Abstract
A middle-aged man with obstructive sleep apnea who had been treated with continuous positive airway pressure developed COVID-19. An analysis of airflow records from the continuous positive airway pressure machine revealed a rise in his respiratory rate on the night before the onset of COVID-19-related symptoms, while his nocturnal respiratory rate had been stable during the 18-month period prior to the presently reported episode. The present case suggests that a rise in respiratory rate detected using continuous positive airway pressure machine data could be an important sign of impending acute illness, such as COVID-19. Studies to elucidate the usefulness of this method are warranted.
Citation:
Nakano H, Kadowaki M, Furukawa T, Yoshida M. Rise in nocturnal respiratory rate during CPAP may be an early sign of COVID-19 in patients with obstructive sleep apnea. J Clin Sleep Med. 2020;16(10):1811–1813.
Keywords: COVID-19, CPAP, obstructive sleep apnea, respiratory rate
INTRODUCTION
The COVID-19 pandemic has had a tremendous impact on the world. Many subjects with obstructive sleep apnea (OSA) can develop this disease. OSA and severe COVID-19 do share common risk factors including obesity, cardiovascular disease, diabetes mellitus, and hypertension.1,2 Meanwhile, continuous positive airway pressure (CPAP) therapy, which is the gold standard treatment for moderate to severe OSA, can shed viruses from patients into their local environment, endangering others living with them.3 Therefore, early detection of COVID-19 is desirable for OSA subjects.
Most current CPAP machines record airflow data from the flow sensor incorporated into the machine and store it either on a Secure Digital memory card and/or in cloud storage. Recently, we treated a patient with OSA whose CPAP flow data contained an important sign that could potentially be utilized for the early detection of COVID-19.
REPORT OF CASE
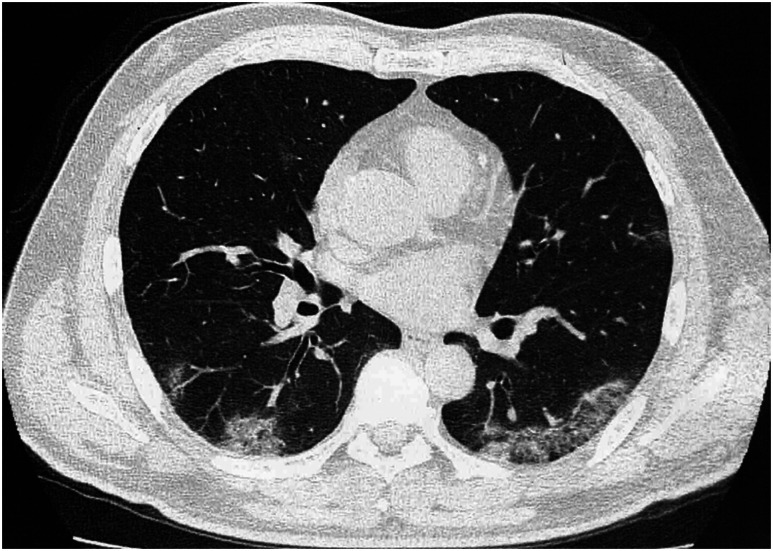
A 64-year-old man with severe OSA who had been receiving CPAP therapy for 5 years presented with flu-like symptoms that had begun 5 days before. He had noticed a fever (temperature, 38.5°C) in the afternoon 4 days before visiting our clinic. His symptoms included diarrhea and fatigue, followed by loss of the sensations of taste and smell and shortness of breath. At the time of his presentation at our clinic, a physical examination revealed a body temperature of 37.2°C, a pulse rate of 88/min, an SpO2 of 98%, and no audible adventitious lung sounds. Blood tests indicated the presence of a mild inflammation (white blood cells, 8240/mm3; C-reactive protein, 3.28 mg/dL). Although chest X-ray findings were normal, a computed tomography examination of the chest revealed bilateral peripheral infiltrates (Figure 1), consistent with COVID-19 pneumonia. A nasopharyngeal swab test for COVID-19 polymerase chain reaction was performed. The next day, a positive result was received, and the patient was admitted to a designated hospital for COVID-19. CPAP use was discontinued on the second hospital day, at which time his condition deteriorated slightly and he required supplemental oxygen administration. He recovered relatively quickly, and the oxygen therapy was discontinued on the fifth hospital day.
Figure 1. Computed tomography of the chest showing bilateral peripheral infiltrates.
Analysis of CPAP machine records
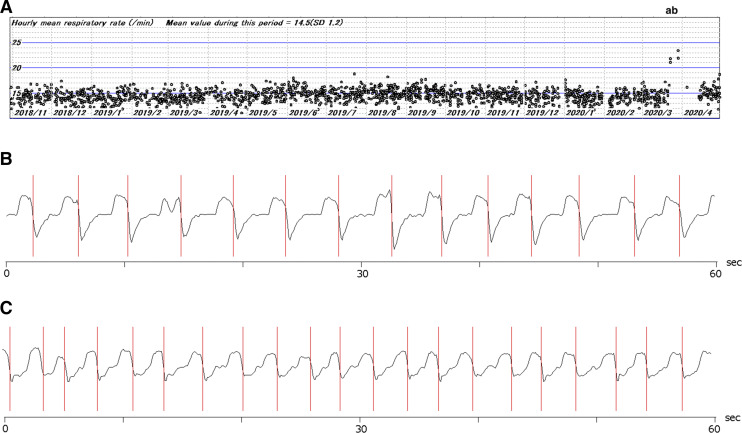
The patient had been using a CPAP machine (DreamStation AutoCPAP; Philips Respironics, Murrysville, PA) since October 2018. All of the data stored in the Secure Digital memory card was downloaded, and the hourly mean respiratory rate was calculated from the flow rate data files using a custom-made computer program (CpapAnal.exe, written by Hiroshi Nakano) (Figure 2). The program detects the end of inspiratory phase from appropriately filtered flow rate signal using zero-crossing method. The program was written in C++ language using Microsoft Visual Studio 2019. The validity of the computer analysis was confirmed by visual analysis of the raw flow rate data. The mean respiratory rate during the 18-month period prior to the present episode was 14.5/min (standard deviation, 1.2). On the night before the onset of his symptoms, the patient’s mean respiratory rate increased to 21 22/min, which was sustained until the night of admission.
Figure 2. Respiratory rate obtained from CPAP flow records.
(A) The hourly respiratory rates for an 18-month period had been stable until 2 days before the onset of symptoms. A sudden surge in the respiratory rate (A) occurred on the night before the day of symptom onset. The increase in the respiratory rate was sustained until the night when the patient was admitted to hospital (B). His adherence to CPAP deteriorated, and he began receiving supplemental oxygen therapy after hospital admission. (B and C) Examples of raw flow rate trace for 60 seconds from the CPAP machine on a usual night (B) and at “a” (C). The vertical lines indicate the end-inspiratory points that were detected by the computer program and used to obtain the respiratory rate.
DISCUSSION
We report a patient with OSA in whom an increased respiratory rate detected using CPAP flow rate data suggested the onset of COVID-19 disease.
Respiratory rate is known to be an important vital sign, together with pulse rate, blood pressure, and body temperature. An increased respiratory rate is known to be an early sign of a lower respiratory infection in elderly patients.4 Regarding COVID-19 disease, a high respiratory rate (≥ 30/min) is regarded as a sign defining the presence of severe disease.5 There have not been any reports describing the respiratory rate during the early stage of COVID-19 disease. One study reported that 37 out of 55 asymptomatic subjects with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection had computed tomography evidence of pneumonia.6 Therefore, not only a heightened body temperature, but also early lung involvement can cause an increased respiratory rate during the early stage of this disease.
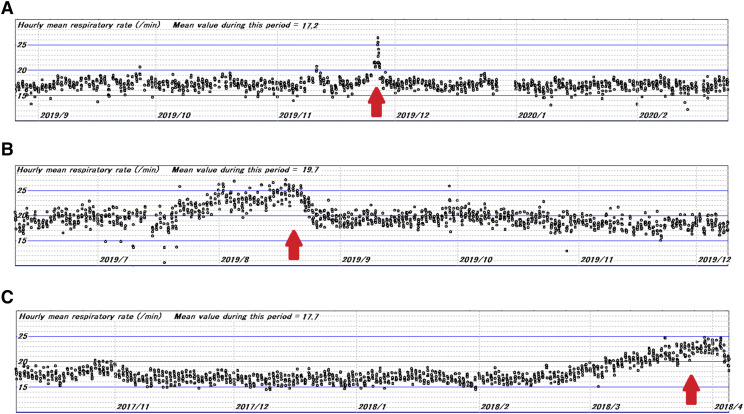
The exact measurement of respiratory rate is not always easy in clinical practice.7 Respiration itself can be perturbed in response to situations where it is being counted. In contrast, the respiratory rate while one is asleep is stable and reliable. A recent study reported that the mean nocturnal respiratory rate can predict cardiovascular and all-cause mortality in community-dwelling older people.8 Recent typical CPAP machines can record the flow rate measured using a flow sensor at a sampling frequency of 25 Hz (ResMed Sleepmate 10; San Diego, CA) or 5 Hz (DreamStation AutoCPAP) every night for more than 3 years. Obtaining the respiratory rate from these flow rate records is not difficult. We have developed software (CpapAnal.exe) for this purpose. In our experience, a significant rise in respiratory rate was observed in many patients experiencing acute changes in health status. The pattern seemed different according to the course of the illness (Figure 3). We believe that the respiratory rate from CPAP machines could provide important information for early recognition of a change in the user’s health status. We hope that the CPAP vendors provide an option in their software for obtaining more detailed information, including long-term respiratory rate trends.
Figure 3. Examples of respiratory rate trends over 6-month period obtained from CPAP flow records.
Patients being treated for severe OSA experienced an acute illness during the treatment periods. Arrows indicate the day when the patients sought medical attention. The illnesses were diagnosed as (A) influenza, (B) bacterial pneumonia, and (C) acute exacerbation of chronic interstitial pneumonia. CPAP machines used were DreamStation AutoCPAP (A and B) and Sleepmate 10 (C).
CONCLUSIONS
The analysis of CPAP machine data can yield the nocturnal respiratory rate. The present case suggests that an increased respiratory rate might be an early sign of COVID-19 disease. Studies to elucidate the usefulness of this method are warranted.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. The authors declare no conflicts of interest.
ABBREVIATIONS
- CPAP
continuous positive airway pressure
- OSA
obstructive sleep apnea
REFERENCES
- 1.Du R-H, Liang L-R, Yang C-Q, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5):2000524. 10.1183/13993003.00524-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lighter J, Phillips M, Hochman S, et al. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin Infect Dis. 2020, ciaa415, 10.1093/cid/ciaa415. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kryger MH, Thomas R. Home PAP devices in patients infected with COVID-19. J Clin Sleep Med. 2020;16(7):1217–1219. 10.5664/jcsm.8490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McFadden JP, Price RC, Eastwood HD, Briggs RS. Raised respiratory rate in elderly patients: a valuable physical sign. Br Med J (Clin Res Ed). 1982;284(6316):626–627. 10.1136/bmj.284.6316.626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 6.Wang Y, Liu Y, Liu L, Wang X, Luo N, Li L. Clinical outcomes in 55 patients with severe acute respiratory syndrome coronavirus 2 who were asymptomatic at hospital admission in Shenzhen, China. J Infect Dis. 2020;221(11):1770–1774. 10.1093/infdis/jiaa119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takayama A, Takeshima T, Nakashima Y, Yoshidomi T, Nagamine T, Kotani K. A comparison of methods to count breathing frequency. Respir Care. 2019;64(5):555–563. 10.4187/respcare.06451 [DOI] [PubMed] [Google Scholar]
- 8.Baumert M, Linz D, Stone K, et al. Mean nocturnal respiratory rate predicts cardiovascular and all-cause mortality in community-dwelling older men and women. Eur Respir J. 2019;54(1):1802175. 10.1183/13993003.02175-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]