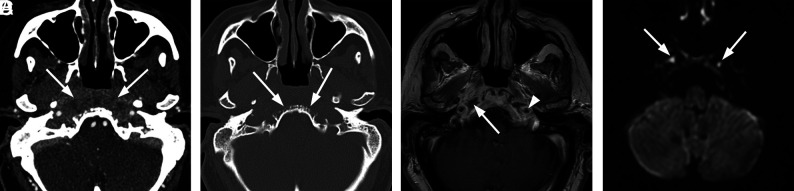
FIG 2.
Atypical skull base osteomyelitis. A 72-year-old man with history of hypertension presented with a 9-week history of sinus congestion, rhinorrhea, and headache. The patient had been treated for severe sinusitis with several courses of oral antibiotics and steroid injections prescribed by his primary care physician as well as community ear, nose, and throat physicians. Just before admission, he developed left hearing loss and left-sided facial palsy. Swab culture of the nasopharynx revealed P aeruginosa. The patient was treated with amoxicillin-pot clavulanate (Augmentin) and Ceftazidime (Ceftaz) with clinical resolution after several weeks. Follow-up MR imaging at 4 months confirmed improvement. A, Axial contrast-enhanced CT scan demonstrates patchy heterogeneous density in the preclival soft tissues extending to involve the carotid spaces bilaterally (arrows). The inflammatory tissues in the preclival soft tissues could mimic an infiltrative neoplasm of the nasopharynx. B, Axial bone CT at the same level shows irregular erosions of the ventral clivus (arrows). C, Axial T1-weighted contrast-enhanced MRI. There is nodular enhancement involving the clivus at this level with focal areas of necrosis and abscess just inferior to the foramina lacerum (arrow). Note circumferential enhancement of the petrous internal carotid arteries (arrowhead). D, Axial DWI depicts small foci of fluid near the foramen lacerum bilaterally as diffusion-restricted, consistent with focal abscesses (arrows).