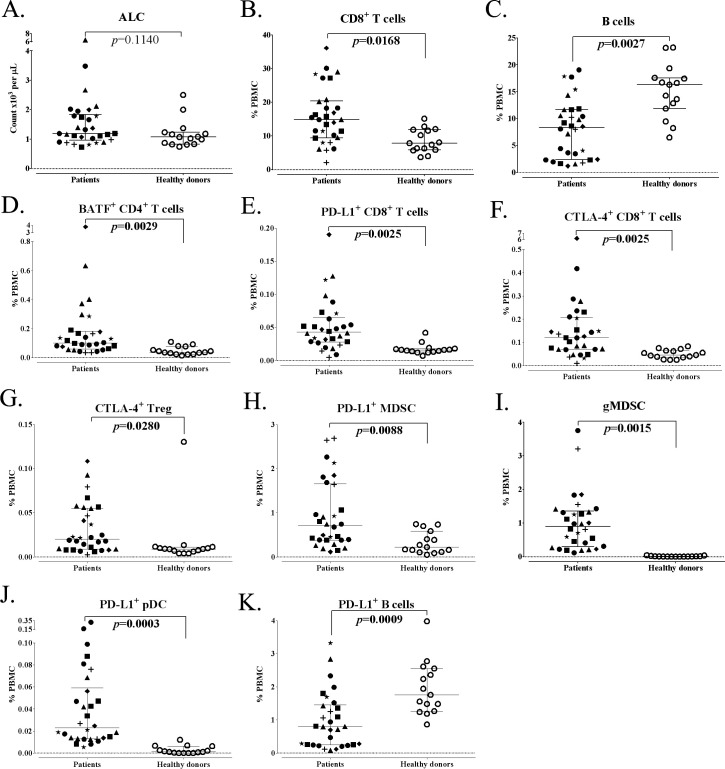
Figure 3.
Differences in standard parental immune cell types and refined subsets in age-matched advanced cancer patients and healthy donors. Patients with advanced cancer (n=30) and healthy donors (n=15) included in this analysis were age-matched above age 40. (A) ALC of cancer patients and healthy donors. (B, C) Standard parental immune cell types that were different between cancer patients and healthy donors. (D–K) Representative graphs are shown for notable refined subsets with differences between cancer patients and healthy donors. Graphs display median ALC or median frequency as a percentage of PBMCs with 25–75 percentiles. Cancer type is indicated by shape (square: GI (anal, colon, esophageal); n=6; triangle: pancreatic, n=6; star: breast, n=3; plus sign: mesothelioma, n=3; diamond: renal cell, n=3; closed circle: other (adrenocortical, chordoma, lung, medullary thyroid, neuroendocrine, ovarian, prostate, and spindle cell), n=9; open circle: healthy donors, n=15). Differences were defined by an adjusted p<0.05, the median of groups showing a >50% difference, and a frequency above 0.01% for PBMCs. P value was calculated using the Mann-Whitney test and with Holm adjustment made for multiple comparisons using the number of standard immune cell types with a frequency above 0.01% of PBMCs (n=9). For refined subsets, Holm adjustment was made using the number of subsets within each standard subset with a frequency above 0.01% for PBMCs (n=29 for CD4+ T cells, 25 for CD8+ T cells, 5 for Tregs, 14 for NK cells, 3 for NKT cells, 4 for B cells, 2 for cDCs, 3 for pDCs and 15 for MDSCs). Figure adapted from Lepone.18 ALC, absolute lymphocyte count; BATF, basic leucine zipper ATF-like transcription factor; cDC, conventional dendritic cells; CTLA-4, cytotoxic T lymphocyte-associated protein-4; GI, gastrointestinal; gMDSCs, granulocytic myeloid-derived suppressor cells; NK, natural killer; PBMCs, peripheral blood mononuclear cells; pDC, plasmacytoid DC; PD-L1, programmed cell death ligand-1; Tregs, regulatory T cells.