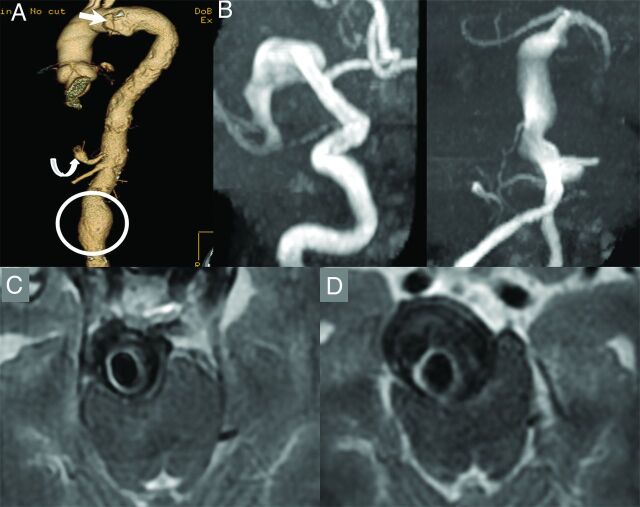
Fig 1.
A 67-year-old man who is a former smoker with a history of a penetrating atheromatous ulcer of the aortic arch (white arrow), a 5.6-cm abdominal aortic aneurysm (circle), and a celiac artery aneurysm (curved arrow, A). The patient had an episode of dizziness and headache and underwent a noncontrast CT of the head, which demonstrated enlarged intracranial arteries. An MRA demonstrated fusiform aneurysmal dilation of the entire right M1 segment measuring 10 mm in maximum diameter and a largely thrombosed fusiform aneurysm of the basilar artery, which measured 18 mm in maximum diameter (B and C). Approximately 9 months later, the aneurysm grew to 25 mm in diameter and started causing obstructive hydrocephalus (D). The patient also had a new perforator pontine infarct at the time (not shown). A programmable ventriculoperitoneal shunt was placed; however, the patient died due to complications of hydrocephalus 3 months later.