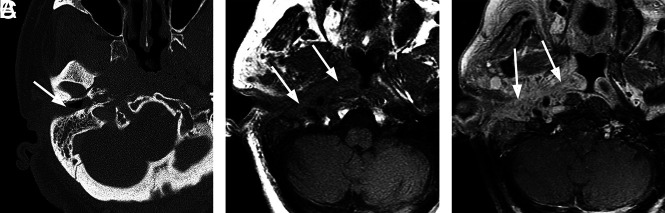
FIG 5.
Typical SBO from NEO. An 82-year-old woman with insulin-dependent diabetes presented with a several-month history of pain and drainage from the right ear. The patient was recently treated as an outpatient with several rounds of antibiotics (including amoxicillin/clavulanate and ciprofloxacin) for otitis media and NEO, but symptoms had progressed. Following imaging and a diagnosis of SBO, the patient was treated with 4 weeks of IV vancomycin and piperacillin/tazobactam and additional 4 weeks of oral ciprofloxacin. The patient initially had clinical improvement, but a gallium scan at 8 weeks showed persistent uptake. The patient did not return for follow-up as instructed but returned 8 months after the original admission with progressive infection extending to the central skull base and left temporal bone, requiring an additional 6 weeks of IV antibiotic treatment. A, Axial CT scan through the right EAC demonstrates thickening and partial opacification of the external auditory canal (arrow). There is subtle erosion along the posterior wall of the external auditory canal and mild soft-tissue fullness of the right nasopharynx. B, Axial T1-weighted MR image demonstrates obliteration of normal fat planes in the submucosal and preclival tissues of the nasopharynx (arrows). This process extends posterolaterally to the tip of the mastoid on the right. C, Axial T1-weighted contrast-enhanced image demonstrates heterogeneous enhancement of abnormal tissue extending from the tip of the mastoid on the right to the nasopharynx (arrows) without discrete abscess formation.