Abstract
BACKGROUND AND PURPOSE:
Stent-assisted endovascular treatment and flow diversion techniques are increasingly used for the management of wide-neck intracranial aneurysms. We report our initial clinical experience using a new flow diversion technique for the endovascular management of bifurcation aneurysms.
MATERIALS AND METHODS:
Eight bifurcation aneurysms were treated by placing 2 stents in Y-configuration with no accompanying endosaccular packing. This treatment technique aimed at flow diversion was selected in these cases because 1) the aneurysm was giant and causing mass effect, 2) the emanating branches were incorporated within the sac, or 3) the aneurysm was too small. Aneurysms were located at middle cerebral (5 aneurysms) and basilar artery bifurcations (3 aneurysms). Five aneurysms were small, 1 was large, and 2 were partially thrombosed giant. Closed-cell stents were used in all Y-stent placement procedures.
RESULTS:
In all aneurysms, both stents could be placed at the intended locations without any procedural complication. Follow-up angiograms obtained at 3 months to 2 years demonstrated that all stents were patent except for one with asymptomatic P1 occlusion. Complete occlusion with remodelled bifurcation was observed in all middle cerebral artery bifurcation aneurysms and the large basilar tip aneurysm. Residual filling despite reduction in size was observed in both of the partially thrombosed giant aneurysms at 2-year and 3-month follow-up angiograms, respectively.
CONCLUSIONS:
Flow diversion with double stent placement in Y-configuration provided successful and stable aneurysm occlusion. The technical and clinical results achieved are highly encouraging that this technique may contribute to the endovascular treatment of these complex bifurcation aneurysms.
The use of self-expanding neurovascular stents solely or in combination with endosaccular coiling has been reported to be feasible and effective in endovascular treatment of wide-neck or fusiform intracranial aneurysms.1–11 However, wide-neck aneurysms located at the arterial bifurcations, especially in the aneurysms where the bifurcating branches emanate directly from the base of the aneurysm, may still not be amenable to being treated by using a single stent. Recently, Y-configuration double stent-assisted coil embolization (open-cell design Neuroform stent; Boston Scientific, Natick, Massachusetts) was reported to be a safe and effective option for the endovascular treatment of these bifurcation aneurysms.12–15 By deploying 2 stents in a Y-configuration, complete coil embolization of these difficult aneurysms could be accomplished while preserving the parent circulation.13 In an experimental study designed to assess the changes in the hemodynamic forces acting on a bifurcating aneurysm model after stent placement with a Y-configuration, marked reduction in the residual motion inside the aneurysm sac together with the associated large reduction in the velocity and shear stress inside the sac were shown, and these findings have inspired us with the possibility of the mere use of stents, without endosaccular coil packing, as a viable therapy for some aneurysms.16
We report, to our knowledge, the first case series where a novel “Y” stent flow diversion technique was used for management of 8 bifurcation aneurysms without endosaccular coiling. Furthermore, this is the first report of successful Y-stent–assisted treatment of wide-neck bifurcation aneurysms by using the Enterprise stent (Cordis Neurovascular, Miami Lakes, Florida) with a closed-cell design.
Materials and Methods
Case Reports and Description of Technique
Eight patients (5 men, 3 women) with an age range of 41–53 years (mean age, 46.6 years) harboring 8 wide-neck bifurcation aneurysms were treated by using the sole Y-stent placement technique (Table). All patients were premedicated with antiplatelet therapy consisting of 300 mg/day aspirin and a loading dose of 300–450 mg of clopidogrel 1 to 7 days before the procedure, followed by 75 mg/day. We investigated the clopidogrel response by using the rapid platelet function assay VerifyNow P2Y12 (Accumetrics, San Diego, California) before the procedure, and a ratio of 40% or more was obtained in all patients. Of the 8 aneurysms, 5 were located at the MCA bifurcation and 3 at the basilar tip. Aneurysm sizes were classified as small (<1 cm), large (1–2.5 cm), and giant (>2.5 cm). In this series, 5 of the aneurysms were small, 1 was large, and 2 were partially thrombosed giant. In all but the first case, the primary aim was achieving aneurysmal thrombosis by using hemodynamic effects of Y-stent placement without endosaccular coiling. In the first case, the initial treatment plan had been Y-stent–assisted coiling; however, the microcatheter that had been jailed within the aneurysm sac before stent placement was kicked out of the sac while performing Y-stent placement, and catheterization of the sac after stent placement failed. The operator decided to stage the treatment (case 1).
Summary of relevant clinical and angiographic data in 8 patients with wide-neck bifurcation aneurysms treated using Y-stent flow diversion technique
| Case No. | Age (yr), Sex | Aneurysm Location | Aneurysm Type | Aneurysm Size | Microcatheter Jail before Stent Placement | Latest Angiographic Follow-Up | Final Angiographic Result | Initial Presentation | Final Clinical Result (modified Rankin Scale) |
|---|---|---|---|---|---|---|---|---|---|
| 1a | 50, M | MCA bifurcation | R | Small | Yes | 1 yr | Complete occlusion | SAH, failed surgical clipping | 0 |
| 2 | 48, M | Basilar tip | R | Large | No | 2 yr | Complete occlusion | SAH, medical treatment, headache | 0 |
| 3b | 41, F | Basilar tip | U | Giant | No | 2 yr | Residual filling | Mass effect, aglutition | 0 |
| 4 | 53, M | MCA bifurcation | U | Small | Yes | 1 yr | Complete occlusion | Asymptomatic | 0 |
| 5 | 49, M | MCA bifurcation | U | Small | No | 1 yr | Complete occlusion | Headache | 0 |
| 6 | 44, F | MCA bifurcation | U | Small | No | 6 mo | Complete occlusion | Headache | 0 |
| 7 | 43, M | MCA bifurcation | U | Small | No | 6 mo | Complete occlusion | Asymptomatic | 0 |
| 8 | 45, F | Basilar tip | U | Giant | No | 3 mo | Residual filling | Headache, mass effect, aglutition, and ptosis | 1 |
Patient had a previous failed surgical treatment attempt.
Patient needed additional coiling.
All procedures were performed under general anesthesia. A 6F guiding catheter was introduced into the ICA for MCA bifurcation aneurysms and into the VA for basilar bifurcation aneurysms. Using 3D rotational angiography with reconstruction images and the working projections obtained from these, the more challenging bifurcating branch (ie, the branch with a more acute angle relative to the main trunk) was selected to be catheterized first by using a technique described previously.17 Under roadmap guidance, a Prowler Select Plus (Cordis) microcatheter with a 0.016-inch microguidewire (Terumo, Tokyo, Japan) was used to select the designated branch. In 2 cases, an SL-10 microcatheter with a 0.012-inch microguidewire (Terumo) was used to catheterize the aneurysm sac and jailed before deploying the first stent. Then, the first Enterprise stent was deployed in the first branch extending down to the main artery. A Prowler Select Plus microcatheter was advanced over the pusher of the stent to position at the bifurcation point so that the catheter was safely inside the proximal part of the first stent. Then, the pusher was withdrawn, and the 0.016-inch guidewire was used once more to select the second bifurcating branch through the interstices of the first stent. After catheterization of the second branch, the second Enterprise stent was deployed with half of the stent in the second branch and the other half within the lumen of the previously placed stent. All patients received intravenous heparin with the goal of elevating the activated clotting time to 2 to 3 times the baseline value during the procedure, and the heparin was not reversed at the end of the procedure. Puncture site hemostasis was achieved by using vascular closure devices. Three patients with large and giant basilar bifurcation aneurysms received 16 mg/day intravenous dexamethasone for 1 week after the procedure, to prevent acute edema and mass effect on the brain stem that may develop due to rapid aneurysmal thrombosis. All patients were discharged on life-long aspirin and clopidogrel for 6 months.
Illustrative Cases
Case 1.
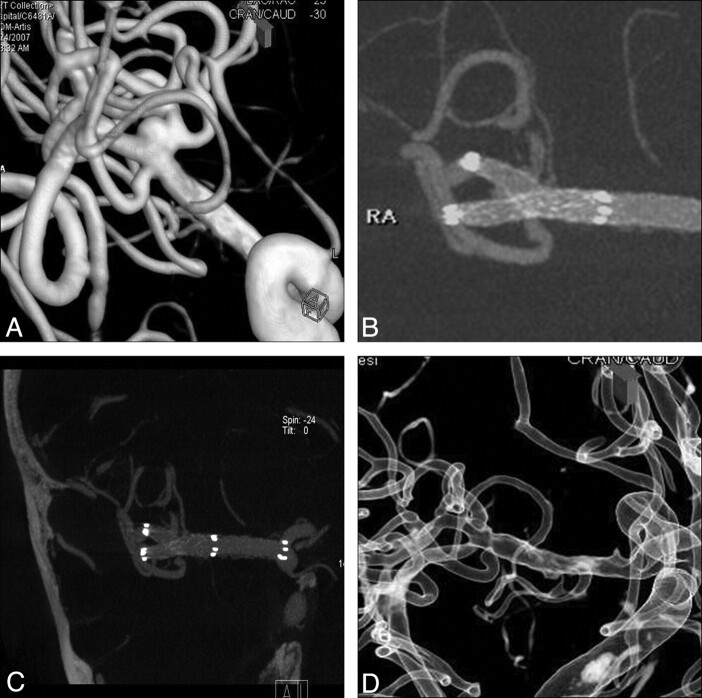
A 38-year-old man with a ruptured right MCA bifurcation aneurysm of 4-mm diameter had a history of failed surgical clipping (only wrapping could be performed) and was referred to our center for endovascular treatment. Because it was a very wide-neck and shallow aneurysm, balloon or single stent-assisted coiling was thought to be inadequate to protect both MCA branches from coil protrusion, thus Y-stent–assisted coiling was planned. After placing the Prowler Select Plus microcatheter into the superior trunk, an SL-10 microcatheter was placed into the aneurysm sac before deployment of the first stent. The first stent was deployed successfully in the superior trunk, jailing the SL-10 microcatheter between the stent and M1 segment. Then, while attempting to catheterize the inferior trunk, the SL-10 microcatheter was kicked backed from the sac because of the interaction between the 2 microcatheters. After withdrawing the SL-10 microcatheter, the second stent could be placed within the inferior trunk without any difficulties. Control angiogram after deployment of both stents revealed significant reduction of contrast filling of the aneurysm. Catheterization of the aneurysm sac was tried gently, but because there was resistance while the microcatheter was being pushed through the stent struts, the operator did not want to force and decided to stage the treatment. When the patient was taken to the angiography suite to complete the treatment in the first month, the aneurysm was found to show total occlusion. The 1-year control angiography confirmed the stable complete occlusion of the aneurysm (Fig 1).
Fig 1.
Initial 3D reconstruction image of rotational angiogram (A) shows small wide-neck MCA trifurcation aneurysm. Posttreatment 3D reconstruction image of flat panel CTA (B) demonstrates the Y-configuration of the 2 stents placed within the MCA branches crossing the neck of the aneurysm, which is still filling in between. 3D reconstruction image of the flat panel CTA (C) obtained at 1-month control and 3D image of rotational angiogram at 1-year control (D) showing complete occlusion of the aneurysm and reconstruction of the trifurcation.
Case 2.
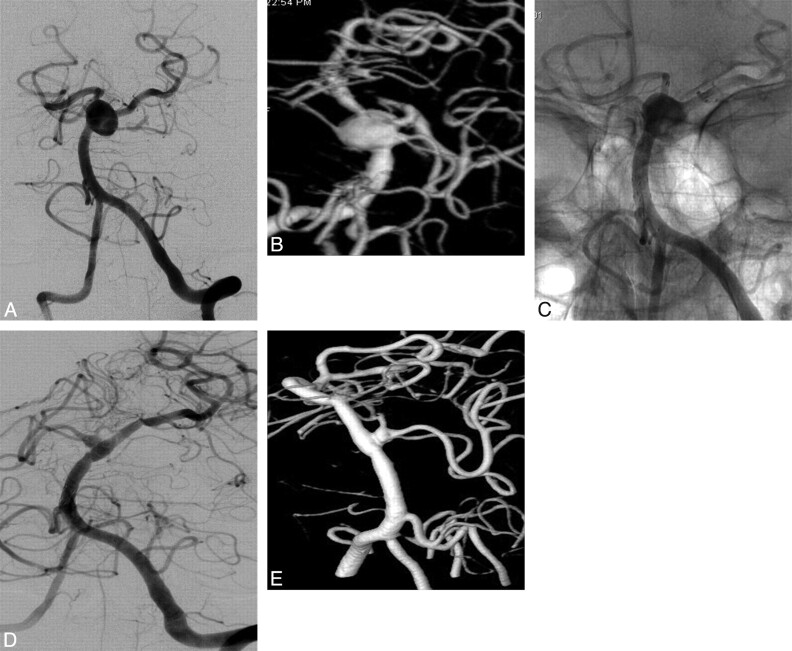
A complex basilar bifurcation aneurysm with a diameter of 14 mm, which both PCAs and SCAs were emanating directly from the aneurysm, was diagnosed in a 45-year-old man with a past history of SAH (>1 year ago) and severe headache. He received only medical treatment during the acute stage of SAH. Y-stent flow diversion technique was the primary goal for this aneurysm to achieve aneurysmal thrombosis with a remodeled bifurcation because there was neither a definable aneurysm neck nor a sac to be coiled. The 1-month control CTA showed occlusion of the aneurysm with remodelled basilar tip; the stent segment within the right P1 was not filling with contrast and the distal PCA was filling via right PcomA. The patient did not have any relevant symptoms. The basilar trunk and left PCA were patent. The 6-month and 2-year control angiograms revealed stable complete occlusion of the aneurysm and completely remodeled basilar bifurcation (Fig 2).
Fig 2.
Pretreatment left vertebral artery angiogram in oblique projection (A) and 3D reconstruction image of rotational angiogram (B) show the basilar tip aneurysm without a definable neck. Posttreatment angiogram (C), nonsubtracted view, shows the “Y”-configured stents extending into the both posterior cerebral arteries from the basilar trunk. The 2-year follow-up angiogram (D) and 3D reconstruction image of rotational angiogram (E) demonstrate completely remodeled basilar bifurcation with the aneurysm sac disappeared and occlusion of the right P1.
Case 3.
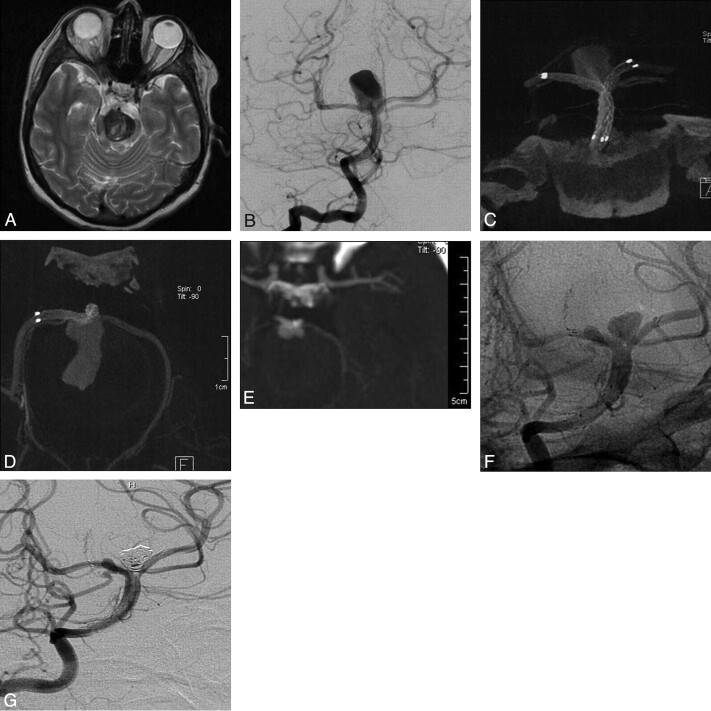
A 48-year-old woman was admitted to our hospital with headache, lethargy, aglutition, and right sixth and seventh nerve palsies that started 3 days before admission. MR imaging showed a giant (3 cm in diameter), partially thrombosed basilar bifurcation aneurysm having a significant mass effect on brain stem. The primary goal of flow diversion with Y-stent placement in this patient was leading to aneurysmal thrombosis without packing the sac, which could aggravate the mass effect on the brain stem and cause worsening of the patient's symptoms. Two weeks after a successful Y-stent placement procedure, the patient was neurologically intact with the symptoms due to mass effect resolved. The 1-month control CTA showed significant decrease in size of the patent aneurysm lumen. The 1-year control angiogram showed progressive thrombosis and change in the shape of the aneurysm sac so that it became a bilobulated, small aneurysm. The 2-year control angiogram showed no further thrombosis so the remaining larger lobule was occluded with coil packing. The smaller lobule is still being followed (Fig 3).
Fig 3.
T2-weighted axial MR image (A) shows the giant basilar tip aneurysm causing mass effect and increased signal intensity in the brain stem. Pretreatment right vertebral artery angiogram in Towne projection (B) demonstrates the large and wide-neck basilar tip aneurysm. Posttreatment coronal (C) and axial (D) 3D reconstruction images of flat panel CTA demonstrate the “Y”-configuration of double stent placement. The 1-month follow-up axial CTA image (E) shows the significant decrease in size of the patent aneurysm lumen. The 2-year control angiogram (F), nonsubtracted view, shows progressive thrombosis and change in the shape of the aneurysm sac so that it became a bilobulated, small aneurysm. The larger lobule was coiled in the same session, and the small lobule is still being followed. G, Angiogram, subtracted image obtained after coiling.
Results
All patients were successfully treated by using this technique with no procedural complications, such as thromboemboli, arterial dissections and ruptures, or spasms. Of the 8 aneurysms, 1 MCA bifurcation and 1 basilar tip aneurysm had had previous rupture. The patient with the MCA bifurcation aneurysm underwent a subsequent surgical clipping, but the clipping attempt failed and the aneurysm was wrapped. The patient with the basilar tip aneurysm received only medical treatment during the acute phase of SAH. Both of these patients were referred to our center for endovascular treatment almost a year after SAH with no neurologic deficit. Two patients with partially thrombosed giant basilar tip aneurysms presented with cranial nerve deficits due to the mass effect of the aneurysms to the brain stem. Other patients had no neurologic deficits.
According to the immediate postoperative angiograms, reduced contrast filling was observed in all aneurysms with significant contrast stagnation within the sac in 3 large-to-giant basilar tip aneurysms. One of the 2 patients who presented with cranial nerve palsies became neurologically intact with no remaining mass effect signs 2 weeks after the procedure. The other patient developed hydrocephalus, and a ventriculoperitoneal shunt surgery was necessary. Her symptoms due to mass effect improved with remaining partial third nerve palsy.
All patients underwent follow-up CTA at 1 month (except for the patient in case 1 who had DSA) and DSA at 3 months to 2 years. Based on the latest follow-up, a 3-month follow-up angiogram was obtained in 1 patient, a 6-month follow-up in 2 patients, a 1-year follow-up in 3 patients, and a 2-year follow-up in 2 patients. Complete occlusion with remodelled bifurcation was observed in all MCA bifurcation aneurysms and the large basilar tip aneurysm (illustrative case 2) at the latest follow-ups. In this case with completely remodelled basilar tip, the right arm of the stent (right P1) was also asymptomatically occluded as described above. The 1-month CTA control showed significant and slight reduction in size for both of the giant basilar tip aneurysms, respectively. The 1-year control angiogram of the former aneurysm showed progressive thrombosis and a change in the shape of the aneurysm sac so that it became a bilobulated (heart-shaped) small aneurysm. The 2-year control angiogram showed no further thrombosis, so the larger lobule was treated with coil packing. The smaller lobule is still being followed, and the patient has remained symptom free so far. The latest follow-up angiogram for the latter aneurysm was obtained at 3 months, and a significant reduction in size was observed with residual filling. This aneurysm is still being followed.
Discussion
Since the development of self-expandable neurovascular stents, stent-assisted embolization techniques are being used increasingly for the endovascular treatment of wide-neck or fusiform intracranial aneurysms. In addition to their role of supporting aneurysm packing, they produce flow redirection and stent-induced endothelialization, providing reconstruction of the diseased parent artery. The evidence of spontaneous aneurysmal thrombosis by using sole stent placement technique without additional endosaccular packing was reported previously.1,2,9,11,18–20 Hemodynamic effects of the stents in the endovascular treatment of aneurysms include disruption of intra-aneurysmal flow pattern, resulting in turbulence, and production of blood stasis within the aneurysm, resulting in aneurysmal thrombosis. Moreover, aneurysm hemodynamic parameters were reported to be significantly modified by placement of multiple stents compared with single stent placement.21 Zenteno et al10 reported their series of 20 patients with aneurysms located at the posterior circulation treated by using the sole stent placement technique with an occlusion rate of 80% at the 1-year follow-up. Crowley et al22 described the multiple “in-stent stents” technique used to treat a fusiform basilar artery aneurysm, which resulted in almost complete occlusion at the 4-month control angiogram.
Flow diversion techniques ensured a new philosophy in endovascular treatment of complex, dissecting, wide-neck or fusiform aneurysms that were not amenable to other surgical or endovascular treatment strategies. Recently, new embolization devices are being used, designed primarily to hemodynamically exclude the aneurysm from the circulation and to achieve the curative reconstruction of the parent arteries.23,24 In an experimental study on a bifurcating aneurysm model in which Y-configured stents were placed, marked reduction in the residual motion inside the aneurysm sac together with the associated large reduction in the velocity and shear stress inside the sac was shown. This information encouraged us to use the Y-configured stents without endosaccular coil packing as a viable therapy for some aneurysms.16 However, to our knowledge, this is the first clinical report on the use of flow diversion effect of Y-stent placement for bifurcation aneurysms. Also, the safety and efficacy of the flow diversion devices at the bifurcations have not been demonstrated yet, unlike for sidewall aneurysms.23,24 Moreover, as distinct from the previously reported Y-stent–assisted embolization techniques, a closed-cell design self-expandable stent was used in all patients in our series.
Our first experience with this technique (illustrative case 1) was rather serendipitous because the previously jailed microcatheter within the aneurysm sac was kicked out during stent deployment, and the attempt at catheterization after Y-stent placement failed. However, after deployment of the second stent, significant reduction in contrast filling of the aneurysm sac was noted and that was why we decided not to force the catheterization and eventually staged the treatment. The 6-month control angiogram revealed complete occlusion of the aneurysm, leading us to use this technique in selected cases. We preferred to use the technique 1) in the bifurcation aneurysms in which we would not perform endosaccular packing due to small size or shape; or 2) due to the concern of increasing mass effect in large and giant aneurysms; when the aneurysm was too small to be coiled; or 3) when there was no definable neck with the main branches emanating directly from the aneurysm. In all patients but 2, aneurysms were completely occluded, and the bifurcations were remodeled at the 3-month to 2-year control angiograms. In one patient, who presented with symptomatic mass effect of the aneurysm on the brain stem, a significant size reduction was achieved in the patent lumen of the aneurysm, but complete occlusion did not occur even at the 2-year control angiogram. The remaining sac was coiled without any evidence of mass effect. In the other patient with a giant basilar tip aneurysm, reduction in size and mass effect was observed at the 3-month control; however, there was still residual filling. All stents but one remained patent with no in-stent stenosis. In only one patient with a basilar bifurcation aneurysm, the right P1 was found to be occluded in association with complete thrombosis of the aneurysm in the control. The distal PCA was filling via PcomA in this patient, and he remained asymptomatic.
Double stent placement in Y-configuration was performed by using a closed-cell design stent (Enterprise) in all cases without any technical difficulties. This stent addressed the problem of intracranial navigation because it can be advanced through standard microcatheters. In all previously reported series on Y-stent–assisted embolization technique, an open-cell-design stent was used,13–15 and it was thought that the wide interstices of this stent make it unlikely that stent alone would precipitate aneurysm thrombosis.13 The Enterprise stent was preferred in this series not only because of its ease of delivery and deployment but also because it seemed more likely to provide superior modification on aneurysm hemodynamic parameters with its narrower interstices and higher radial force. Moreover, one may argue that inevitable oversizing (because Enterprise stents do not have smaller sizes than 4.5 mm) also may have an additive role in the amount of flow diversion achieved. Angiograms obtained after deployment of the second stent demonstrated hemodynamic effects of the technique, such as diminished contrast filling and stagnation within the aneurysm sac, that were more notable in the larger aneurysms.
We feel that the impact of this technique would be important in endovascular treatment of bifurcation aneurysms with a very wide neck or with no definable neck, large or giant aneurysms with mass effect, and those too small to be packed. The major current concern is the small size of the parent vessel relative to the diameter of the smallest available stent.
Conclusions
Our preliminary experience shows that Y-stent flow diversion technique is a feasible, secure, and effective option for the endovascular treatment of complex bifurcation aneurysms. A larger series with longer follow-up is required to assess the long-term durability and safety; however, the technical and clinical results achieved were highly encouraging, and we believe that this technique may contribute to the endovascular treatment of these complex bifurcation aneurysms.
Abbreviations
- CTA
CT angiography
- DSA
digital subtraction angiography
- ICA
internal carotid artery
- MCA
middle cerebral artery
- PCA
posterior cerebral artery
- PcomA
posterior communicating artery
- R
ruptured
- SAH
subarachnoid hemorrhage
- SCA
superior cerebellar artery
- U
unruptured
- VA
vertebral artery
Footnotes
Disclosures: S.G., research support (including provision of equipment or materials): Microvention; consultant: eV3. I.S., consultant: eV3.
References
- 1. Fiorella D, Albuquerque FC, Deshmukh VR, et al. Usefulness of the Neuroform stent for the treatment of cerebral aneurysms: results at initial (3–6 mo) follow-up. Neurosurgery 2005;56:1191–202 [DOI] [PubMed] [Google Scholar]
- 2. Lylyk P, Ferrario A, Pabon B, et al. Buenos Aires experience with the Neuroform self-expanding stent for the treatment of intracranial aneurysms. J Neurosurg 2005;102:235–41 [DOI] [PubMed] [Google Scholar]
- 3. Lubicz B, Leclerc X, Levivier M, et al. Retractable self-expandable stent for endovascular treatment of wide-necked intracranial aneurysms: preliminary experience. Neurosurgery 2006;58:451–57 [DOI] [PubMed] [Google Scholar]
- 4. Pumar JM, Blanco M, Vazquez F, et al. Preliminary experience with LEO self-expanding stent for the treatment of intracranial aneurysms. AJNR Am J Neuroradiol 2005;26:2573–77 [PMC free article] [PubMed] [Google Scholar]
- 5. Higashida RT, Halbach VV, Dowd CF, et al. Initial clinical experience with a new self-expanding nitinol stent for the treatment of intracranial cerebral aneurysms: the Cordis Enterprise stent. AJNR Am J Neuroradiol 2005;26:1751–56 [PMC free article] [PubMed] [Google Scholar]
- 6. Weber W, Bendszus M, Kis B, et al. A new self-expanding nitinol stent (Enterprise) for the treatment of wide-necked intracranial aneurysms: initial clinical and angiographic results in 31 aneurysms. Neuroradiology 2007;49:555–61 [DOI] [PubMed] [Google Scholar]
- 7. Liebig T, Henkes H, Reinartz J, et al. A novel self-expanding fully retrievable intracranial stent (SOLO): experience in nine procedures of stent-assisted aneurysm coil occlusion. Neuroradiology 2006;48:471–78 [DOI] [PubMed] [Google Scholar]
- 8. Yavuz K, Geyik S, Pamuk AG, et al. Immediate and midterm follow-up results of using an electrodetachable, fully retrievable SOLO stent system in the endovascular coil occlusion of wide-necked cerebral aneurysms. J Neurosurg 2007;107:49–55 [DOI] [PubMed] [Google Scholar]
- 9. Yavuz K, Geyik S, Saatci I, et al. WingSpan stent system in the endovascular treatment of intracranial aneurysms: clinical experience with midterm follow-up results. J Neurosurg 2008;109:445–53 [DOI] [PubMed] [Google Scholar]
- 10. Zenteno MA, Santos-Franco JA, Freitas-Modenesi JM, et al. Use of the sole stenting technique for the management of aneurysms in the posterior circulation in a prospective series of 20 patients. J Neurosurg 2008;1104–18 [DOI] [PubMed] [Google Scholar]
- 11. Pumar JM, Lete I, Pardo MI, et al. LEO stent monotherapy for the endovascular reconstruction of fusiform aneurysms of the middle cerebral artery. AJNR Am J Neuroradiol 2008;29:1775–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chow MM, Woo HH, Masaryk TJ, et al. A novel endovascular treatment of a wide-necked basilar apex aneurysm by using a Y-configuration, double-stent technique. AJNR Am J Neuroradiol 2004;25:509–12 [PMC free article] [PubMed] [Google Scholar]
- 13. Thorell WE, Chow MM, Woo HH, et al. Y-configured dual intracranial stent-assisted coil embolization for the treatment of wide-necked basilar tip aneurysms. Neurosurgery 2005;56:1035–40 [PubMed] [Google Scholar]
- 14. Sani S, Lopes DK. Treatment of a middle cerebral artery bifurcation aneurysm using a double Neuroform stent “Y” configuration and coil embolization: technical case report. Neurosurgery 2005;57:E209. [DOI] [PubMed] [Google Scholar]
- 15. Lozen A, Manjila S, Rhiew R, et al. Y-stent-assisted coil embolization for the management of unruptured cerebral aneurysms: report of six cases. Acta Neurochir 2009;151:1663–72 [DOI] [PubMed] [Google Scholar]
- 16. Canton G, Levy DI, Lasheras JC. Hemodynamic changes due to stent placement in bifurcating intracranial aneurysms. J Neurosurg 2005;103:146–55 [DOI] [PubMed] [Google Scholar]
- 17. Saatci I, Geyik S, Yavuz K, et al. X-configured stent-assisted coiling in the endovascular treatment of complex anterior communicating artery aneurysms: a novel reconstructive technique. AJNR Am J Neuroradiol 2011;32:E113–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Doerfler A, Wanke I, Egelhof T. Double-stent method: therapeutic alternative for small wide-necked aneurysms. Technical note. J Neurosurg 2004;100:150–54 [DOI] [PubMed] [Google Scholar]
- 19. Rhee K, Han MH, Cha SH. Changes of flow characteristics by stenting in aneurysm models: influence of aneurysm geometry and stent porosity. Ann Biomed Eng 2002;30:894–904 [DOI] [PubMed] [Google Scholar]
- 20. Vanninen R, Manninen H, Ronkainen A. Broad-based intracranial aneurysms: thrombosis induced by stent placement. AJNR Am J Neuradiol 2003;24:263–66 [PMC free article] [PubMed] [Google Scholar]
- 21. Kim M, Levy EI, Meng H, et al. Quantification of hemodynamic changes induced by virtual placement of multiple stents across a wide-necked basilar trunk aneurysm. Neurosurgery 2007;61:1305–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Crowley RW, Evans AJ, Kassell NF, et al. Endovascular treatment of a fusiform basilar artery aneurysm using multiple “in-stent stents”. J Neurosurg Pediatrics 2009;3:496–500 [DOI] [PubMed] [Google Scholar]
- 23. Fiorella D, Woo HH, Albuquerque FC, et al. Definitive reconstruction of circumferential, fusiform intracranial aneurysms with the Pipeline embolizatiion device. Neurosurgery 2008;62:1115–21 [DOI] [PubMed] [Google Scholar]
- 24. Lylyk P, Miranda C, Ceratto R, et al. Curative endovascular reconstruction of cerebral aneurysms with the Pipeline embolization device: the Buenos Aires experience. Neurosurgery 2009;64:632–43 [DOI] [PubMed] [Google Scholar]