Ireland and sometimes in the UK. British and European standard stockings differ in the degree of compression exerted on the limb (Table 1). This pilot study aimed to compare the efficacy of European class 1 (18–21 mmHg) and class 2 (23–32 mmHg) compression stockings in preventing ulcer recurrence and to identify patients who benefit from the greatest level of compression. Second, the study aimed to explore factors that affect patient compliance with stocking wear.
Table 1.
Levels of compression hosiery
| The difference in compression levels | ||
|---|---|---|
| British standard | European hosiery | |
| Class 1 | 14–17 mmHg | 18–21 mmHg |
| Class 2 | 18–24 mmHg | 23–32 mmHg |
| Class 3 | 25–35 mmHg | 34–46 mmHg |
Methods
The primary objective of this pilot study was to record the rate of ulcer recurrence in both stocking classes and to determine factors that influence ulcer recurrence. Ulcer recurrence was defined as epithelial breakdown anywhere below the knee of the study leg lasting more than 4 weeks requiring resumption of compression bandaging treatment.
The secondary objectives were first, to identify factors that affect compliance and determine if patients in lighter stockings (class 1) were more compliant with wear and, secondly, identify if wearing compression hosiery negatively affects patients' activities of daily living. Patients from hospital and community leg ulcer clinics in the Mid‐West Area in Ireland with healed venous leg ulcers were invited to participate in this randomised controlled trial. Ethical approval for the study was granted by the Mid‐Western Regional Hospital Complex ethics committee. Written information was provided and once the patient agreed to participate a written consent form was signed. A computer‐generated randomised list was used for randomisation; the results were entered sequentially into numbered, sealed envelopes, which were assigned to consecutive patients once consented. Patients were randomised to either European class 1 (18–21 mmHg) (n = 50) or class 2 (23–32 mmHg) (n = 50) compression stockings once the ulcer had healed. The stockings used were Mediven®; elegance (closed toe) or Mediven®; plus (open toe) (Royale Distributing Agency, Dublin, Ireland). These stockings were chosen as they were commonly prescribed in both hospital and community clinics at the time of study recruitment. Patients were measured for the stockings and given a choice of colour and option of closed or open toe. All patients were educated on stocking wear including the importance of wearing stockings, how to get into and remove them and stocking maintenance. Following randomisation, all patients participating in the study were invited to attend University Hospital Limerick at some stage during the study period, to have a duplex scan of their legs to determine venous incompetence. Patients were followed up at 1 week, 3, 6, 9 and 12 months to monitor for ulcer recurrence, and a questionnaire was completed on compliance and the patients' experience of wearing the stockings. The questionnaire included questions on how often the patients wore the stockings (all day every day – removing at night time, some part of every day, some days, all day and all night); on how easy it was to independently get into and remove the stockings or if they required assistance, and whether wearing the stockings limited their activities of daily living. The patients were also asked to score their overall experience of wearing compression stockings on a visual analogue scale (VAS), ranging from 1 to 10; 1 translating as a very poor experience to 10 relating to excellent. Figure 1 illustrates the questionnaire used.
Figure 1.
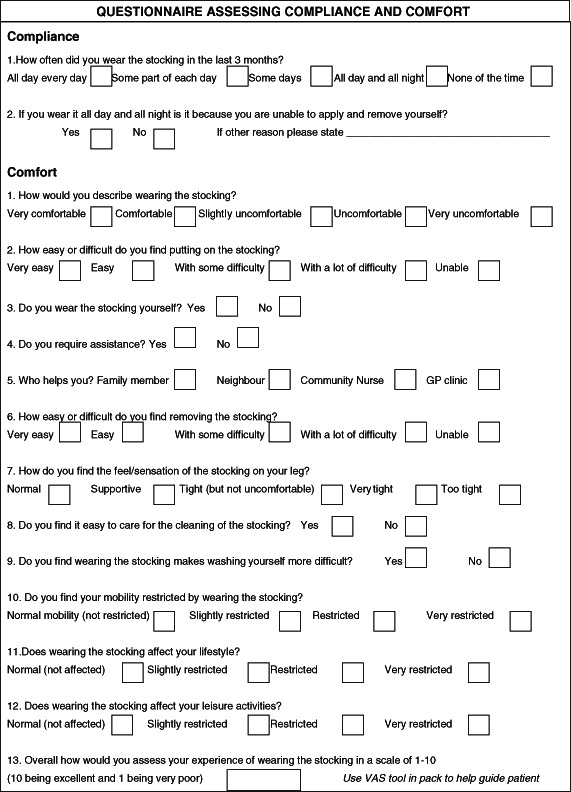
Compliance and comfort questionnaire.
Patients attended a hospital outpatients clinic for review by the vascular team if they wished to consider having superficial venous surgery.
Statistical analysis
Intention‐to‐treat analysis was carried out on data using Statistical Package for Social Sciences (SPSS, version 18). Descriptive statistics were computed on all variables to determine frequencies, means, medians and measures of centrality. Multi‐variable analyses were computed using chi‐squared and Fisher's exact tests. Relative risk was calculated on independent risk factors for recurrence. A P value of <0·05 was considered statistically significant. This study was not blinded.
Results
A total of 100 patients with newly healed venous leg ulcers were recruited into this study. Fifty patients were randomised to wear class 1 and fifty to class 2 stockings. One patient randomised to class 1 was lost to follow‐up and withdrawn from the study analysis. The mean age was 69·3 years (SD = 11·0) there was no statistical difference in mean age between those in class 1 or class 2 groups (69·7 versus 68·9 years, P = 0·71). The majority of participants were fully mobile, 87·8% in class 1 and 90% in class 2, the remaining patients mobilised with an aid. While half (50·5%) of all the study participants had a history of multiple previous venous ulcers, there was no statistical difference between class 1 and class 2 groups for previous ulceration (23 versus 27, P = 0·549). Nine patients (9%), five in class 1 and four in class 2 group, reported having a previous deep vein thrombosis (DVT); 36 patients in each group had visible varicose veins.
There was an overall 12‐month ulcer recurrence rate of 16·1% (n = 16). Of these, ten patients were in class 1 and six in class 2 stockings. There was no statistical difference in the rate of ulcer recurrence between those randomised to class 1 or class 2 stockings (P = 0·287) (Figure 2). Of the 16 patients with ulcer recurrence, 9 were diagnosed with superficial venous disease, (6 in class 2 and 3 in class 1 groups). Four patients had both superficial and deep venous incompetence; all were in the class 1 group. One scan was incomplete as the deep veins could not be visualised due to obesity and two of the ulcer recurrence patients were unwilling to have a scan done.
Figure 2.
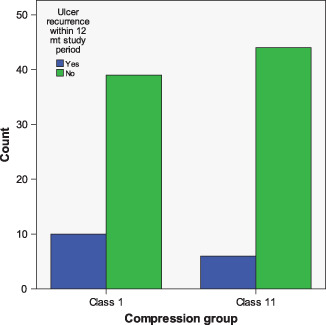
Twelve‐month ulcer recurrence rates.
Superficial and deep incompetence was diagnosed in 13 patients, of these only those in class 1 stockings developed ulcer recurrence. There was no significant difference between those in class 1 or class 2 stockings who had a history of multiple ulcer recurrence and went on to develop a new ulcer (eight and six patients developed recurrence, respectively). However, patients with a history of multiple episodes of ulceration were more likely to develop a new ulcer (RR = 6·86, P = 0·001).
In total, 11 (11·1%) study patients did not adhere to wearing the prescribed compression hosiery; 7 of these developed a new ulcer within the 12‐month period. The four patients who did not wear stockings and did not develop a new ulcer were all diagnosed as having superficial incompetence. The likelihood of developing an ulcer when not wearing stockings was highly significant when compared with those compliant with compression hosiery wear (RR = 6·22, P = <0·0001). There was no significant difference in rates of compliance between groups (P = 0·760). Table 2 details the reasons for non‐compliance. When the analysis was repeated to compare recurrence rates among those actually adhering to wearing stockings (n = 43 in class 1, n = 45 in class 2), rates of recurrence were not statistically different; there were six new ulcers in the class 1 group and three in the class 2 group (P = 0·309).
Table 2.
Reason for hosiery non‐compliance n = 11
| Reason for non‐compliance | Number | Class of stocking | Recurrence |
|---|---|---|---|
| Unable to tolerate tightness | n = 2 | Class 2 | n = 1 |
| Unable to apply/remove | n = 2 | Class 1 | |
| n = 2 | Class 2 | n = 1 | |
| Skin sensitivity | n = 2 | Class 1 | n = 2 |
| n = 1 | Class 2 | n = 1 | |
| Unwilling to wear hosiery | n = 2 | Class 1 | n = 2 |
Of those stocking wearers (n = 88), compliance with recommended daily duration of stocking wear was high with 75% at 3 months reporting wearing stockings ‘all day every day’. This reduced to 65% at 12 months. However, this figure also includes those not in compression due to recurrence (n = 6). There was no statistically significant difference between the two groups in compliance at either 3 or 12 months (P = 0·179 and 0·564, respectively). Two patients reported wearing the stockings ‘all day and all night' due to difficulty in getting into and removing stockings, and depend on a family member to change the stockings.
The ability of the patient to wear the stocking themselves was reported as 67% at 3 months and 73% at 12 months; there was no statistical difference between groups. The activities of daily living were not limited in either group by wearing compression hosiery. Overall, VAS mean score of patients' experience wearing compression stockings was reported as 7·47 at 3 months and 7·30 at 12 months; there was no significant difference between groups at each time interval.
Seven patients underwent superficial venous surgery. Results of the duplex report showed that a further 76 patients had either superficial or superficial and deep venous incompetence, and may have been suitable for surgery but did not proceed this route.
Discussion
There is a high incidence of recurrence among patients with venous ulcers. This study has shown that just over half of the study participants had a history of multiple previous ulcers while others have reported that up to 60% of all venous ulcers receiving treatment are recurrent (12). The rates of recurrence increase as time from healing becomes more distant (13). The 12‐month recurrence rate of 16·3% reported in this study is favourably low when compared with other studies 8, 9, 10, 11. This is most likely due to the support given to patients participating in the study in the form of the 3 monthly follow‐up checks. The regular patient contact may have increased compliance and hence reduced the rates of recurrence. This highlights the need for ongoing patient education and support in the form of stocking clinics once a patient's ulcer is healed. The lack of significance in recurrence rates among those in class 1 or class 2 stockings may be due to a type II error as the sample size may not have been sufficiently large to detect significance between the two groups. However, as the greater percentage of recurrences was among those in lighter compression, it would indicate that patients should be prescribed the highest level of compression stocking they can get into and tolerate. Patients who were not compliant with compression stockings were at a much greater risk of developing a new ulcer. This highlights the importance of education in informing patients of the reasons for continued compression and the need for community support for those who are unable to independently put on or remove the stockings.
All patients with both deep and superficial incompetence wearing class 1 stockings (n = 4) developed a new ulcer. These patients are an important sub‐group of healed venous ulcer patients for whom class 1 stockings are unlikely to confer protection against recurrence.
Although surgery has been shown to significantly reduce rates of recurrence 11, 12, the findings of this study showed that patients may be reluctant to have surgery, with only 7·1% having superficial venous surgery. The reason for this may be linked to the older age profile of this group and their own reticence towards any type of surgery. Alternatively, perhaps surgery is not being routinely discussed as an option for patients with healed venous ulcers and a change in protocol to routinely offer patients a vascular consultation to discuss surgery should be considered. Further research into the reasons for the low uptake on superficial venous surgery identified in this study is planned.
The differences in compression levels among British and European stockings are a source of concern and require awareness among practitioners and clinicians, so that the correct level of compression is prescribed. The findings of this study identified that there may be sub groups of patients who require greater levels of compression; in this study, patients with both superficial and deep incompetence were identified as a group for whom class 1 did not appear to generate enough pressure to prevent ulcer recurrence. It is important therefore that practitioners be mindful of the differences in available stockings and to check the compression level generated rather than the stocking classification. Compression hosiery in USA are not identified by compression class and instead are descriptively labelled with the levels of pressure generated, for example, moderate support 20–30 mmHg. Perhaps the compression hosiery industry should consider standardising such a labelling system for British and European hosiery to reduce the risk of inadequate compression being prescribed and inadvertently increasing the risk of ulcer recurrence.
Patients should be offered the highest level of compression hosiery they can comply with; the higher the level of compression the less likely an ulcer recurrence.
The old adage of ‘something is better than nothing’ is true when it comes to compression hosiery to prevent ulcer recurrence. This study found that patients wearing compression stockings are significantly less likely to develop a new ulcer than those who do not wear any form of compression. The higher the level of compression the less likely an ulcer recurrence, and those diagnosed with both superficial and deep incompetence require the greatest level of compression.
References
- 1. Clarke‐Moloney M , Keane N , Kavanagh E. Changes in leg ulcer management practice following training in an Irish community setting. J Wound Care 2008. ; 17 : 116 – 21. [DOI] [PubMed] [Google Scholar]
- 2. O'Brien JF , Grace PA , Perry IJ , Burke PE. Prevalence and aetiology of leg ulcers in Ireland. Ir J Med Sci 2000. ; 169 : 110 – 2. [DOI] [PubMed] [Google Scholar]
- 3. Ragnarson‐Tennvall G , Hjelmgren J. Annual costs of treatment for venous leg ulcers in Sweden and the United Kingdom. Wound Repair Regen 2005. ; 13 : 13 – 8. [DOI] [PubMed] [Google Scholar]
- 4. Charles H. Does leg ulcer treatment improve patients' quality of life? J Wound Care 2004. ; 13 : 209 – 13. [DOI] [PubMed] [Google Scholar]
- 5. Clarke‐Moloney M , O'Brien JF , Grace PA , Burke PE. Health‐related quality of life during four‐layer compression bandaging for venous ulcer disease: a randomised controlled trial. Ir J Med Sci 2005. ; 174 : 21 – 5. [DOI] [PubMed] [Google Scholar]
- 6. Moffatt CJ , Franks PJ , Oldroyd M , Bosanquet N , Brown P , Greenhalgh RM , McCollum CN. Community clinics for leg ulcers and impact on healing. BMJ 1992. ; 305 : 1389 – 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ghauri ASK , Taylor MC , Deacon JE , Whyman MR , Earnshaw JJ , Heather BP , Poskitt KR. Influence of a specialised leg ulcer service on management and outcome. Br J Surg 2000. ; 87 : 1048 – 56. [DOI] [PubMed] [Google Scholar]
- 8. Franks PJ , Oldroyd MI , Dickson D , Sharp E , Moffatt C. Risk factors for leg ulcer recurrence: a randomised trial of two types of compression stocking. Age Aging 1995. ; 24 : 490 – 4. [DOI] [PubMed] [Google Scholar]
- 9. Nelson EA , Harper D , Prescott R , Gibson B , Brown D , Ruckley V. Prevention of recurrence of venous ulceration: Randomised controlled trial of class 2 and class 3 elastic compression. J Vas Surg 2006. ; 44 : 803 – 8. [DOI] [PubMed] [Google Scholar]
- 10. Nelson EA , Bell‐Syer SEM , Cullum NA. Compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev 2000. ; 4 : Art. No. CD002303. [DOI] [PubMed] [Google Scholar]
- 11. Barwell JR , Davies CE , Deacon J , Harvey K , Minor J , Sassano A , Taylor M , Usher J , Wakely C , Earnshaw JJ , Heather BP , Mitchell DC , Whyman MR , Poskitt KR. Comparison of surgery and compression with compression alone in chronic venous ulceration (ESCHAR study): randomised controlled trial. Lancet 2004. ; 363 : 1854 – 9. [DOI] [PubMed] [Google Scholar]
- 12. Gohel MS , Barwell JR , Taylor M , Chant T , Foy C , Earnshaw JJ , Heather BP , Mitchell DC , Whyman MR , Poskitt KR. Long term results of compression therapy alone versus compression plus surgery in chronic venous ulceration (ESCHAR): randomised controlled trial. BMJ 2007. ; 335 : 83 – 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vowden KR , Vowden P. Preventing venous ulcer recurrence: a review. Int Wound J 2006. ; 3 : 11 – 21. [DOI] [PMC free article] [PubMed] [Google Scholar]


