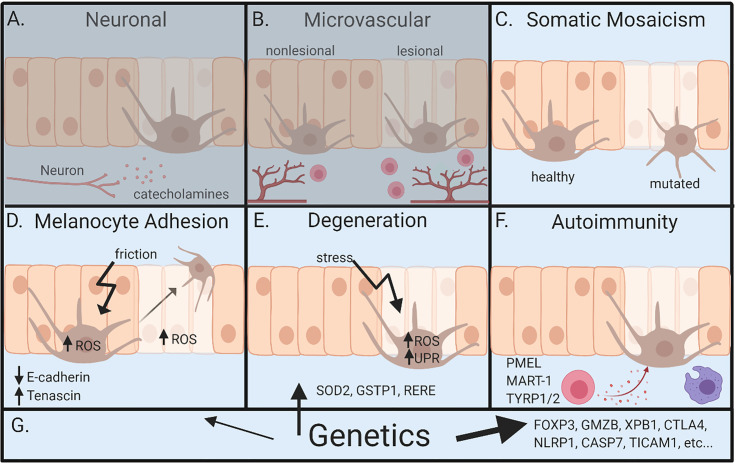
Figure 2.
Overview of pathogenesis for vitiligo. (A) Neuronal involvement – neurons within the skin release neuropeptides like catecholamines, which act on melanocytes and lead to depigmentation. (B) Microvascular theory – vitiligo lesions have increased blood flow during segmental vitiligo, which allows for increased infiltration of lymphocytes that results in autoimmune attack of melanocytes. (C) Somatic mosaicism – depigmentation develops because a somatic mutation in melanocytes leads to genetically distinct populations that are susceptible to autoimmune attack. (D) Melanocyte adhesion – friction or oxidative stress in melanocytes or keratinocytes leads to melanocyte loss because of reduced adhesion to the skin. (E) Degenerative theory – depigmentation occurs because of intrinsic melanocyte defects, such as increased susceptibility to environmental stressors and dysregulation of reactive oxidative species (ROS). (F) Autoimmunity theory – autoreactive immune cells attack and kill melanocytes, ultimately leading to depigmentation. (G) Genetics – underlies all pathways leading to vitiligo. Genetic studies most clearly implicate autoimmunity, but also melanocyte contributions. Neuronal and microvascular theories are least supported, represented by (A, B) being grayed. Figure created in BioRender.com.