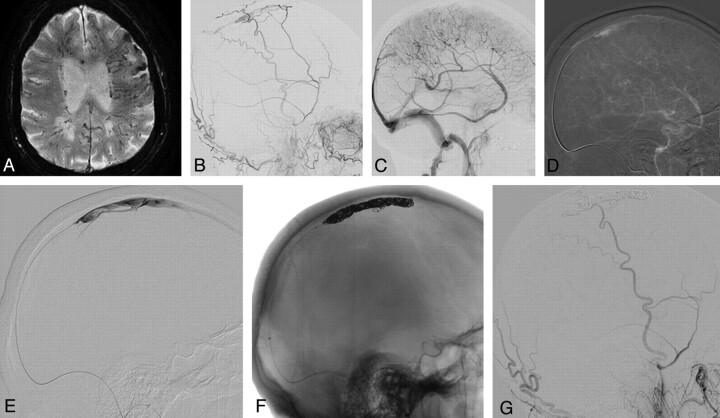
Fig 3.
Dural AVF of an isolated SSS with cortical venous reflux. An 87-year-old man presented with seizure, alteration of consciousness, and progressive weakness of his right hand. A, A T2 gradient-echo sequence demonstrates multiple dilated transmedullary veins and cortical microhemorrhages as a sign of chronic venous congestion. B and C, ECA (B) and ICA (C) runs demonstrate a DAVF into the SSS with occlusion at the distal third of the SSS with venous congestion. A 6F Shuttle-SL guide sheath (Cook, Bloomington, Indiana) is placed into the right jugular bulb, and a 6F Neuron (Penumbra, Alameda, California) catheter is advanced into the proximal SSS. D, From here, a 0.035-inch guidewire is advanced into the venous pouch. E–G, Via the thus-opened track, a microcatheter is advanced (E) with confirmation of the tip of the catheter in the SSS, and complete occlusion of the isolated sinus with coils is performed (F), leading to complete obliteration of the DAVF (G).