Fig. 3.
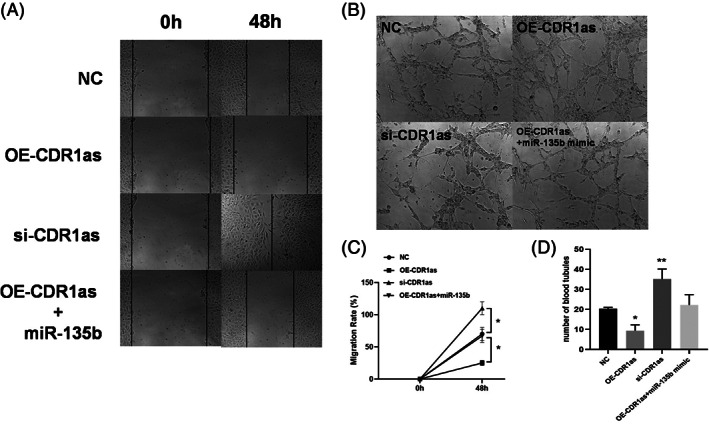
Effects of CircCDR1as on the migration and angiogenesis of BMECs. (A) Representative images of wound scratch‐wound assays after transfecting bone microvascular endothelial cells (BMECs) with CDR1as, si‐CDR1as, OE‐CDR1as + miR‐135b, and NC. Images were taken at 0 and 48 h after the cell layer was scratched with a pipette tip. Scale bar: 50 μm. (B) Representative images of tube formation assays at 48 h after seeding BMECs transfected with OE‐CDR1as, si‐CDR1as, OE‐CDR1as + miR‐135b, and NC on Matrigel. Scale bar: 100 μm. (C) Statistical analysis of the wound‐healing rates revealed that transfection with OE‐CDR1as statistically significantly inhibited BMEC migration compared with that of the NC group whereas transfecting siCDR1as had the opposed effect. (D) Statistical analysis of the relative change in tube length revealed that transection with OE‐CDR1as had statistically significantly inhibited tube formation in BMECs compared with that of the NC group, whereas transfecting si‐CDR1as had the opposed effect. n = 3 per group. *P < 0.05,**P < 0.01.
