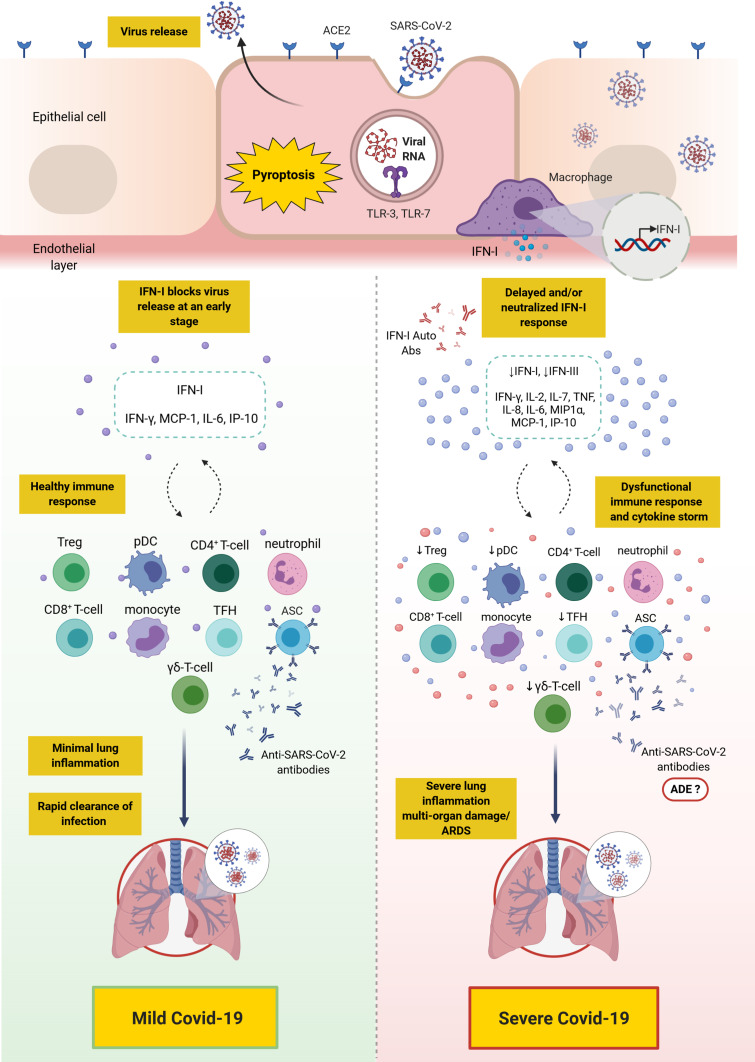
Figure 2.
Overall depiction of the immune response in mild versus severe Covid-19. SARS-CoV-2 binds to ACE2 expressing cells. Upon entry, viral RNA is recognized by TLR-7 which results in the production of proinflammatory cytokines (such as IL-6 and TNF) and IFN-I. Alveolar macrophages trigger the release of proinflammatory cytokines and chemokines attracting T-cells, pDC and monocytes to the site of infection. In mild Covid-19, the release of IFN-I blocks viral replication and its release at an early stage, thus, controlling the infection. However, in severe Covid-19, due to a defective immune response, a delay in IFN-I production and/or its neutralization with anti-IFN-I autoantibodies may lead to continued viral replication and a profound inflammatory response, namely “cytokine storm”. This is also accompanied with the accumulation of neutrophils, monocytes and T-cells in the lungs leading to lung damage. Ineffective anti-SARS-CoV-2 antibodies produced by ASCs may play a role in the pathogenesis of SARS-CoV-2 and its clinical sequalae through ADE.
Note: This figure was created with BioRender.com.
Abbreviations: ACE2, angiotensin-converting enzyme 2; ADE, antibody-dependent enhancement; ARDS, acute respiratory distress syndrome; Auto-Abs, autoantibodies; ASC, antibody secreting cell; Covid-19, coronavirus disease 2019; IFN, interferon; IP-10, interferon γ-induced protein-10; IL, interleukin; MCP-1, monocyte chemoattractant protein-1; MIP1α, macrophage inflammatory protein 1α; pDC, plasmacytoid dendritic cell; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TLR, toll-like receptor; TNF, tumor necrosis factor; Treg, regulatory T-cells; TFH, T follicular helper.