SUMMARY:
Intracranial dissecting aneurysms constitute rare lesions with complex management and elevated morbidity and mortality. Results of 23 patients harboring such lesions treated with the PED are reported. Standard dual antiplatelet therapy was instituted. Neurologic and angiographic assessments were obtained at 3, 6, and 12 months. Clinical presentation included SAH (52%), symptoms of mass effect (22%), ischemia (4%), and incidental finding (22%). The posterior circulation was affected in 91% of cases. Total occlusion was demonstrated in 69.5% of patients, with an increment to 87.5% considering only patients with at least 3 months of follow-up. Small aneurysms demonstrated higher rates of total occlusion (6/7) compared with large (5/7) and giant (5/9) ones. Good clinical outcome was achieved in 74% of patients. Reconstructive endovascular treatment of intracranial dissecting aneurysms with the PED provided good clinical and angiographic results with acceptable risks, representing an attractive therapeutic option for this complex disease, especially when parent vessel preservation is mandatory.
Dissecting aneurysms of the intracranial circulation are uncommon, accounting for 3% of all cerebral aneurysms.1 They are significantly less frequent than saccular lesions but usually more difficult to treat, with a devastating natural history and up to 80% mortality in 5 years if left untreated. Dissecting aneurysms pose a great challenge to both surgical and endovascular treatments due to their location and anatomic configuration.
Clinical presentation includes symptoms related to mass effect, thromboembolic ischemia, and SAH. Ischemic events predominate in extracranial dissections, while hemorrhage usually results from intracranial lesions.1 Diagnosis is based on the classic angiographic pearl-and-string sign, with luminal dilation adjacent to a stenotic segment. MR imaging techniques are now replacing conventional angiography as the criterion standard for the diagnosis of arterial dissections, due to similar resolution and actual demonstration of the intramural hematoma.
To prevent artery occlusion or distal embolization, anticoagulation or antiaggregation has gained widespread acceptance for the treatment of arterial dissections. Nevertheless, these medications are not innocuous and may be sometimes ineffective in preventing symptomatic progression. On the other hand, in the setting of SAH, the high rate of rebleeding among patients treated conservatively argues for treatment in the acute phase.1 Additionally, it is uncommon for a dissecting aneurysm to resolve spontaneously or with medical treatment only, as seen with arterial dissections. Given this scenario, despite sharing the same etiology, arterial dissection and dissecting aneurysm respond differently to treatment and should be managed accordingly.
With the evolution of endovascular techniques, increasing effort has been made to preserve parent vessel patency when managing dissecting aneurysms, in contrast to deconstructive modalities of treatment usually applied to these lesions. Their higher incidence of recanalization after coiling, compared with saccular aneurysms, has prompted the use of stent-assisted techniques in an effort to obtain definitive occlusion. Better results might be expected with flow diverters. We report our experience using the PED (Chestnut Medical Technologies, Menlo Park, California) for the endovascular treatment of dissecting intracranial aneurysms.
Case Series
Studied Population
The present study is a retrospective all-inclusive case series of patients treated with the PED for dissecting aneurysms from October 2007 to September 2010. Those lesions were considered to be dissecting when associated with 1 or both of the following conditions: 1) intimal flap and irregular parent artery narrowing, and 2) false lumen and/or intramural hematoma involving the parent artery, confirmed by MR imaging.
Because the PED was an investigational device, its application in this series was always prospectively approved by our institutional ethics committee, either on a case-by-case basis (compassionate use) or within the context of the Pipeline Embolization Device in the Intracranial Treatment of Aneurysms trial.2 Written informed consent was obtained from every patient.
Antiplatelet Therapy
Patients treated electively were preloaded with 75 mg of clopidogrel and 100 mg of aspirin daily at least 72 hours before PED deployment. Four patients were treated in the setting of acute SAH and, therefore, received a 300-mg loading dose of clopidogrel pretreatment. Dual antiplatelet medication was maintained in all patients for at least 6 months after the procedure, followed by continuous single therapy with aspirin lifelong. Intravenous heparin was administered during surgery to maintain an activated clotting time between 250 and 300 seconds. Heparinization was not reversed at the end of the procedure.
PED
The PED is a flexible microcatheter-delivered self-expanding endovascular stent-like construct engineered specifically for the treatment of cerebral aneurysms. It consists of a braided mesh cylinder composed of 48 individual platinum and cobalt chromium microfilaments. The stent is mounted in a recess on a flexible delivery wire and is front-loaded via an introducer and delivered through a standard 0.027-inch-internal-diameter microcatheter.3
Procedure
Treatments were performed with the patient under general anesthesia, via a transfemoral arterial approach. Simultaneous aneurysm coil embolization, usually reserved for previously ruptured lesions, was performed before deployment of the PED only in the absence of intra-aneurysm thrombus. Partially thrombosed lesions were coiled through a jailed microcatheter after delivery of the PED across the aneurysm neck. This jailing technique allowed for easy microcatheter removal through gentle retraction, with no construct disruption.
All PEDs were deployed following a standard procedure.3 First, the microcatheter was manipulated under high-magnification fluoroscopic roadmap control across the aneurysm neck. The PED, mounted on a delivery wire and constrained within a sheath, was then inserted into the rotating hemostatic valve and introduced into the hub of the microcatheter. By pushing the delivery wire, we advanced the PED through the microcatheter into position for deployment. Through a combination of forward pressure on the delivery wire and retraction on the microcatheter, the device was deployed, expanding to release from the delivery microwire. When constrained within a microcatheter, the PED is elongated 2.5 times its maximally expanded deployed configuration. This foreshortening must be taken into account during positioning and deployment of the construct.
Procedural Assessment and Follow-Up
Technical success was defined as PED deployment with complete coverage of the aneurysm neck, preserved patency of the parent artery, and no clinically evident adverse event. Clinical evaluation was always performed at discharge; concurrent clinical and angiographic follow-ups were usually performed at 3, 6, and 12 months after treatment. An independent neurologist was responsible for neurologic assessment. Angiographic follow-up included the standard projections as well as the working angle for PED deployment. The primary angiographic end point was complete aneurysm occlusion. Any residual filling of the lesion was interpreted as incomplete occlusion.
Results
Patient characteristics are summarized in the On-line Table, including clinical presentation, aneurysm size and location, the number of devices implanted during treatment, the length of follow-up, best angiographic result, and GOS score.
Over a 36-month study period, 23 patients (12 female) harboring 23 dissecting aneurysms were treated with the PED. Age ranged from 5 to 79 years (average, 50 years). The most common clinical presentation was SAH (52%), but only 4 of those patients were treated in the acute setting of hemorrhage. Five aneurysms were found incidentally (22%), another 5 presented with symptoms of mass effect (22%), and 1, of cerebellar ischemia (4%).
Most of those dissecting dilations compromised the intradural segment of the vertebral artery (39%), followed by the basilar trunk (26%), vertebrobasilar junction (13%), basilar tip/P1 segment (9%), and PICA (4%, Fig 1). Only 2 lesions were found in the anterior circulation, 1 in the supraclinoid ICA and the other 1 in proximal middle cerebral artery. Seven aneurysms were classified as small (<10 mm); 7 as large (10 to 25 mm), and 9 as giant (>25 mm). Partially thrombosed lesions represented 26% of this series (1 large and 5 giant).
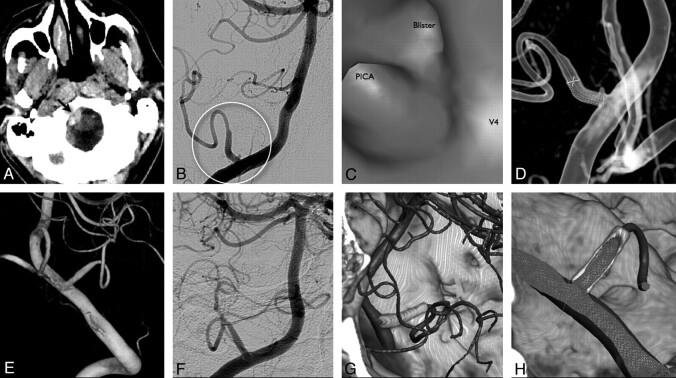
Fig 1.
This 33-year-old man (patient 16) presented with headache 2 days following an episode of mild head trauma. A, Brain CT demonstrates a small hematoma adjacent to the brain stem. Both CTA and MR angiography were negative for vascular abnormalities. B, Cerebral DSA shows an atypical fusiform dilation of the proximal segment of the PICA, associated with a blister-like aneurysm intimately related to the previous hemorrhage site. C and D, This lesion, probably dissecting in origin, is also demonstrated by tridimensional virtual EndoView (C) and was treated 1 week after ictus with a single PED (D). E−H, Immediate control 3D DSA confirms adequate endoluminal reconstruction of the PICA (E), which remains stable 9 months after treatment (F−H).
Mean follow-up time was 6 months (1–18 months). Total angiographic occlusion was observed in 16 patients (69.5%). However, when considering only patients with at least 3 months of follow-up, this percentage increased to 87.5% (14 of 16 patients). Small aneurysms demonstrated higher indices of total occlusion (85.7%) compared with large (71.5%) and giant (55.5%) ones. Once total angiographic occlusion had been achieved, no sign of recanalization was observed. Side branches and perforators covered during treatment remained patent at follow-up.
A total of 51 devices were used to treat 23 dissecting aneurysms, and 46 of these were successfully deployed on the first attempt (90% of technical success). One device fell into the aneurysm sac, 2 slipped proximally during deployment, and 2 presented exaggerated shortening while compacting, missing total neck coverage, which required deployment of an additional PED. Multiple implants were intentionally used in large and giant fusiform lesions that had bled before, with the expectation of enhancing the flow-diverting effect and eventually accelerating the healing process. Simultaneous coiling was performed in 9 patients, most in previously ruptured large (n = 3) and giant (n = 4) lesions. Incidental aneurysms were all treated with PED alone. Three patients had been previously treated with other stents and coils. Two small basilar aneurysms managed with Neuroform microstents (Boston Scientific, Natick, Massachusetts) were totally occluded after PED deployment; 1 giant vertebral lesion, which had previously received 1 LEO stent (Balt Extrusion, Montmorency, France), remained open 18 months after PED deployment. Asymptomatic intrastent stenosis was observed in 2 patients, both previously treated with 1 single PED. One showed complete resolution in 12 months, and the other remained stable, not requiring therapy (Fig 2).
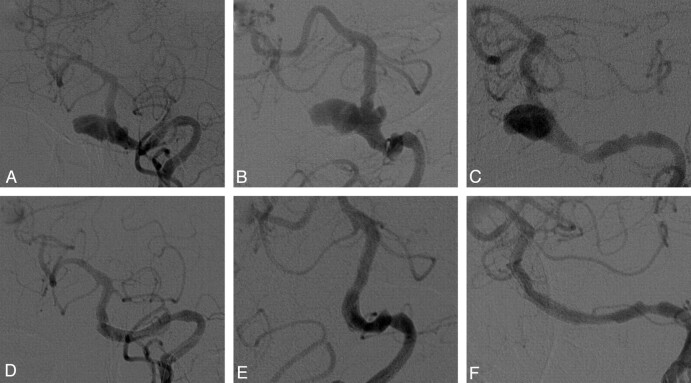
Fig 2.
A−C, A 72-year-old man (patient 5) harboring this large incidental dissecting aneurysm of the proximal basilar trunk is treated with a single PED, with favorable outcome. Six-month control angiogram shows adequate parent vessel reconstruction, despite the persistence of a proximal stenotic segment and signs of mild intrastent hyperplasia. The patient remains asymptomatic, not requiring further treatment. D−F, After 18 months of follow-up, the angiographic findings remain unchanged, with stable aneurysm occlusion.
Good clinical outcome (GOS scores of 4 and 5) was achieved in 74% of patients. One presented with a retroperitoneal hematoma, and 1 experienced a thromboembolic complication (ipsilateral cerebellar stroke after stent placement and coiling of a giant partially thrombosed vertebral dissecting aneurysm), both with complete recovery. Residual deficits were related to neurologic conditions preceding treatment. Two patients died from late complications of SAH. There was no sign of aneurysm rupture following treatment with PED in this series.
Discussion
When facing an intracranial dissecting aneurysm, the physician must consider some key features that differentiate this lesion from both saccular aneurysms and nonaneurysm arterial dissections. First, the favorable outcome of arterial dissections with medical therapy alone is not observed in dissecting intracranial aneurysms, which tend to keep growing and eventually bleed. Second, ruptured lesions carry an extremely high rate of rebleeding, requiring urgent treatment. Due to its dissecting nature, wall friability can make surgical clipping difficult and even risky. On the other hand, recanalization after coiling alone is almost certain. Therefore, deconstructive modalities of treatment like trapping or parent vessel occlusion, performed either surgically or endovascularly, have predominated for managing those lesions, usually with good results.1,4 However, in situations in which parent artery preservation is mandatory, the use of stent-assisted techniques may be the most adequate choice.5
Stent technology has evolved to include the treatment of intracranial aneurysms, which leads to neointimal formation and provides an endoluminal matrix for endothelial growth and vessel remodeling. It can also change inflow within the lesion, promoting saccular thrombosis, though the role of this phenomenon in clinical practice may be limited by the high porosity of currently available stents. The PED has been designed to address this issue, with much more effective flow diversion capability and very promising preliminary results.3,6 In addition, when treating a dissecting aneurysm, proper stent placement may help to reattach the dissected arterial flap, thus closing off the false lumen and favoring healing.
Topographic distribution and clinical presentation in this studied population properly exemplified the usual characteristics of intracranial dissecting aneurysms, which predominate in the posterior circulation and are usually diagnosed after bleeding. The elevated number of devices required for treatment reflects the high proportion of large and giant as well as previously ruptured lesions included in the analysis. Because most were electively treated, good clinical outcomes were obtained in most patients, with acceptable morbidity (8.7%). The ischemic postoperative complication experienced was probably due to distal embolization from a partially thrombosed giant lesion, though perforating compromise could not be ruled out. Both deaths in this series were not attributed to the endovascular procedure.
Given total occlusion rates of coiled saccular aneurysms reported in the current literature (from 19% to 66%),7 the greater tendency for recanalization of dissecting compared with saccular lesions, and the high number of large and giant aneurysms in the studied group (almost 70%), which are known to have worse angiographic results, we think that the 69.5% of global occlusion presented here represents a good result for the treatment of this complex disease. Furthermore, as previously reported,3 better results observed with longer follow-up testify to the efficacy of the PED, providing progressive intra-aneurysm thrombosis and final stable occlusion. Unfortunately, 5 of the studied patients have not had any follow-up angiogram obtained (2 patients died due to complications of severe pretreatment SAH, another 2 were lost during follow-up, and 1 refused to undergo any control study), which left us with only their immediate postoperative angiogram for analysis. Angiograms obtained after 6 months of PED deployment demonstrated 90% (9/10) complete aneurysm occlusion. After 12 months, the only lesion that remained opened was a giant vertebral aneurysm previously treated with coils and a stent (LEO, Balt), which has also been demonstrated to impair progression to cure after treatment with the PED.3
Overall, 7 aneurysms (30%) remained opened after treatment, 5 with no angiographic control. Progression to total occlusion is expected with longer follow-up. Nevertheless, these patients remain susceptible to hemorrhage. Parent vessel sacrifice could have been considered in some of those lesions, possibly with higher rates of complete obliteration.4 However, deconstructive techniques are not always tolerated, with severe late complications even following a negative balloon test occlusion and favorable clinical outcomes usually limited to ICA and vertebral lesions, more amenable to total thrombosis.
Recent reports of delayed rupture after treatment with flow diverters have considered a potential aggressive autolytic effect of unstable clot on the aneurysm wall.8 Hemodynamic changes have also been implicated in bleeding cases.9 Fortunately, we have not experienced such hemorrhagic complications, which could be the result of our limited follow-up, small amount of partially thrombosed lesions, simultaneous coiling, and the frequent use of multiple devices in this series.
Conclusions
Reconstructive endovascular treatment of intracranial dissecting aneurysms with the PED provided good clinical and angiographic results with acceptable risks, especially when considering the high morbidity and mortality associated with this complex disease, as well as the limited results obtained with other currently available therapeutic strategies. Curative reconstruction has been obtained in most patients with midterm follow-up, probably representing one of the best options of treatment in cases in which parent vessel preservation is mandatory. Clinical trials enrolling larger numbers of patients with long-term follow-up are necessary to confirm this hypothesis.
Supplementary Material
ABBREVIATIONS
- DSA
digital subtraction angiography
- GOS
Glasgow Outcome Score
- ICA
internal carotid artery
- PED
Pipeline Embolization Device
- PICA
posterior inferior cerebellar artery
- SAH
subarachnoid hemorrhage
Footnotes
Disclosures: Pedro Lylyk: Research Support (including provision of equipment or materials): Boston Scientific, Cordis, Microvention; Consultant: Chestnut Medical.
References
- 1. Santos-Franco JA, Zenteno M, Lee A. Dissecting aneurysms of the vertebrobasilar system: a comprehensive review on natural history and treatment options. Neurosurg Rev 2008;31:131–40, discussion 140 [DOI] [PubMed] [Google Scholar]
- 2. Nelson PK, Lylyk P, Szikora I, et al. The Pipeline embolization device for the Intracranial Treatment of Aneurysms Trial. AJNR Am J Neuroradiol 2011;32:34–40. Epub 2010 Dec 9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lylyk P, Miranda C, Ceratto R, et al. Curative endovascular reconstruction of cerebral aneurysms with the Pipeline embolization device: the Buenos Aires experience. Neurosurgery 2009;64:632–42, discussion 642–43, quiz N6 [DOI] [PubMed] [Google Scholar]
- 4. Steinberg GK, Drake CG, Peerless SJ. Deliberate basilar or vertebral artery occlusion in the treatment of intracranial aneurysms: immediate results and long-term outcome in 201 patients. J Neurosurg 1993;79:161–73 [DOI] [PubMed] [Google Scholar]
- 5. Wakhloo AK, Mandell J, Gounis MJ, et al. Stent-assisted reconstructive endovascular repair of cranial fusiform atherosclerotic and dissecting aneurysms: long-term clinical and angiographic follow-up. Stroke 2008;39:3288–96 [DOI] [PubMed] [Google Scholar]
- 6. Szikora I, Berentei Z, Kulcsar Z, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the Pipeline embolization device. AJNR Am J Neuroradiol 2010;31:1139–47. Epub 2010 Feb 11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Raymond J, Guilbert F, Weill A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 2003;34:1398–403 [DOI] [PubMed] [Google Scholar]
- 8. Kulcsár Z, Houdart E, Bonafé A, et al. Intra-aneurysmal thrombosis as a possible cause of delayed aneurysm rupture after flow-diversion treatment. AJNR Am J Neuroradiol 2011;32:20–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cebral JR, Mut F, Raschi M, et al. Aneurysm rupture following treatment with flow-diverting stents: computational hemodynamics analysis of treatment. AJNR Am J Neuroradiol 2011;32:27–33. Epub 2010 Nov 11 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.