Abstract
Background.
Reducing inappropriate antibiotic prescriptions (Rxs) is a major quality improvement initiative in the United States. Tracking antibiotic prescribing trends is 1 method of assessing improvement in antibiotic prescribing. The purpose of this study was to assess longitudinal antibiotic prescribing practices among dental specialists.
Methods.
This was a retrospective ecological longitudinal trend study. The authors calculated monthly systemic antibiotic Rx counts, and rates per 100,000 beneficiaries, from a pharmacy benefits manager in the United States from 2013 through 2015. The authors calculated average annual antibiotic Rx rates (AARs) for the 3-year study period. The authors used a quasi-Poisson regression model to analyze antibiotic Rx trends. The authors quantified seasonal trends, when present, via peak-to-trough ratios (PTTRs).
Results.
Dental specialists prescribed 2.4 million antibiotics to the cohort of 38 million insurance beneficiaries during the 3-year study period (AAR = 2,086 Rxs per 100,000 beneficiaries). Oral and maxillofacial surgeons prescribed the most antibiotics (1,172,104 Rxs; AAR = 1,018 Rxs per 100,000 beneficiaries), followed by periodontists (527,038 Rxs; AAR = 457 Rxs per 100,000 beneficiaries), and endodontists (447,362 Rxs; AAR = 388 Rxs per 100,000 beneficiaries). Longitudinal antibiotic prescribing trends were stable among all dental specialties in the regression models (P > .05). The authors observed substantial seasonal variation in antibiotic Rxs in 2 specialties: pediatric dentistry (PTTR, 1.18; 95% confidence interval, 1.13 to 1.25) and orthodontics and dentofacial orthopedics (PTTR, 1.41; 95% confidence interval, 1.21 to 1.71), with the highest rates of antibiotic Rxs in the spring and winter.
Conclusions.
Antibiotic prescribing practices for dental specialists remained stable. The authors observed seasonal trends in 2 specialties.
Practical Implications.
Public health efforts are needed improve antibiotic prescribing among dental specialties.
Keywords: Dental public health, epidemiology, antimicrobials, antimicrobial resistance, bacteria, infectious diseases
The systematic approach to improving antibiotic prescribing has been termed antibiotic (or antimicrobial) stewardship. Antibiotic stewardship improves the safety and quality of patient care, while reducing health care costs and combating the spread of antibiotic-resistant infections.1 The Centers for Disease Control and Prevention (CDC) has provided implementation tool kits for antibiotic stewardship programs in hospital, clinic, and nursing home settings.2 Each tool kit recommends tracking and improving antibiotic use. Ideally, this would be accomplished with a thorough evaluation of the appropriateness of each antibiotic prescription (Rx). Realistically, many antibiotic stewardship programs focus on evaluating antibiotic Rx trends over time for a subset of specific conditions or for commonly prescribed antibiotics.
Tracking national antibiotic prescribing trends is 1 method used to determine whether providers are improving antibiotic prescribing behavior over time.3 Overall antibiotic prescribing should decrease over time, given that the CDC estimates that 30% of outpatient antibiotic Rxs are unnecessary.4 However, it is unclear whether public health efforts to improve antibiotic prescribing are affecting health care providers. Findings from 1 study among all health care providers revealed modest reductions in overall antibiotic use over time,5 whereas findings from another revealed no change.6 Tracking antibiotic prescribing trends among all providers also can show some temporal trends. For example, overall antibiotic prescribing rates are higher during winter months.5,6 This finding is thought to be related to inappropriate antibiotic treatment of viral upper respiratory tract infections, which are more common in the winter months.5,6
Although dentists are responsible for approximately 10% of outpatient antibiotic Rxs, few study investigators have evaluated antibiotic prescribing trends among dentists. Authors of 2 articles identified that general dentists prescribe several antibiotics that have no clear dental indications or activity against dental pathogens.7,8 Authors of 1 longitudinal analysis evaluated antibiotic Rx trends of general dentists and found that overall antibiotic prescribing remained unchanged from 2013 through 2015.9 However, investigators from studies in Canada,10 Australia,11 and the Czech Republic12 reported increased dental antibiotic prescribing.
To our knowledge, no study investigators have investigated longitudinal antibiotic prescribing trends among US dental specialists. This investigation is important because dental specialists, despite being a relatively small group of care providers, are responsible for approximately 27% of dental antibiotic Rxs.8 Our aim in this study was to characterize longitudinal antibiotic prescribing patterns within a US national pharmacy benefits manager.
METHODS
We analyzed data on outpatient antibiotic Rxs written by dental specialists from January 1, 2013, through December 31, 2015. We obtained the data from Express Scripts Holding Company (ESHC), the largest pharmacy benefits manager in the United States. The data included the oral health care provider’s American Dental Association (ADA) recognized specialty, his or her location, the prescribed antibiotic’s name and dose, and the number of days’ antibiotic supply (treatment duration). We included data on antibiotic prescribing by general dentists as a reference. We removed Rx claims for members with missing or duplicate information because these are errors within the database. According to the standard protocol within ESHC, we excluded reversed (unfilled) Rx claims from the analysis. These Rxs are less than 4% of claims within the database. We also excluded topical antibiotics, systemic or topical antifungals, antiparasitics, and antivirals. We combined antibiotics with the same active ingredient but a different formulation (for example, extended-release tablets). We included antimicrobials with antibacterial properties (for example, methenamine).
We analyzed the count of antibiotics prescribed by all oral health care providers and stratified the result according to dental specialty. We also obtained the number of Rxs and the total number of beneficiaries in the database. We summed the number of Rxs in each provider category. We also calculated the average annual Rx (AAR) per provider and per 100,000 beneficiaries.
We used quasi-Poisson regression models by using the calendar month during the study period (January 2013 through December 2015) as the independent variables to evaluate antibiotic prescribing trends for each dental specialty; we considered P values less than .05 statistically significant. We explored locally weighted scatterplot smoothing regression models to visualize nonlinear trends.
When we identified nonlinear trends in antibiotic prescribing, we assessed these trends by fitting log-linear Poisson regression models to monthly data by using a method we have described previously.6 We then calculated the magnitude of seasonal variations via peak-to-trough ratios (PTTRs), which are interpreted as a relative risk, with the trough month as the reference level. This calculation provides additional flexibility in the patterns of seasonal variation and helps adjust for secular trend bias. Christensen and colleagues13 have published a detailed description of PTTRs. Furthermore, we stratified nonlinear overall prescribing trends according to the antibiotic prescribed to explore which specific antibiotics were driving the seasonal variation. We used the top 5 most commonly prescribed antibiotics (amoxicillin, azithromycin, cephalexin, clindamycin, and penicillin) for stratified seasonal analyses. We performed all analyses with software (R, Version 3.4.4, R Foundation for Statistical Computing). Washington University’s Human Research Protection Office approved this study.
RESULTS
Antibiotic use
Over the 3-year study period, dental specialists were responsible for more than 2.4 million antibiotic Rxs (AAR, 2,086 Rx/100,000 beneficiaries) compared with more than 6.4 million Rxs for general dentists (Table 1). Dental specialties prescribing the most antibiotics over the study period were oral and maxillofacial surgery (1,172,2014 Rxs; AAR, 1,018 Rx/100,000 beneficiaries), periodontics (527,038 Rxs; AAR, 457 Rxs/100,000 beneficiaries), and endodontics (447,362 Rxs; AAR, 388 Rxs/100,000 beneficiaries). These specialties accounted for almost 90% of antibiotic Rxs among dental specialists in this cohort.
Table 1.
Number of antibiotics prescribed by dental specialists and rate per 100,000 beneficiaries* from January 2013 through December 2015, United States.
| DENTAL DISCIPLINE/SPECIALTY | 2013 | 2014 | 2015 | TREND P VALUE† | |||
|---|---|---|---|---|---|---|---|
| No. of Rxs‡/ No. of Providers (Rx Rate§) | Rate per 100,000 Beneficiaries | No. of Rxs/ No. of Providers (Rx Rate) | Rate per 100,000 Beneficiaries | No. of Rxs/ No. of Providers (Rx Rate) | Rate per 100,000 Beneficiaries | ||
| General Dentistry¶ | 2,151,729/132,495 (16) | 5,596 | 2,149,859/133,126 (16) | 5,455 | 2,133,384/133,382 (16) | 5,707 | .512 |
| Total: Specialties Summary | 803,916/22,837 (35) | 2,091 | 799,497/22,658 (35) | 2,029 | 799,102/22,080 (36) | 2,138 | .802 |
| Dental Public Health | 5,730/455 (13) | 15 | 5,639/442 (13) | 14 | 5,457/444 (12) | 15 | .947 |
| Endodontics | 151,339/4,338 (35) | 394 | 148,184/4,304 (34) | 376 | 147,839/4,204 (35) | 395 | .883 |
| Oral and Maxillofacial Pathology | 31,591/433 (73) | 82 | 30,285/421 (72) | 77 | 30,580/404 (76) | 82 | .968 |
| Oral and Maxillofacial Radiology | 576/10 (58) | 2 | 618/10 (62) | 2 | 601/10 (60) | 2 | .937 |
| Oral and Maxillofacial Surgery | 387,625/5,730 (68) | 1,008 | 390,423/5,638 (69) | 991 | 394,056/5,506 (72) | 1,054 | .246 |
| Orthodontics and Dentofacial Orthopedics | 3,768/1,308 (2.9) | 10 | 3,729/1,303 (2.9) | 10 | 3,294/1,198 (2.7) | 9 | .784 |
| Pediatric Dentistry | 26,942/4,304 (6.3) | 70 | 26,646/4,305 (6.2) | 68 | 25,847/4,207 (6.1) | 69 | .802 |
| Periodontics | 178,117/4,466 (40) | 463 | 175,830/4,435 (40) | 446 | 173,091/4,328 (40) | 463 | .915 |
| Prosthodontics | 18,228/1,793 (10) | 47 | 18,143/1,800 (10) | 46 | 18,337/1,779 (10) | 49 | .850 |
Beneficiaries were from Express Scripts Holding Company.
The authors analyzed trends via monthly quasi-Poisson regression models.
Rx: Prescription.
Rx rate: Express Scripts Holding Company prescription rate per dental care provider. Both the total prescription rate per provider and the total prescription rate per 100,000 beneficiaries were calculated as mean per year.
The authors used general dentistry as a reference group for comparison purposes.
Trends in antibiotic use
Overall rates of antibiotic Rxs remained stable in each of the 9 dental specialties analyzed (eFigures 1–10, available online at the end of this article, Table 1). Although all specialties had stable secular trends, results from locally weighted scatterplot smoothing regression analyses revealed that both orthodontists and pediatric dentists had recurring peaks and troughs over the study period (eFigures 4 and 8, available online at the end of this article). Specifically, peaks appeared in January for both specialties, and troughs occurred near July for orthodontists and August and September for pediatric dentists.
We further quantified the seasonal variation in antibiotic prescribing among orthodontists and pediatric dentists by using log-linear Poisson regression models with autoregressive integrated moving average error terms. Pediatric dental antibiotic Rxs had a PTTR of 1.18 (95% confidence interval, 1.13 to 1.25) (Figure 1A, Table 2), whereas orthodontic antibiotic Rxs had a PTTR of 1.41 (95% confidence interval, 1.21 to 1.71) (Figure 2A, Table 2). Azithromycin was the antibiotic with the highest PTTRs for both pediatric dentists (Figure 1B, Table 2) and orthodontists (Figure 2B, Table 2); however, several other antibiotics had seasonal variation as well (data not shown).
Figure 1.
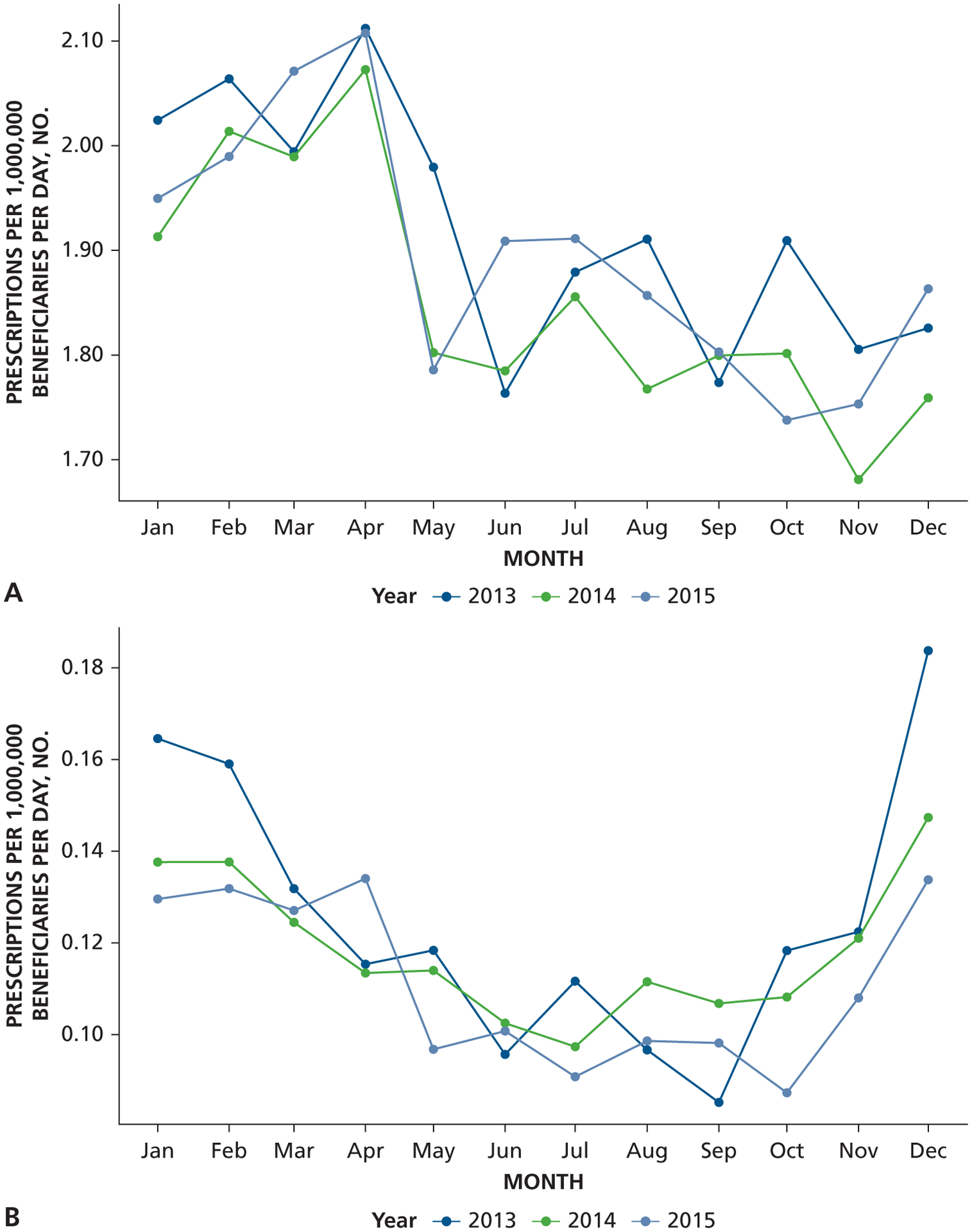
Monthly variation of rate of antibiotic use in pediatric dentistry from January 2013 through December 2015, United States. A. Overall antibiotic use. B. Azithromycin use. Stratified antibiotic prescribing rates are lower than overall antibiotic prescribing rates.
Table 2.
Estimates of seasonal variation in pediatric dentistry and orthodontic and dentofacial orthopedics antibiotic prescriptions expressed as peak-to-trough ratio from January 2013 through December 2015, United States.
| DENTAL SPECIALTY | ANTIBIOTIC* | PEAK-TO-TROUGH RATIO (95% CONFIDENCE INTERVAL) | PEAK MONTH | TROUGH REFERENCE MONTH |
|---|---|---|---|---|
| Pediatric Dentistry | All antibiotics | 1.18 (1.13 to 1.25) | April | November |
| Azithromycin | 1.55 (1.30 to 2.05) | December | July | |
| Orthodontics and Dentofacial Orthopedics | All antibiotics | 1.41 (1.21 to 1.71) | January | July |
| Azithromycin | 2.65 (1.89 to 4.57) | December | July |
Confidence intervals generally are reported, rather than P values, for peak-to-trough calculations; the authors considered confidence intervals that do not include 1 as statistically significant.
Figure 2.
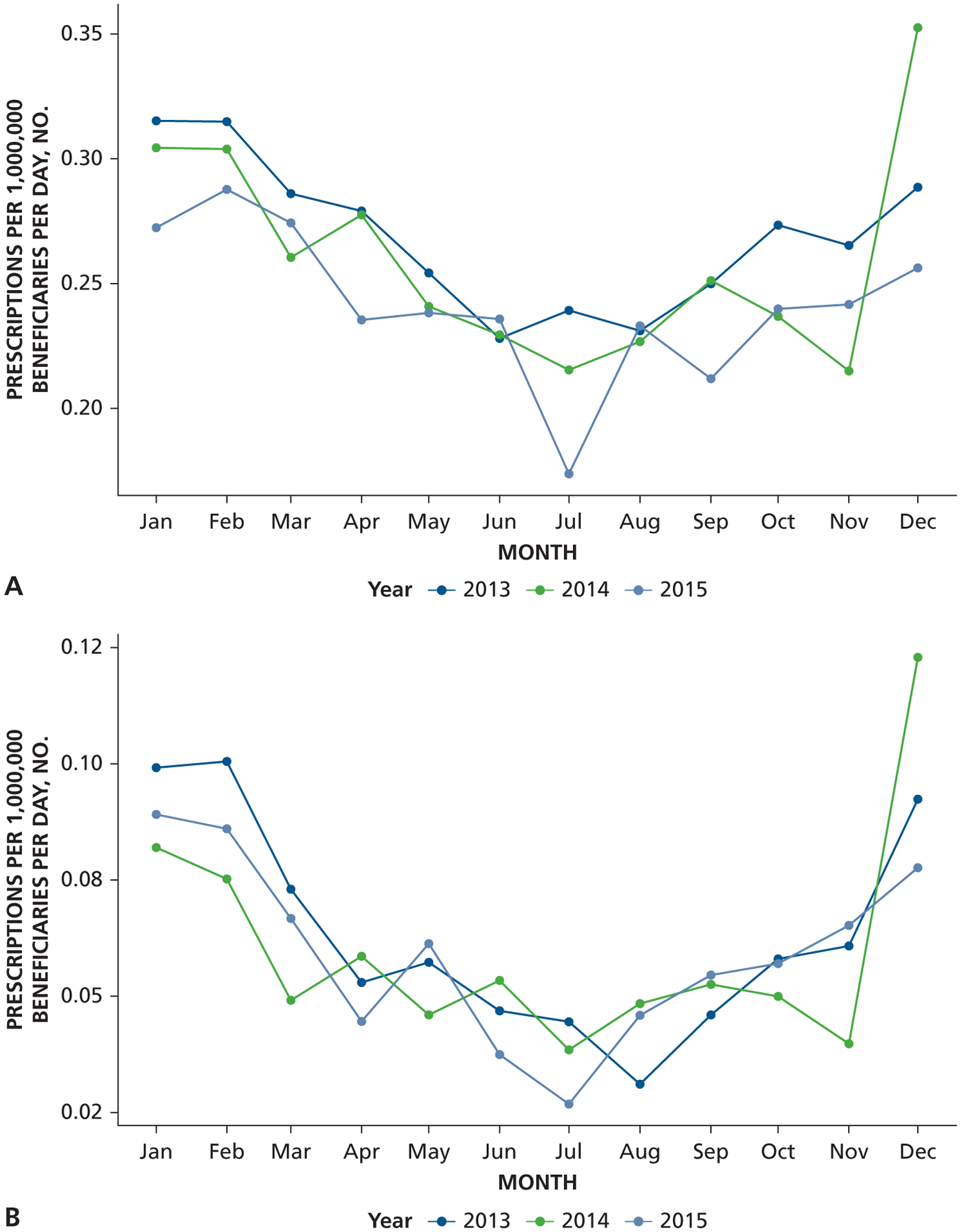
Monthly variation of rate of antibiotic use in orthodontics and dentofacial orthopedics from January 2013 through December 2015, United States. A. Overall antibiotic use. B. Azithromycin use. The y-axis is lower for orthodontic antibiotic prescriptions than for pediatric antibiotic prescriptions because orthodontists prescribe fewer antibiotics than do pediatric dentists.
DISCUSSION
We found that among the 9 dental specialties recognized by the ADA that we included in our study, antibiotic prescribing rates remained stable from January 2013 through December 2015. These findings were not surprising, given stable antibiotic prescribing practices among general dentists reported during the same time frame.9 However, our findings are still important. To our knowledge, this is the first longitudinal analysis of antibiotic prescribing trends for dental specialists in the United States.
Limited data exist for antibiotic prescribing among dental specialists. Results from a 2017 scoping review of 118 studies in which the investigators evaluated dental antibiotic prescribing showed that investigators in most studies focused on antibiotic prescribing among all oral health care providers or general dentists within a region.14 Of all of the included studies, only 9 were dedicated to dental specialty groups.15–23 The specialties included oral and maxillofacial surgery (n = 4),16,20,21,23 endodontics (n = 2),15,18 pediatric dentistry (n = 2),17,19 and periodontics (n = 1)22; no studies were focused on dental public health, oral and maxillofacial pathology, oral and maxillofacial radiology, orthodontics and dentofacial orthopedics, or prosthodontics. Furthermore, 8 of the 9 studies were cross-sectional surveys, which prevents evaluation of antibiotic prescribing trends over time.15–22
Despite the limitations, previous studies of antibiotic prescribing patterns among dental specialists had important findings. In 1 study of pediatric dentists, 30% reported prescribing antibiotics for a prolonged duration (10 days), and 15% reported prescribing antibiotics for dental pain.19 In another study of pediatric dentists, only 28% of antibiotic Rxs were adherent to clinical practice guidelines.17 In a national survey of endodontists in 2002, researchers found modest improvements in antibiotic prescribing for some conditions, but other conditions had no improvement in 25 years.18 Among studies in which the investigators evaluated oral surgeons in Spain, researchers found that 39% would prescribe antibiotics for extractions taking less than 5 minutes; postoperative antibiotic duration varied from 2 through 8 days.21 In a study of antibiotic prescribing among periodontists, 44% reported that they prescribed postoperative antibiotics after an implant placement.22 These data suggest substantial heterogeneity in antibiotic prescribing among dental specialists and substantial opportunities for improvement.
Historically, most public health efforts during the study period were focused on improving antibiotic prescribing among physicians. Since the early 2000s, the CDC has been engaged in educational campaigns to raise awareness of antibiotic resistance and improve antibiotic prescribing practices in physicians’ offices. In 2018, the CDC published guidance for antimicrobial stewardship programs in outpatient settings.24 The American Board of Internal Medicine Foundation also has partnered with multiple medical professional organizations to release antibiotic stewardship clinical practice recommendations via the Choosing Wisely initiative.25
Several free antibiotic stewardship educational materials for dentists and dental specialists are available. For example, the CDC provides an easy-to-use checklist for antibiotic prescribing in dentistry26 and a table of clinical tips for antibiotic prescribing for dentists.27 For dental specialists, the American Academy of Pediatric Dentistry,28,29 the American Association of Endodontists,30,31 and the American Academy of Periodontology32 also have useful guidelines. Furthermore, the ADA is in the process of developing guidelines for dental infections, which should complement the long-standing ADA antibiotic prophylaxis guidelines nicely.33 The authors have provided a list of 3 useful resources from the CDC and ADA on how to optimize antibiotic prescribing (Box).
Box: List of resources.
American Dental Association Antibiotic Stewardship https://www.ada.org/en/member-center/oral-health-topics/antibiotic-stewardship
Centers for Disease Control and Prevention Antibiotic Stewardship in Oral Health21–22 https://www.cdc.gov/oralhealth/infectioncontrol/faqs/antibiotic-stewardship.html
American Dental Association Combating Antibiotic Resistance https://jada.ada.org/article/S0002-8177(14) 61234–4/pdf
Further research will be necessary to evaluate the effect of the future ADA guidelines for dental infections after its release. Dentists and dental specialists have been quick to embrace the ADA antibiotic prophylaxis guidelines.34,35 However, significant opportunities to improve antibiotic prescribing for some conditions remain. For example, in a survey of 450 community dentists in Canada, investigators found that 42% of respondents still recommend antibiotic prophylaxis for mitral valve prolapse.36 Generally, targeted interventions, such as clinical decision support tools and communication skills training, have been more successful at improving antibiotic prescribing among medical care providers.37
Interventional strategies customized to dentistry likely will be used to improve antibiotic prescribing among dentists and dental specialists. Outside the United States, clinical audit and feedback interventions have been successful in reducing antibiotic use by general dentists and oral maxillofacial surgeons. In 1 study in the United Kingdom, the investigators pooled data from a previous audit and feedback investigation and reported a 43.6% reduction in antibiotic Rxs and an increase in Rxs that were error free for prescribed duration, frequency, and dosaged—from 48% through 78% after the intervention.38 The intervention was also well accepted by oral health care practitioners: more than 97% of the dentists involved in 1 clinical audit reported it useful.39 In another study in which the investigators used prospective audit and feedback of antibiotics prescribed in an oral surgery department in the United Kingdom, antibiotic appropriateness increased from 30% before the intervention to 80% afterward.23
The seasonal prescribing pattern of pediatric dentists and orthodontists is a novel finding in the dental literature. However, investigators in other studies have described seasonal variation in antibiotic Rxs.5,6,40,41 This variation is widely thought to be driven by inappropriate antibiotic prescribing for viral upper respiratory tract infections.5,6,41 We speculate that the seasonal variation observed in our study also is related to antibiotic management of viral infections. Viral sinusitis, in particular, may manifest with referred tooth pain. Such infections are common among children, which may help explain why we observed these trends specifically for pediatric dentists and orthodontists.42 School summer vacations also may help explain the summer troughs in antibiotic prescribing by pediatric dentists and orthodontists.
Investigators should complete further studies to elucidate more fully the antibiotic prescribing trends among dental specialists and investigate optimal interventions to optimize prescribing rates. Studies in which the investigators assess the appropriateness of and motivation for antibiotic Rxs by dental specialists will be helpful in determining more specific targets for intervention. In addition, further research is necessary to understand seasonal variation in antibiotic prescribing among orthodontists and pediatric dentists.
Our study has limitations. First, it was difficult to analyze the secular trends in certain specialties because of a low number of antibiotic Rxs. Second, because the ESHC database only contains Rxs purchased via insurance benefits, our data may underrepresent antibiotic Rxs that patients might pay for out of pocket. Third, we were unable to evaluate the indication or appropriateness for each antibiotic Rx. Fourth, our database did not contain any information about dentists from disciplines, such as oral medicine, that are not recognized by the ADA.
CONCLUSIONS
During the 3-year study period, we did not identify any significant changes in antibiotic prescribing practices among dental specialists. Our data suggest there may be antibiotic stewardship opportunities to improve antibiotic prescribing practices. Furthermore, we observed some seasonal variation in antibiotic prescribing among pediatric dentists and orthodontists. These trends may be related to inappropriate treatment of viral respiratory conditions.
Supplementary Material
Disclosures.
Drs. Munshi and Henderson are employees of Express Scripts Holding Company (ESHC) and have received ESHC stock and stock options as part of employee compensation. Dr. Fraser has grant funding from the Centers for Disease Control and Prevention, Doris Duke Charitable Foundation, Foundation for Barnes-Jewish Hospital, and National Institutes of Health, and her spouse is senior vice president and chief medical officer at ESHC. None of the other authors reported any disclosures.
This study was funded by grant U54CK000482 (M.J.D., Q.F., K.W., V.J.F.) from the Centers for Disease Control and Prevention. Research reported in this publication was supported by award KL2TR002346 from the National Center for Advancing Translational Sciences, National Institutes of Health.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Centers for Disease Control and Prevention, the Department of Veterans Affairs, the National Institutes of Health, or the U.S. government.
The authors thank S. Reza Jafarzadeh, DVM, MPVM, PhD, from Boston University School of Medicine for his assistance with peak-to-trough analyses and interpretation.
ABBREVIATION KEY
- AAR
Annual antibiotic prescription rates
- ADA
American Dental Association
- CDC
Centers for Disease Control and Prevention
- ESHC
Express Scripts Holding Company
- PTTR
Peak-to-trough ratio
- Rx
Prescription
Footnotes
This article has an accompanying online continuing education activity available at: http://jada.ada.org/ce/home.
SUPPLEMENTAL DATA
Supplemental data related to this article can be found at: https://doi.org/10.1016/j.adaj.2019.05.028.
Contributor Information
Michael J. Durkin, Division of Infectious Diseases, Washington University School of Medicine in St. Louis, Campus Box 8051, 4523 Clayton Ave., St. Louis, MO 63110-1093.
Qianxi Feng, Data analyst, Division of Infectious Diseases, Washington University School of Medicine in St. Louis, and a graduate student, Brown School of Social Work and Public Health, Washington University in St. Louis, St. Louis, MO..
Katie J. Suda, Research health scientist, Center of Innovation for Complex Chronic Healthcare, Edward Hines Jr. Veterans Affairs Hospital, and an associate professor, Department of Pharmacy Systems, Outcomes, and Policy, University of Illinois at Chicago, Chicago, IL..
Peter B. Lockhart, Department of Oral Medicine, Carolinas Medical Center, Charlotte, NC..
Martin H. Thornhill, Professor, Department of Oral Medicine, Carolinas Medical Center, Charlotte, NC, and a professor, Unit of Oral and Maxillofacial Medicine, Pathology and Surgery, School of Clinical Dentistry, University of Sheffield, Sheffield, United Kingdom..
Kyle Warren, Data analyst, Division of Infectious Diseases, Washington University School of Medicine in St. Louis, St. Louis, MO, and a graduate student, University of Missouri School of Medicine, Columbia, MO..
Victoria J. Fraser, Washington University School of Medicine in St. Louis, St. Louis, MO..
References
- 1.Srinivasan A Antibiotic stewardship: why we must, how we can. Cleve Clin J Med. 2017;84(9):673–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Core elements of antibiotic stewardship. Available at: https://www.cdc.gov/antibiotic-use/core-elements/index.html. Accessed August 21, 2019.
- 3.Centers for Disease Control and Prevention. Antibiotic prescribing and use in doctor’s offices. Available at: https://www.cdc.gov/antibiotic-use/community/index.html. Accessed June 6, 2018.
- 4.Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010–2011. JAMA. 2016; 315(17):1864–1873. [DOI] [PubMed] [Google Scholar]
- 5.Suda KJ, Hicks LA, Roberts RM, Hunkler RJ, Taylor TH. Trends and seasonal variation in outpatient antibiotic prescription rates in the United States, 2006 to 2010. Antimicrob Agents Chemother (Bethesda). 2014;58(5): 2763–2766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Durkin MJ, Jafarzadeh SR, Hsueh K, et al. Outpatient antibiotic prescription trends in the United States: a national cohort study. Infect Control Hosp Epidemiol. 2018; 39(5):584–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roberts RM, Bartoces M, Thompson SE, Hicks LA. Antibiotic prescribing by general dentists in the United States, 2013. JADA. 2017;148(3):172–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Durkin MJ, Hsueh K, Sallah YH, et al. An evaluation of dental antibiotic prescribing practices in the United States. JADA. 2017;148(12):878.e1–886.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durkin MJ, Feng Q, Warren K, et al. ; Centers for Disease Control and Prevention Epicenters. Assessment of inappropriate antibiotic prescribing among a large cohort of general dentists in the United States. JADA. 2018; 149(5):372.e1–381.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marra F, George D, Chong M, Sutherland S, Patrick DM. Antibiotic prescribing by dentists has increased: why? JADA. 2016;147(5):320–327. [DOI] [PubMed] [Google Scholar]
- 11.Ford P, Saladine C, Zhang K, Hollingworth S. Pre-scribing patterns of dental practitioners in Australia from 2001 to 2012: antimicrobials. Aust Dent J. 2017;62(1):52–57. [DOI] [PubMed] [Google Scholar]
- 12.Pipalova R, Vlcek J, Slezak R. The trends in antibiotic use by general dental practitioners in the Czech Republic (2006–2012). Int Dent J. 2014;64(3):138–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Christensen AL, Lundbye-Christensen S, Dethlefsen C. Poisson regression models outperform the geometrical model in estimating peak-to-trough ratio of seasonal variation: a simulation study. Comput Methods Programs Biomed. 2011;104: 333–340. [DOI] [PubMed] [Google Scholar]
- 14.Stein K, Farmer J, Singhal S, Marra F, Sutherland S, Quiñonez C. The use and misuse of antibiotics in dentistry: a scoping review. JADA. 2018;149(10):869.e5–884.e5. [DOI] [PubMed] [Google Scholar]
- 15.De-Bem SHC, Nhata J, Santello LC, Bighetti RL, da Cruz Filho AM. Antibiotic prescription behavior of specialists in endodontics. Dent Press Endod. 2011;1(3): 88–93. [Google Scholar]
- 16.Deeb GR, Soung GY, Best AM, Laskin DM. Anti- biotic prescribing habits of oral and maxillofacial surgeons in conjunction with routine dental implant placement. J Oral Maxillofac Surg. 2015;73(10):1926–1931. [DOI] [PubMed] [Google Scholar]
- 17.Yesudian GT, Gilchrist F, Bebb K, et al. A multicentre, multicycle audit of the prescribing practices of three paediatric dental departments in the North of England. Br Dent J. 2015;218(12):681–685. [DOI] [PubMed] [Google Scholar]
- 18.Yingling N, Ellenbyrne B, Hartwell G. Antibiotic use by members of the American Association of Endodontics in the year 2000: report of a national survey. J Endod. 2002;28(6):396–404. [DOI] [PubMed] [Google Scholar]
- 19.Sivaraman S, Hassan M, Pearson JM. A national survey of pediatric dentists on antibiotic use in children. Pediatr Dent. 2015;35(7):546–549. [PubMed] [Google Scholar]
- 20.Segura-Egea JJ, Velasco-Ortega E, Torres-Lagares D, Velasco-Ponferrada MC, Monsalve-Guil L, Llamas-Carreras JM. Pattern of antibiotic prescription in the management of endodontic infections amongst Spanish oral surgeons. Int Endod J. 2010;43(4):342–350. [DOI] [PubMed] [Google Scholar]
- 21.Sancho-Puchades M, Herraez-Vilas JM, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C. Analysis of the antibiotic prophylaxis prescribed by Spanish oral surgeons. Med Oral Patol Oral Cir Bucal. 2009;14(10):533–537. [DOI] [PubMed] [Google Scholar]
- 22.Froum SJ, Weinberg MA. An evaluation of antibiotic use in periodontal and implant practices. Int J Periodontics Restorative Dent. 2015;35(4):481–487. [DOI] [PubMed] [Google Scholar]
- 23.Chopra R, Merali R, Paolinelis G, Kwok J. An audit of antimicrobial prescribing in an acute dental care department. Prim Dent J. 2014;3(4):24–29. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Core elements of outpatient antibiotic stewardship. Available at: https://www.cdc.gov/antibiotic-use/community/improving-prescribing/core-elements/core-outpatient-stewardship.html. Accessed May 19, 2019.
- 25.American Board of Internal Medicine Foundation. Choosing Wisely. Available at: http://www.choosingwisely.org/clinician-lists/#keyword=antibiotic. Accessed July 12, 2017.
- 26.Centers for Disease Control and Prevention. Check-list for antibiotic prescribing in dentistry. Available at: https://www.cdc.gov/antibiotic-use/community/downloads/dental-fact-sheet-FINAL.pdf. Accessed August 30, 2018.
- 27.Centers for Disease Control and Prevention. Addressing antibiotic resistance in dentistry: “What can WE do?” Available at: https://blogs.cdc.gov/safehealthcare/addressing-antibiotic-resistance-in-dentistry-what-can-we-do/. Accessed August 30, 2018.
- 28.Guideline on use of antibiotic therapy for pediatric dental patients. Pediatr Dent. 2016;38(6):325–327. [PubMed] [Google Scholar]
- 29.Guideline on antibiotic prophylaxis for dental patients at risk for infection. Pediatr Dent. 2016;38(6):328–333. [PubMed] [Google Scholar]
- 30.American Association of Endodontists. AAE guidance on antibiotic prophylaxis for patients at risk of systemic disease. Available at: http://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/aae_antibiotic-prophylaxis.pdf. Accessed June 7, 2018.
- 31.American Association of Endodontists. AAE guidance on the use of systemic antibiotics in endodontics. Available at: http://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/aae_systemic-antibiotics.pdf. Accessed June 7, 2018.
- 32.Slots J Systemic antibiotics in periodontics. J Periodontol. 2004;75(11):1553–1565. [DOI] [PubMed] [Google Scholar]
- 33.Wilson W, Taubert KA, Gewitz M, et al. ; American Heart Association. Prevention of infective endocarditis: guidelines from the American Heart Associationda guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. JADA. 2008;139(suppl):3S–24S. [DOI] [PubMed] [Google Scholar]
- 34.Lockhart PB, Hanson NB, Ristic H, Menezes AR, Baddour L. Acceptance among and impact on dental practitioners and patients of American Heart Association recommendations for antibiotic prophylaxis. JADA. 2013; 144(9):1030–1035. [DOI] [PubMed] [Google Scholar]
- 35.Cherry WR, Lee JY, Shugars DA, White RR, Vann WF. Antibiotic use for treating dental infections in children: a survey of dentists’ prescribing practices. JADA. 2012;143:31–38. [DOI] [PubMed] [Google Scholar]
- 36.Jain P, Stevenson T, Sheppard A, et al. Antibiotic prophylaxis for infective endocarditis: knowledge and implementation of American Heart Association Guidelines among dentists and dental hygienists in Alberta, Canada. JADA. 2015;146(10):743–750. [DOI] [PubMed] [Google Scholar]
- 37.Drekonja DM, Filice GA, Greer N, et al. Antimicrobial stewardship in outpatient settings: a systematic review. Infect Control Hosp Epidemiol. 2015;36(2):142–152. [DOI] [PubMed] [Google Scholar]
- 38.Palmer N, Dailey Y, Martin M. Pharmacology: can audit improve antibiotic prescribing in general dental practice? Br Dent J. 2001;191(5):253–255. [DOI] [PubMed] [Google Scholar]
- 39.Palmer N, Dailey Y. General dental practitioners’ experiences of a collaborative clinical audit on antibiotic pre-scribing: a qualitative study. Br Dent J. 2002;193(1):46–49. [DOI] [PubMed] [Google Scholar]
- 40.Sun L, Klein EY, Laxminarayan R. Seasonality and temporal correlation between community antibiotic use and resistance in the United States. Clin Infect Dis. 2012; 55(5):687–694. [DOI] [PubMed] [Google Scholar]
- 41.Hobbs MR, Grant CC, Ritchie SR, et al. Antibiotic consumption by New Zealand children: exposure is near universal by the age of 5 years. J Antimicrob Chemother. 2017;72(6):1832–1840. [DOI] [PubMed] [Google Scholar]
- 42.Miller EK, Williams JV. The common cold. In: Nelson Textbook of Pediatrics. 20th ed. Philadelphia, PA: Elsevier; 2016:2011–2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


