Abstract
Objectives. To project the range of excess deaths potentially associated with COVID-19–related unemployment in the United States and quantify inequities in these estimates by age, race/ethnicity, gender, and education.
Methods. We used previously published meta-analyzed hazard ratios (HRs) for the unemployment–mortality association, unemployment data from the Bureau of Labor Statistics, and mortality data from the National Center for Health Statistics to estimate 1-year age-standardized deaths attributable to COVID-19–related unemployment for US workers aged 25 to 64 years. To accommodate uncertainty, we tested ranges of unemployment and HR scenarios.
Results. Our best estimate is that there will be 30 231 excess deaths attributable to COVID-19–related unemployment between April 2020 and March 2021. Across scenarios, attributable deaths ranged from 8315 to 201 968. Attributable deaths were disproportionately high among Blacks, men, and those with low education.
Conclusions. Deaths attributable to COVID-19–related unemployment will add to those directly associated with the virus and will disproportionately burden groups already experiencing incommensurate COVID-19 mortality.
Public Health Implications. Supportive economic policies and interventions addressing long-standing harmful social structures are essential to mitigate the unequal health harms of COVID-19.
In April 2020, the US unemployment rate peaked at 14.7%, its highest level since the Great Depression. A robust literature has shown that unemployment increases mortality.1 Unemployment may increase risk of mortality through multiple mechanisms, including elevated risk of suicide, substance abuse, health care deferment, and cardiovascular disease.2 This has resulted in recent calls to examine excess mortality resulting from unemployment driven by the COVID-19 pandemic.3 We used existing data to estimate the short-term mortality consequences of the epidemic of corollary illnesses3 likely to result from the COVID-19 recession.
Our primary objectives were to (1) project the plausible range of excess deaths associated with the March and April 2020 incident unemployment attributable to COVID-19 (hereafter referred to as “COVID-19–related unemployment”), and (2) examine inequities in these estimates by age, race/ethnicity, gender, and educational attainment. This work has important implications for considering the full range of health consequences and health inequities linked to COVID-19.
METHODS
We estimated the 1-year death count attributable to the spring 2020 spike in COVID-19–related unemployment for the US population in the labor force aged 25 to 64 years. We derived hazard ratios (HRs) for all-cause mortality associated with unemployment from a highly cited meta-analysis.1 We used only the HRs from studies that controlled for baseline health behaviors that may otherwise confound estimates.1 We drew seasonally adjusted unemployment prevalence from Bureau of Labor Statistics monthly reports. We defined pre–COVID-19 unemployment as February 2020—immediately before the economic impacts of COVID-19 manifested in US unemployment estimates—and peak of COVID-19–related unemployment as April 2020. We calculated COVID-19–related unemployment as the difference between peak of and pre–COVID-19 unemployment. We derived all-cause mortality counts and rates from the National Center for Health Statistics.
We converted HRs to relative risks (RRs) and calculated the fraction of deaths attributable to COVID-19–related unemployment (the population attributable fraction, or PAF) using the COVID-19–related unemployment prevalence and unemployment–mortality RRs (formulas are in the Appendix [available as a supplement to the online version of this article at http://www.ajph.org]). We multiplied the PAF by total annual prepandemic deaths to calculate the annualized excess deaths expected from COVID-19–related unemployment.
We calculated attributable deaths overall and stratified them by race/ethnicity, gender, and educational attainment. We age-adjusted estimates by using age-specific HRs, unemployment prevalence, and mortality counts and rates for age groups 25 to 34, 35 to 44, 45 to 54, and 55 to 64 years. We calculated total excess deaths as the sum of age-specific–attributable deaths. Inputs aligned imperfectly for exact population groups and periods. For example, unemployment estimates were available only for those aged 55 years and older rather than those aged 55 to 64 years. We used the most recent and rigorous estimates available and aligned them as well as possible (Table A [available as a supplement to the online version of this article at http://www.ajph.org]). Fully adjusted HRs were available by age group and gender but not by age group and education or race/ethnicity; we assumed the overall age group–specific HRs applied to each age group within each subgroup. Unemployment estimates were unavailable by age–education group and by age–race/ethnicity group for the study periods; we assumed that the relative contributions of each group to overall unemployment for the most recent stratified data (2019 for age–education and quarter 1 of 2020 for age–race/ethnicity) held for 2020, and we applied a correction factor.
Finally, because COVID-19–related unemployment levels are uncertain and the mortality effects of COVID-19–related unemployment may vary in magnitude (but are likely consequential under any set of circumstances), we generated estimates for ranges of scenarios. Unemployment ranged from 10% (maximum observed during the Great Recession)4 to 26.5% (upper bound using alternative definitions of labor force participation).5 HRs ranged from −2-fold to +3-fold from observed. To project alternative unemployment levels for subgroups, we assumed that the relative disparities in unemployment surges across subgroups from February to April 2020 were constant.
RESULTS
We estimated 30 231 excess deaths attributable to COVID-19–related unemployment among the US population aged 25 to 64 years between April 2020 and March 2021 (Table B [available as a supplement to the online version of this article at http://www.ajph.org]). Attributable deaths varied by age, gender, education, and race/ethnicity, with the burden disproportionately experienced by men, Blacks, those aged 45 years or older, and those with a high school education or less (Figure 1). For example, Blacks made up 12% of the population but 19% of unemployment-related deaths. Similarly, individuals with a high school education or less represented 37% of the population but 72% of unemployment-related deaths.
FIGURE 1—
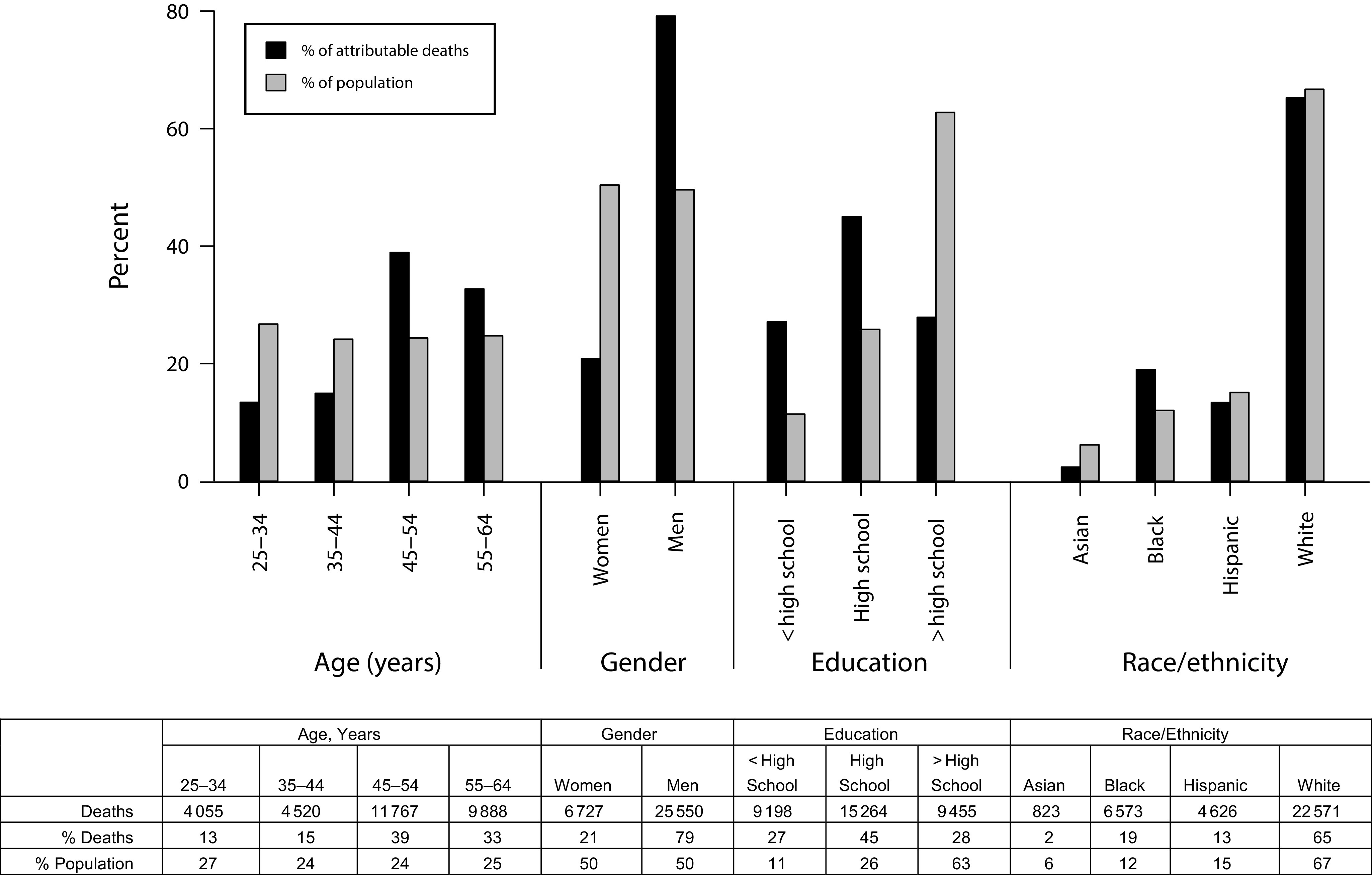
Estimated 1-Year Age-Standardized Death Count Attributable to COVID-19–Related Unemployment for the US Population Aged 25–64 Years, by Race/Ethnicity, Gender, and Educational Attainment: April 2020–March 2021
Note, high school = high school diploma or equivalent; Hispanic = Hispanic or Latinx. Values indicate the attributable death count, percentage of attributable deaths, and percentage of population in each group. All race/ethnicity groups are non-Hispanic/Latinx unless otherwise specified.
Attributable deaths varied across unemployment levels and harmfulness of unemployment (Table C [available as a supplement to the online version of this article at http://www.ajph.org]). In the best-case scenario, if April 2020 unemployment was 10% and half as harmful as previously observed, we estimated 8315 attributable deaths. In the worst-case scenario, if April 2020 unemployment was 26.5%5 and thrice as harmful as previously observed, we estimated 201 968 attributable deaths.
DISCUSSION
Substantial uncertainty remains about the health consequences of the COVID-19 pandemic. We used available evidence to approximate 1-year excess all-cause deaths attributable to unemployment in the US working-age population following the April 2020 COVID-19–related unemployment spike. Our best estimate is 30 231 excess deaths. This estimate is in line with previously published estimates for excess suicide, alcohol, and drug misuse associated with unemployment.6,7 To put these estimates in context, as of January 18, 2021, there have been 398 838 deaths attributable to the virus itself.8
There are 2 key takeaways: first, deaths attributable to COVID-19–related unemployment will add to those directly associated with the virus. Second, COVID-19 unemployment-attributable deaths will disproportionately burden Black Americans, those aged 45 years or older, men, and those with low education. These disparities are stark and contribute to an unjust double burden9 whereby the combination of high unemployment and excess COVID-19 deaths will further contribute to unacceptable and preventable deaths, particularly among low-educated and Black Americans.
Limitations
We note several limitations. First, we applied meta-analyzed HRs with a median follow-up of 8 years to annualized death counts; we may have overestimated 1-year deaths if some causes required longer durations to manifest (e.g., alcoholic liver cirrhosis). However, the risk of unemployment-related mortality is highest in the short term.1 Overestimation may also occur because excess deaths from COVID-19 may preempt some COVID-19–related unemployment deaths. Second, we used standard definitions of unemployment and labor force participation, which may not capture labor force dynamics during a pandemic. Mortality may also result from withdrawal from the labor force. Third, our HRs reflect both incident and cross-sectionally assessed unemployment irrespective of unemployment duration; incident COVID-19–related unemployment may be shorter in duration. Relatedly, the factors that moderate the mortality effects of unemployment are uncertain10; heterogeneity in HRs by unmeasured factors is possible. Further, because race- and education-specific HRs were unavailable, the true inequities between groups may be wider than we report.
Our estimates reflect short-term attributable mortality among a hardest-hit group—those who lost their jobs. It is worth noting that recession effects can last far longer than the recession itself.11 Our data suggest that we can expect excess mortality linked to unemployment that will compound the impact of the pandemic on morbidity and mortality, particularly among vulnerable groups. These effects will also plausibly extend well beyond the 1-year time window that was the focus of our analysis.
Public Health Implications
Existing data can be used to forecast COVID-19–related health impacts and inform decision making. Adequate responses to pandemics would require adopting specific policies to protect workers and mitigate the harms of unemployment,12 while intervening in long-standing, unjust social structures. Proactive public policies are needed to prevent further inequitable health and social consequences of the COVID-19 pandemic.
ACKNOWLEDGMENTS
This study was supported by the National Institute on Aging, National Institutes of Health (grant T32 AG049663).
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
This study was based entirely on publicly available secondary data and was therefore exempt from institutional review board review.
REFERENCES
- 1.Roelfs DJ, Shor E, Davidson KW, Schwartz JE. Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med. 2011;72(6):840–854. doi: 10.1016/j.socscimed.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jin RL, Shah CP, Svoboda TJ. The impact of unemployment on health: a review of the evidence. CMAJ. 1995;53(5):529–540. [Erratum in: Jin RL. Effect of unemployment on health: acknowledgement. CMAJ. 1995;153(11):1567–1568] [PMC free article] [PubMed] [Google Scholar]
- 3.Harvey Brenner M. Will there be an epidemic of corollary illnesses linked to a COVID-19–related recession? Am J Public Health. 2020;110(7):974–975. doi: 10.2105/AJPH.2020.305724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cunningham E. Great recession, great recovery? Trends from the current population survey. Monthly Labor Review. April 2018. Available at: https://www.bls.gov/opub/mlr/2018/article/great-recession-great-recovery.htm. Accessed July 7, 2020.
- 5.Fairlie RW, Couch K, Xu H. The Impacts of COVID-19 on Minority Unemployment: First Evidence From April 2020 CPS Microdata. Cambridge, MA: National Bureau of Economic Research; 2020. NBER working paper 27246. Available at: https://www.nber.org/system/files/working_papers/w27246/w27246.pdf. Accessed January 17, 2021. [Google Scholar]
- 6.Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petterson S, Westfall JM, Miller BF. Projected deaths of despair from COVID-19. Available at: https://digitalcommons.psjhealth.org/cgi/viewcontent.cgi?article=3991&context=publications. Accessed January 17, 2021.
- 8.Coronavirus in the U.S. latest map and case count. New York Times. 2021. Available at: https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html. Accessed January 18, 2021.
- 9.Kirby JB, Kaneda T. “Double jeopardy” measure suggests Blacks and Hispanics face more severe disparities than previously indicated. Health Aff (Millwood) 2013;32(10):1766–1772. doi: 10.1377/hlthaff.2013.0434. [DOI] [PubMed] [Google Scholar]
- 10.Roelfs DJ, Shor E, Blank A, Schwartz JE. Misery loves company? A meta-regression examining aggregate unemployment rates and the unemployment-mortality association. Ann Epidemiol. 2015;25(5):312–322. doi: 10.1016/j.annepidem.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brenner MH. The impact of unemployment on heart disease and stroke mortality in European Union countries. 2016. Available at: http://ec.europa.eu/social/BlobServlet?docId=15932&langId=en. Accessed January 17, 2021.
- 12.Benfer EA, Wiley LF. Health justice strategies to combat COVID-19: protecting vulnerable communities during a pandemic. 2020. Available at: https://www.healthaffairs.org/do/10.1377/hblog20200319.757883/full. Accessed January 17, 2021.


