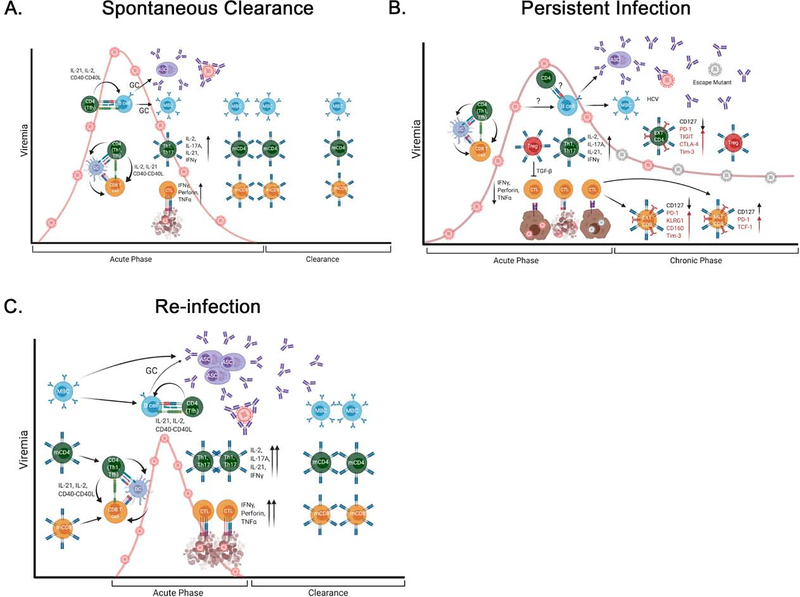
Figure 2. Adaptive immune responses in spontaneous clearance, persistence, and re-infection of HCV.
(A) Spontaneous clearance: during acute HCV infection (0–6 months), CD4+ T cells (Th1 and Tfh cells) activate HCV-specific CD8+ T and B cells indirectly (via DCs) or directly (via interactions between CD40 and CD40L). Activated CD8+ T cells and B cells enter germinal centers, where they proliferate and differentiate into effector T cells with cytotoxic function or antibody-secreting cells (ASCs), respectively. Cytolytic T cells (CTLs) kill infected hepatocytes, whereas Th1 and Th17 cells release cytokines that promote localized inflammation and potentiate the activities of CTLs. ASCs release antibodies that neutralize autologous HCV. (B) Persistence: activation of B cells and CD8+ T cells by CD4+ T cells (Th1 and Tfh cells) is limited. Treg cells reduce the activity of CTLs, and mutant viruses escape antibody neutralization and killing by T cells. As viremia persists, constant expression of inhibitory molecules (red) results in T-cell exhaustion (EXT), but some CD8+ T cells acquire a memory-like phenotype (TCF1+PD-1+). (C) Re-infection: existing memory CD4+ and CD8+ T cells and memory B cells (MBCs) are rapidly activated and proliferate upon re-exposure to HCV. Activated, HCV-specific T and B cells can undergo further rounds of affinity maturation in germinal centers and/or rapidly differentiate into effector T cells or ASCs, respectively. Cytotoxic activity and nAbs are increased during secondary HCV infection, leading to faster clearance and expansion of memory T and B cells. (GC = germinal center; mCD4+ = memory CD4+ + T cell; mCD8+ = memory CD8+ + T cell; MTL CD8+ = memory-like CD8+ T cell).