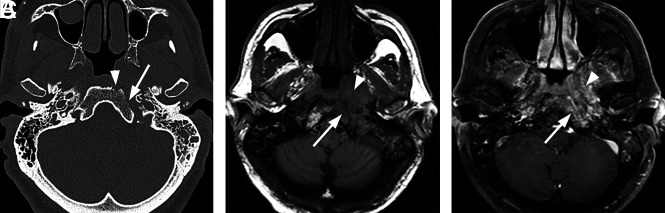
FIG 1.
Typical skull base osteomyelitis. A 55-year-old man with type 2 diabetes with low-grade fever, severe pain, and drainage from his left ear. Eight weeks before imaging, the patient had been diagnosed with left-sided otitis media and possible otitis externa. He had initially been treated with amoxicillin and ofloxacin drops, without improvement. Culture from left-ear drainage revealed methicillin-sensitive S aureus. The patient was treated with IV vancomycin and piperacillin/tazobactam for 2 weeks and then 14 weeks of amoxicillin/clavulanate. All clinical and laboratory parameters initially resolved during 4 months. However, a gallium scan continued to indicate abnormal activity of the skull base at both 8 and 16 weeks. Despite the gallium scan, antibiotics were discontinued. Within 2 weeks, the patient had recurrent symptoms and severe neck pain. Additional imaging (not shown) indicated new cervicocranial septic arthritis, requiring an additional 3 months of IV antibiotics that led to a cure. A, Axial CT demonstrates opacification of left-mastoid air cells. There is subtle erosion along the petro-occipital fissure (arrow) and loss of cortical bone along the left lateral margin of the clivus (arrowhead). B, Axial unenhanced T1-weighted MR image demonstrates abnormal signal in the marrow space of the basiocciput (arrow), ill-defined signal in the left carotid space, and masslike submucosal infiltration of the left nasopharynx (arrowhead). C, Axial T1-weighted fat-saturated contrast-enhanced image demonstrates abnormal enhancement involving the marrow space of the clivus (arrow) as well as heterogeneous enhancement of infiltrating soft tissue in the left nasopharynx (arrowhead).