Abstract
Summary: A 13-year-old boy presented with an arteriovenous malformation (AVM) involving the left mandible that bled after intraoral biopsy. The AVM was treated on an emergency basis by primary intravenous delivery of n-butyl cyanoacrylate after transfemoral catheterization, resulting in complete anatomic and clinical cure.
Because patients with arteriovenous malformations (AVMs) of the mandible may present with a life-threatening hemorrhage (1–4), endovascular treatment often has to be performed on an emergency basis and is considered technically challenging (1). Transvenous embolization has been advocated either by direct transosseous venous puncture for delivery of various embolic agents, including glue (1, 5, 6), or by transfemoral catheterization and packing of coils (3, 7, 8). We report a child with a mandibular AVM that was successfully treated by primary intravenous delivery of n-butyl cyanoacrylate (NBCA) after transfemoral catheterization, resulting in complete anatomic and clinical cure. To our knowledge, this particular technique has not been described for endovascular management of a mandibular AVM.
Case Report
A 13-year-old boy was referred to our hospital for biopsy of a lytic lesion within the left mandible. The patient presented with numbness of the left lower lip but had no history of bleeding. During biopsy, minor bleeding occurred, which was easily brought under control by pressure packing. The patient was immediately transferred to the angiosuite to rule out a vascular lesion. Digital subtraction angiography revealed an AVM of the left mandible with an enlarged mandibular vein (Fig 1A and B). The AVM was fed partially by small branches of the ipsilateral facial artery, but primarily by the inferior dental artery arising from the internal maxillary artery. For endovascular treatment, the left external carotid artery was catheterized with a 5F guiding catheter (Envoy, Cordis Endovascular, Miami Lakes, FL), and a microcatheter was navigated into the facial artery. Particulate embolization was performed first to reduce the shunt volume using polyvinyl alcohol particles (250–350 μm). To position the microcatheter, the inferior dental artery was selectively catheterized at the most distal end of the feeder. From a wedged position, glue (30% NBCA; Histoacryl, B. Braun Melsungen AB, Melsungen, Germany) mixed with iodized oil (Lipiodol, Byk Gulden, Konstanz, Germany) was injected, resulting in a further decrease of the arteriovenous shunting flow, but not in complete occlusion. Therefore, in the same session, the retromandibular vein was catheterized by a transfemoral approach with a 6F guiding catheter, and a microcatheter was then navigated toward the fistula site within the lower mandible (Fig 1C).
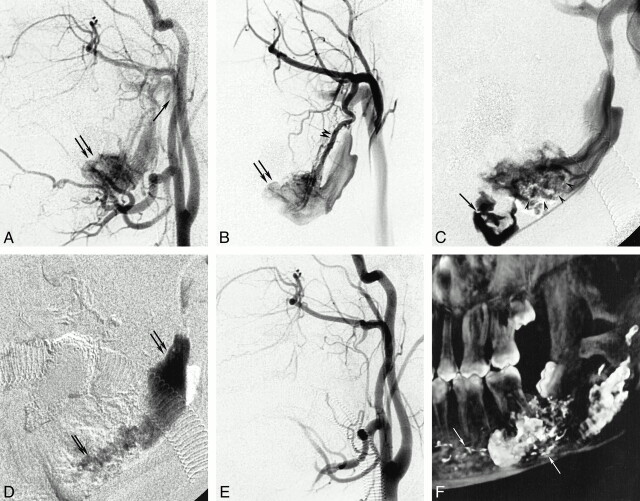
fig 1.
13-year-old boy with an AVM involving the left mandible that bled after intraoral biopsy.
A and B, Initial arteriograms.
A, Left common carotid arteriogram, lateral view, shows opacification of an arteriovenous shunting lesion with early filling of a large venous varix (double arrow) of the left mandibular vein draining into the retromandibular vein (single arrow).
B, Left internal maxillary arteriogram, lateral view, shows the venous varix (arrows) is better filled and supplied mainly by the inferior dental artery (arrowheads), revealing the intraosseous location.
C–F, Studies after embolization.
C, Left mandibular phlebogram shows the tip of the microcatheter navigated into the very proximal part of the vein (arrow). The glue (arrowheads), already delivered by transarterial embolization, only partially occludes the mandibular vein.
D, Roadmap image shows the glue cast (arrows) after the third intravenous injection filling the entire mandibular vein.
E, Left common carotid arteriogram shows complete occlusion of the AVM by the end of the procedure.
F, 3D reconstruction of the left mandible (rotational digital subtraction angiogram) shows the radiopaque embolic agent within the osseous cavity. The glue is positioned in the proximal and distal vein as well as in some of the small feeding vessels (arrows).
During intravenous glue injection, manual compression of the retromandibular vein was performed to block the intravenous flow and prevent distal migration of the liquid adhesive. Furthermore, to avoid gluing of the catheter, the following technique was applied: a 50% NBCA/Lipiodol mixture was injected by pushing it through a 5-mL syringe, stopping after 1 to 2 mL had been injected, thereby creating a kind of bubble. After a few seconds of polymerization, the microcatheter was briefly pulled back 1 to 2 cm to remove the tip of the catheter from the initial glue cast, and then followed by the next injection until another cast of glue had been instilled. This procedure was repeated three times with two microcatheters until the mandibular vein was filled with a total of 5 mL of glue (Fig 1D and F).
When removing the microcatheter, the guiding catheter was positioned as close as possible to the mandibular vein. The external carotid arteriogram showed complete disappearance of the fistula by the end of the procedure, with no remaining filling of the mandibular vein (Fig 1E), such that no additional transarterial embolization was necessary. No bleeding occurred during or after the procedure. The patient received steroids and prophylactic antibiotic treatment for 5 days, made a full recovery, and was discharged after 8 days. A follow-up arteriogram after 10 weeks confirmed the stable result with complete occlusion of the arteriovenous shunt.
Discussion
AVMs of the dental arcade are rare lesions occurring predominantly in childhood. Most patients present with minor bleeding episodes that ensue while brushing the teeth; some present with life-threatening hemorrhages after tooth extraction or biopsy (1–4). Other symptoms include bruit, dental loosening, swelling of the soft tissues of the face, change in skin and mucosal color, and dysesthesia of the lower lip or chin due to sensorial fifth nerve irritation (1, 9, 10). Therapeutic management of these lesions may be difficult, because most patients present in an emergency setting and the complex vascular architecture (ie, the recruitment of numerous feeding vessels from the ipsi- and contralateral facial, lingual, and maxillary arteries) complicates surgical as well as endovascular treatment.
Surgical resection after partial embolization may be safe, because it can be complete (8, 11), but because it may be associated with significant loss of blood and often produces mutilating alterations in the still-growing face, it is not recommended as the treatment of choice (1, 8). Transarterial particulate embolization usually does not result in complete occlusion, and recurrence and rehemorrhage are frequent complications (1, 5). Transarterial glue embolization is more effective and complete (1), but sometimes remains incomplete if it is not possible to place the catheter distally or to obtain sufficient filling of the mandibular vein (8). Therefore, direct puncture through the bone for direct access to the venous pouch has been proposed by some authors (1, 5, 6, 8). This approach allows placement of a microcatheter into the proximal venous drainage and delivery of a sufficient amount of embolic material. Complete and permanent occlusion of the AVM is possible and has also been successfully carried out by our group. Chiras et al (8) reported successful occlusion using a combination of detachable balloons and pieces of gelatin sponge after direct puncture of the venous pouch. However, because the aggressive transosseous approach requires technical experience to be performed successfully, it might not always be the treatment of choice, particularly in pediatric emergency care. Transfemoral venous catheterization of mandibular AVMs has been successfully performed in individual cases by Kiyosue et al (3) and Beek et al (7). Both groups achieved significant reduction of the arteriovenous shunting flow and recommended transvenous coil packing as a safe and possibly more effective treatment than transarterial glue deposition. In our opinion, this technique represents a valuable alternative, but, owing to the often remarkably enlarged vein, more coils are needed for effective reduction of the shunt or complete closure (3). In addition, the procedure can be rather expensive and, more important in a life-threatening situation, time-consuming. Finally, in the event the vein is not packed densely enough, repeat transarterial or transvenous embolization may become necessary, as described before by Kiyosue et al (3) and Beek et al (7).
With the exception of direct transosseous puncture, intravenous injection of NBCA has not been the preferred method for treatment of mandible AVMs. Two major technical problems may be associated with this approach:
1) Gluing of the catheter. This is not a major problem during direct transosseous puncture, because leaving the needle in place allows good control while the catheter is being pulled back. We experienced one incident in which the catheter was accidentally severed after direct puncture of the maxilla, leaving a short (2-cm) piece of catheter within the vein. However, this did not create any clinical problems, such as foreign body reaction, for the patient. During transfemoral venous glue injection, the conditions are slightly different, but the technique we applied here was very helpful. Graduated retraction, allowing several glue injections through the same catheter, was possible in this case because the arterial inflow had already been reduced by previous transarterial embolization. In addition, the large diameter of the venous pouch further lowered the intravenous flow velocity. Given this hemodynamic condition, the direct intravenous injection of a 50% NBCA/Lipiodol mixture was considered feasible and safe.
2) Distal migration of the glue toward the pulmonary circulation. To minimize this risk, the 6F guiding catheter was placed close to the exit of the mandibular vein, which also contributed to reduction of the shunt flow. This catheter could also easily be palpated subcutaneously, thus facilitating manual compression of the vein. The efficacy of manual compression of draining veins during glue embolization has been clearly demonstrated by several authors, including our group, and is particularly feasible if the malformation is located superficially (eg, in the soft tissue of the head and neck) (9, 12).
In the case described here, the arteriovenous shunting flow was significantly reduced by transarterial embolization at the beginning of the procedure with only minimal opacification of the draining vein shown in the control angiogram. Nevertheless, the phlebogram clearly showed how misleading these images can be: the mandibular vein was still wide open, representing a trigger for future recruitment of new feeders and recurrence of the AVM. In our experience, complete occlusion of this vein is the only guarantee for complete long-term cure. As stressed by Beek et al (7), primary transvenous embolization carries the risk of a sudden increase of intravenous pressure with subsequent rupture and bleeding if the occlusion remains incomplete. Therefore, reduction of the arterial inflow by transarterial embolization at the beginning of the procedure is strongly recommended (9).
Conclusion
Primary transfemoral venous glue embolization is a simple and safe technique for endovascular management of mandibular AVMs and is particularly feasible in an emergency. The venous varix inside the mandibular bone can be reached with standard catheter techniques and permanently occluded by controlled delivery of the embolic agent. We suggest this feasible, inexpensive, and effective technique as a valuable alternative in the treatment of mandibular AVMs, especially for emergency management of this potentially life-threatening vascular disorder.
Footnotes
Address reprint requests to Goetz Benndorf, MD, Neuroangiography, Department of Radiology, Virchow Hospital, Charité, Humboldt University Berlin, Augustenburger PL. 1, 13353 Berlin, Germany.
Referecnes
- 1.Rodesch G, Soupre V, Vazquez MP, Alvarez H, Lasjaunias P. Arteriovenous malformations of the dental arcades: the place of endovascular therapy: results in 12 cases are presented. J Craniomaxillofac Surg 1998;26:306-313 [DOI] [PubMed] [Google Scholar]
- 2.Engel JD, Supancic JS, Davis LF. Arteriovenous malformation of the mandible: life-threatening complications during tooth extraction [see comments]. J Am Dent Assoc 1995;126:237-242 [DOI] [PubMed] [Google Scholar]
- 3.Kiyosue H, Mori H, Hori Y, Okahara M, Kawano K, Mizuki H. Treatment of mandibular arteriovenous malformation by transvenous embolization: a case report. Head Neck 1999;21:574-577 [DOI] [PubMed] [Google Scholar]
- 4.Lamberg MA, Tasanen A, Jaaskelainen J. Fatality from central hemangioma of the mandible. J Oral Surg 1979;37:578-584 [PubMed] [Google Scholar]
- 5.Resnick SA, Russell EJ, Hanson DH, Pecaro BC. Embolization of a life-threatening mandibular vascular malformation by direct percutaneous transmandibular puncture. Head Neck 1992;14:372-379 [DOI] [PubMed] [Google Scholar]
- 6.Flandroy P, Pruvo JP. Treatment of mandibular arteriovenous malformations by direct transosseous puncture: report of two cases. Cardiovasc Intervent Radiol 1994;17:222-225 [DOI] [PubMed] [Google Scholar]
- 7.Beek FJ, ten Broek FW, van Schaik JP, Mali WP. Transvenous embolisation of an arteriovenous malformation of the mandible via a femoral approach. Pediatr Radiol 1997;27:855-857 [DOI] [PubMed] [Google Scholar]
- 8.Chiras J, Hassine D, Goudot P, Meder JF, Guilbert JF, Bories J. Treatment of arteriovenous malformations of the mandible by arterial and venous embolization. AJNR Am J Neuroradiol 1990;11:1191-1194 [PMC free article] [PubMed] [Google Scholar]
- 9.Han MH, Seong SO, Kim HD, Chang KH, Yeon KM, Han MC. Craniofacial arteriovenous malformation: preoperative embolization with direct puncture and injection of n-butyl cyanoacrylate. Radiology 1999;211:661-666 [DOI] [PubMed] [Google Scholar]
- 10.Mohammadi H, Said-al-Naief NA, Heffez LB. Arteriovenous malformation of the mandible: report of a case with a note on the differential diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997;84:286-289 [DOI] [PubMed] [Google Scholar]
- 11.Fathi M, Manafi A, Ghenaati H, Mohebbi H. Large arteriovenous high-flow mandibular, malformation with exsanguinating dental socket haemorrhage: a case report. J Craniomaxillofac Surg 1997;25:228-231 [DOI] [PubMed] [Google Scholar]
- 12.Benndorf G, Lehmann TN, Lanksch WR. Treatment of external carotid artery fistula by percutaneous venous approach. Intervent Neuroradiol 1999;5:251-256 [DOI] [PubMed] [Google Scholar]