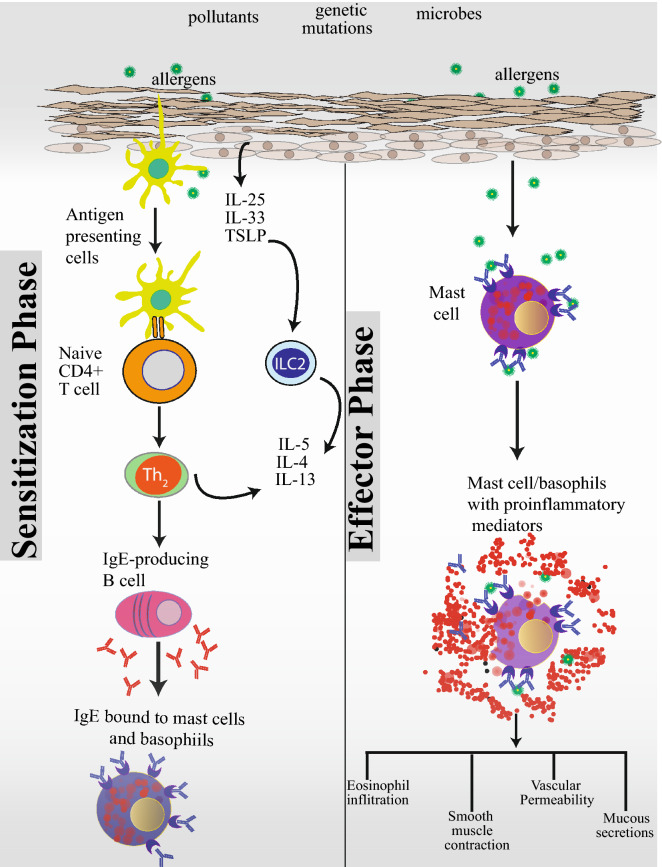
Fig. 1.
A dysfunctional skin barrier caused by exposure to pollutants, pathogenic microbes, and genetic mutations predisposes towards atopic sensitization, the first manifestation of which is atopic dermatitis. An impaired skin barrier releases proinflammatory epidermal cytokines, IL-25, IL-33, and TSLP. In this proinflammatory environment, resident antigen presenting cells further skew naïve T cells towards a Th2 proinflammatory state. ILC2 cells also play a key role in allergic sensitization. ILC2 cells are found near barrier surfaces and are activated by IL-33. Th2 and ILC2 cells produce a number of cytokines, key among them being IL-4, IL-5 and IL-13. In the presence of IL-4 and IL-13, B-cells undergo isotype class switching to IgE producing cells. IgE antibodies then bind to high-affinity FcεRI receptors on the surface of mast cells and basophils and prime these cells for future encounters with the allergen leading to a state of atopic sensitization. In sensitized individuals, subsequent encounters with an allergen leads to cross linking of IgE bound to FcεRI receptors and degranulation and release of proinflammatory mediators by basophils and mast cells leading to eosinophilic infiltration, smooth muscle contraction, vascular permeability, and mucous secretion