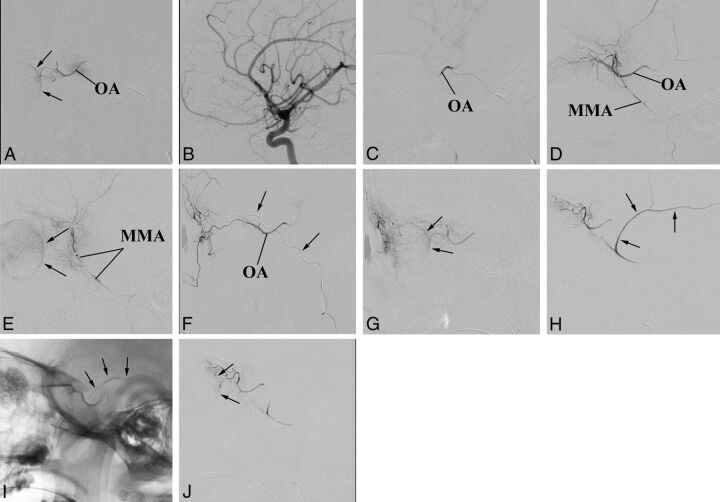
Fig 1.
An exemplary case of adaptable approaches to the IAC. The patient has bilateral retinoblastoma previously enucleated on 1 side (the prosthesis is visible). The remaining eye is a case of VP of drug delivery. A, The OA is successfully catheterized and used in 2 sessions of IAC because the choroidal blush (arrows) is regularly achieved. B–E, Third session of IAC. Selective angiography of the ICA does not show any visible OA (B). Nevertheless catheterization of the OA is successful (C), though the contrast medium flows back into the ICA (On-line Video). Superselective angiography of the MMA shows a good anastomotic pathway to the OA (D), which allows achieving the choroidal blush (arrows in E). F and G, Fourth session of IAC. This time the anastomosis between the MMA and the OA does not guarantee the choroidal blush. An alternative route for drug delivery through the ECA is sought and found between the frontal branch of the superficial temporal artery (arrows point to the microcatheter within the artery) and the supratrochlear artery (F). A later angiographic phase shows that this pathway guarantees the choroidal blush (arrows) (G). H–J, Fifth session of IAC. The anastomosis between the MMA and the OA is working again. However, the contrast medium flows back even into a large branch of the MMA (arrows in H). To reduce the volume of distribution, we glued the meningeal branch (arrows point to the cast in I), and the following injection of contrast medium achieves the choroidal blush (arrows in J).