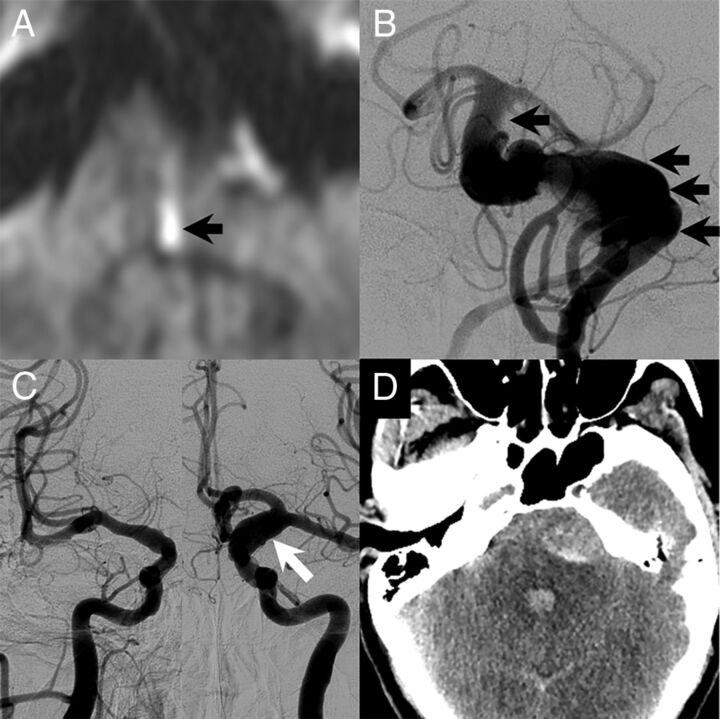
Fig 3.
A 51-year-old man with a long history of headaches with associated nausea and vomiting. He had acute-onset left-sided weakness with a prominent left facial droop along with left face, arm, and leg numbness and slurred speech. The patient had no family history of cerebral aneurysms, though his father had an abdominal aortic aneurysm. A, MR imaging at the time of the initial evaluation showed a medial left pontine infarct (black arrow). There was evidence of a large dolichoectatic aneurysm of the basilar artery on MR imaging, and the patient underwent cerebral angiography for further evaluation. B, Cerebral angiography demonstrated a fusiform-type aneurysm of the basilar artery with a filling defect that was consistent with thrombus (black arrows). The patient also had diffuse arteriomegaly with dilation of the right supraclinoid ICA to 6 mm and dilation of the left supraclinoid ICA to 10 mm (white arrow, C). D, The day following the angiography, the patient had a 10/10 headache. Noncontrast CT at the time showed diffuse subarachnoid hemorrhage with most of the blood products surrounding the basilar artery aneurysm. He died the next day.