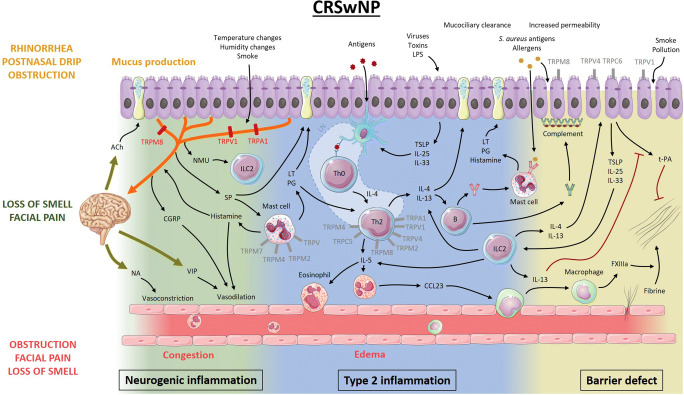
Fig. 2.
Proposed model of the pathophysiology of chronic rhinosinusitis with nasal polyps and the potential role of TRP channels. Antigens presented by dendritic cells initiate development of Th2 cells that release IL-4, IL-5, and IL-13. IL-5 recruits and activates eosinophils, which ultimately leads to fibrin cross-linking and polyp formation. IL-4 and IL-13 stimulate B cells to produce not only monoclonal IgE to Staphylococcus aureus antigens but also polyclonal autoantibodies leading to complement activation at the basement membrane of the epithelium. Together with protease activity from allergens, environmental factors, and inflammatory mediators, this leads to disruption of the epithelial barrier, facilitating penetration of environmental stimuli. Activated epithelial cells release pro-inflammatory mediators, which can activate dendritic cells and type 2 innate lymphoid cells. Much like in AR, the nervous system participates in the inflammatory process through neuro-immune interactions, modulating the immunological battlefield. Type 2 inflammatory mediators can activate and potentially sensitize sensory afferent neurons, while neuropeptides can activate mast cells and type 2 innate lymphoid cells (ILC2). Moreover, central reflexes regulate vascular tone and mucosal gland activity. The role of TRPV1, TRPA1, and TRPM8 in neurogenic inflammation has been studied the most. However, TRP channels present on other cells could be potential therapeutic targets as well (gray). Ach, acetylcholine; NA, noradrenaline; VIP, vasoactive intestinal peptide; CGRP, calcitonin gene-related peptide; NMU, neuromedin U; SP, substance P; ILC2, type 2 innate lymphoid cell; PG, prostaglandins; LT, leukotrienes; LN, lymph node; IL, interleukin; LPS, lipopolysaccharide; TSLP, thymic stromal lymphopoietin; CCL23, chemokine (C-C motif) ligand 23; FXIIIa, activated coagulation factor 13; t-PA, tissue plasminogen activator