Abstract
Objectives
The Coronavirus 2019 (COVID-19) pandemic caused a considerable mortality in long-term care facilities (LTCFs), including residential care setting and nursing homes. This study aimed to estimate COVID-19 incidence and mortality in residential care facilities and to compare them with those recorded in nursing homes.
Design
Nationwide observational study conducted by French health authorities.
Settings and participants
Since March 1, 2020, all LTCFs in France reported all COVID-19 cases and COVID-19–related deaths among their residents.
Methods
Possible cases were those with COVID-19–related symptoms without laboratory confirmation and confirmed cases those with a reverse transcriptase polymerase chain reaction test or serology positive for SARS-CoV-2. We included facilities with at least 1 confirmed case of COVID-19 and estimated the cumulative incidence of COVID-19 cases and mortality due to COVID-19 reported until June 30, 2020, using the maximum bed capacity as a denominator.
Results
Of the 2288 residential care facilities, 310 (14%) and, of the 7688 nursing homes, 3110 (40%) reported COVID-19 cases among residents (P < .001). The cumulative incidence of COVID-19 was significantly lower in residential care facilities as compared with nursing homes (1.10 vs 9.97 per 100 beds, P < .001). Mortality due to COVID-19 was also lower in residential care facilities compared with nursing homes (0.07 vs 1.29 per 100 beds, P < .001). Case fatality was lower in residential care facilities (6.49% vs 12.93%, P < .001).
Conclusion and implications
French residential care facilities experienced a much lower burden from COVID-19 than nursing homes. Our findings may inform the implementation of better infection control practices in these settings.
Keywords: Long-term care facilities, residential care, nursing homes, COVID-19, mortality, case-fatality ratio
The Coronavirus 2019 (COVID-19) pandemic had dramatic consequences for older people.1, 2, 3 Age was the main factor associated with COVID-19–related mortality, with the mortality rate being 60 times higher in people aged ≥80 years than in adults <50 years.4 Several studies have reported on the burden of COVID-19 in long-term care facilities (LTCFs), with large outbreaks and high mortality rates.5, 6, 7, 8, 9 A recent study reported that COVID-19–related deaths in LTCF accounted for 30%-60% of all COVID-19 deaths in many European countries.10
Residential care settings, also named assisted living facilities (Résidences autonomie in France), are a type of LTCF for older people that has some special features compared with nursing homes. These facilities offer their residents an independent private accommodation, including a kitchen, bathroom, television and telephone connections, the provision and maintenance of common areas, access to a restaurant service, laundry service, access to 24-hour security assistance, access to group events or outdoor activities organized by the residence.11 Community services operating in their district take care of the residents who require assistance for dependency or medical care. Nursing homes, on the other hand, provide residents with rooms in group housing with meals served in collective dining rooms and a wide variety of care and services, including assistance for activities of daily living and nursing care.
Many studies have described the consequences of COVID-19 infection in long-term care residents.8 , 12, 13, 14 However, apart from media reports, there have not been published studies reporting the occurrence of COVID-19 in residential care facilities, although those account for about one-fifth of the LTCF in France,15 , 16 and their number is similar to that of nursing homes in the United States.17
We aimed to determine whether these facilities were affected by the COVID-19 pandemic at the same extent as nursing homes.
Methods
Study Design
On March 28, 2020, following reports of COVID-19–related deaths in nursing homes, Santé Publique France, the French national public agency established a surveillance system to monitor the number of COVID-19 cases and deaths reported in LTCFs. As of March 1, 2020, all LTCFs reported daily cases of COVID-19 occurring among their residents and COVID-19–related deaths occurring in the facility or the hospital. According to French health care authorities, COVID-19 confirmed cases were those with a reverse transcriptase polymerase chain reaction (RT-PCR) test or those with COVID-19 clinical infection (acute respiratory infection with cough, fever or dyspnea, abrupt onset of asthenia, myalgia, anosmia or hyposmia, and ageusia or dysgeusia unexplained by other diseases) and serology positive for SARS-CoV-2; possible cases were defined as those with COVID-19 clinical infection but without laboratory confirmation. We included possible cases only from facilities with at least 1 confirmed case, indicating introduction and circulation of the virus. We extracted those data on June 30, 2020, and merged them with the national database of health care facilities (FINESS).
Outcomes
We estimated the proportion of facilities with at least 1 confirmed case of COVID-19. We also calculated the cumulative incidence of COVID-19 cases and mortality due to COVID-19 declared between March 1 and June 30, 2020, using the maximum bed capacity of the facility as denominator, because we did not have access to the exact occupancy rate of the facilities during this period. Because the pandemic severity varied across French regions, we stratified the analysis by the regional level of COVID-19 cumulative incidence. We defined 3 types of regions, based on the regional incidence of COVID-19 in LTCFs: high incidence (>9% of residents), intermediate incidence (3%-9% of residents), low incidence (<3% of residents).
Statistical Analysis
We compared the proportions or incidence rates between residential care settings and nursing homes using chi-square test and Fisher exact test, or analysis of variance. We calculated rate ratios (RRs) and 95% confidence intervals (CIs) using Poisson regression. P values of <.05 were considered as significant. We used Stata16 software (StataCorp, College Station, TX, USA) to perform the analysis.
Results
Among the 9976 LTCFs recorded in the national database, there were 2288 residential facilities and 7688 nursing homes. Of those, 310 (14%) residential care facilities and 3110 (40%) nursing homes reported at least 1 confirmed COVID-19 case among their residents (P < .001) (Table 1 ). Three regions were classified as high incidence (Grand-Est, Hauts-de-France, Ile-de-France), 6 regions were classified as low incidence (Bretagne, Corse, Normandie, Nouvelle Aquitaine, Occitanie, Pays de Loire) and the 4 remaining regions were classified as intermediate incidence (Auvergne-Rhone-Alpes, Bourgogne-Franche Comté, Centre-Val de Loire, Provence Côte d’Azur). The risk of having at least 1 confirmed case in a residential care facility was 67% (RR 0.33, 95% CI 0.30-0.37) lower than in a nursing home. The same pattern was observed when we stratified by level of regional incidence (Table 1).
Table 1.
Number of LTCFs With at Least 1 Confirmed Case of COVID-19 Among Their Residents, by Type of Facility and Regional Level of COVID-19 Incidence, and the RR (95% CI) for Having at Least 1 Confirmed Case of COVID-19 in the Residential Care Facilities Compared With Nursing Homes, France, March 1, 2020, to June 30, 2020
| All Facilities, n (%) (N = 9976) |
Residential Care, n (%) (n = 2288) |
Nursing Homes, n (%) (n = 7688) |
RR (95% CI) | P Value | |
|---|---|---|---|---|---|
| Overall | 3419 (34) | 310 (14) | 3110 (40) | 0.33 (0.30-0.37) | <.001 |
| Regional level of COVID-19 incidence | |||||
| Low incidence (n = 4212) | 901 (21) | 50 (5.8) | 851 (25) | 0.23 (0.18-0.30) | <.001 |
| Intermediate incidence (n = 2941) | 977 (33) | 53 (9.2) | 924 (39) | 0.23 (0.18-0.30) | <.001 |
| High incidence (n = 2823) | 1541 (55) | 206 (24) | 1335 (68) | 0.36 (0.31-0.40) | <.001 |
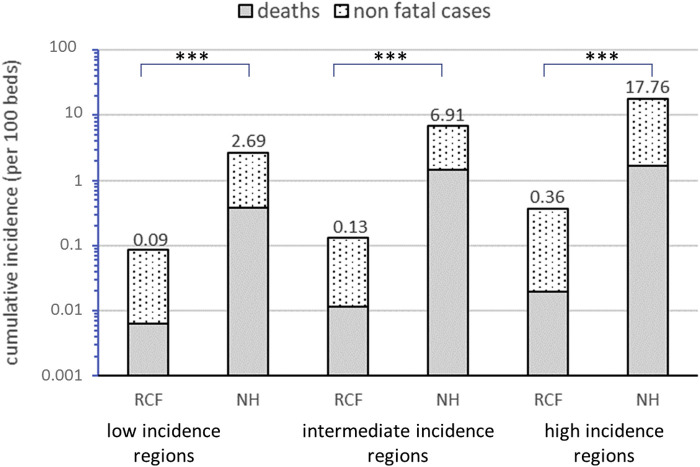
The cumulative incidence rate of COVID-19 was 89% (RR 0.11, 95% CI 0.09-0.13) lower in residential care facilities compared with that of nursing homes (1.10 vs 9.97 per 100 beds, P < .001) (Table 2 ). The differences were significant for confirmed or possible cases of COVID-19. The lower incidence rate of COVID-19 in residential care facilities was observed at all 3 regional levels of COVID-19 incidence (Figure 1 ). COVID-19–related mortality was 95% (RR 0.05, 95% CI 0.04-0.08) lower in residential care facilities compared with that in nursing homes (0.07 vs 1.29 per 100 beds, P < .001). Case fatality was 51% (RR 0.49, 95% CI 0.34-0.68) lower in residential care facilities than in nursing homes (6.49% vs 12.93%, P < .001).
Table 2.
Number of COVID-19 Cases and Deaths, Cumulative Incidence, and Mortality Rates (per 100-Bed Capacity) in French LTCFs by Type of Facility, and RR (95% CI) in Residential Care Facilities Compared With Nursing Homes, France, March 1, 2020, to June 30, 2020
| All Facilities, n∗ (Rate per 100 Beds) (N = 736,038) |
Residential Care Homes, n∗ (Rate per 100 Beds) (n = 120,921) |
Nursing Homes, n∗ (Rate per 100 Beds) (n = 615,117) |
RR (95% CI) | P Value | |
|---|---|---|---|---|---|
| Confirmed cases | 33,426 (4.54) | 744 (0.62) | 32,682 (5.31) | 0.11 (0.10-0.16) | <.001 |
| Possible cases | 29,203 (3.97) | 581 (0.48) | 28,622 (4.65) | 0.10 (0.09-0.12) | <.001 |
| Total cases | 62,629 (8.51) | 1325 (1.10) | 61,304 (9.97) | 0.11 (0.09-0.13) | <.001 |
| COVID-19 deaths | 8011 (1.09) | 86 (0.07) | 7925 (1.29) | 0.05 (0.04-0.08) | <.001 |
Number of cases or deaths.
Fig. 1.
Cumulative incidence of nonfatal and fatal cases of COVID-19 among the residents of French long-term care facilities, by type of facility and regional level of COVID-19 incidence. The differences in incidence between residential care facilities (RCFs) and nursing homes (NHs) were significant in each type of regions.
Discussion
This study indicated that the burden of COVID-19 during the first wave of the pandemic in France was much lower in residents of residential care facilities than those of nursing homes. This could be related to several factors, including differences in living conditions, staff exposure, and general health status of those populations. Testing practices did not differ in the different types of settings during the study period.
One factor that could explain the lower occurrence of COVID-19 in residential care facilities is the smaller number of contacts among the residents and between residents and staff members compared with those observed in nursing homes. In France, residents of residential care facilities are provided with a private housing, including a kitchen, and many of them can easily take their meals in their own premises and using meals-on-wheels services. In contrast, residents in nursing homes do not have these options and eat their meals in dining rooms where interactions with other residents and staff are numerous. In addition, the number of staff members in nursing homes is higher than in residential care facilities. Staff members may be responsible for the transmission of SARS-CoV-2 to the residents as they move back and forth between the facility and the community.9 In France, the staff ratio is about 64 per 100 beds in nursing homes compared with 13 per 100 beds in independent living residences.16 Even if the residents of residential care facilities who are dependent for daily living activities or who require medical care meet additional home-aid staff and health care professionals from the community, they probably still interact with a smaller number of professionals than nursing home residents. Furthermore, in France, special care units for people with dementia and severe behavioral disorders are included in nursing homes, but not in residential care facilities, with the prevalence of dementia being much higher in nursing homes. Patients with dementia are less likely to adopt protective measures leading to increased transmission of COVID-19 in those units. However, from mid-March to early June 2020, French health authorities requested that nursing home residents stay confined in their room and banned visits of their relatives. That has probably reduced the number of contacts between nursing home residents and reduced the differences between residential care and nursing home facilities for this aspect.
In our study, the case-fatality for COVID-19 among residents of residential care facilities was half that observed in nursing homes. This is likely related to some differences in the profile of residents in residential care facilities. Residents in residential care facilities are generally healthier than the nursing home population, with the prevalence of comorbidities being higher among the first.16 According to a French Ministry of Health survey conducted in 2005, the average age of residents was 83 years in residential care facilities and 86 years in nursing homes.16 In the same survey, severe dependence for activities of daily living, defined by Groupe Iso-Ressources (GIR) 1 or 2, was recorded in 54% of residents in nursing homes and in only 1.3% of residents in residential care facilities, and the corresponding values for mild or no dependence (GIR 5 or 6) were 8.6% and 64%, respectively.16 This indicates that residents in residential care facilities are on average younger and less disabled than nursing home residents, and that may explain the lower fatality observed in the former. In addition, because of the high prevalence of disability and severe chronic illness, including dementia, many nursing home residents are not eligible for transfer to an intensive care unit to be cared for with mechanical ventilation, and the proportion of ineligible patients is probably higher than in residential care facilities. This could also contribute to differences in death rates.
It should be noted that the definition of COVID-19 confirmed cases18 , 19 used in our study differs somewhat from the definition given by the World Health Organization20 and the Centers for Disease and Prevention Control,21 according to which a positive RT-PCR test for CoV2-SARS is the only confirmatory laboratory element. When defining the confirmed cases of COVID-19, the French health authorities accepted a positive serology for CoV2-SARS as the confirmatory laboratory element for cases with clinical symptoms of COVID-19 and a negative RT-PCR test or if RT-PCR was not performed.19 This may influence the balance between confirmed and possible cases and should be taken into account when comparing the incidence rate of confirmed cases observed in our study with that of other studies. However, same case definition was applied to residential care facilities and nursing homes, so this cannot explain the differences in incidence rates observed.
Our study had several limitations. First, we cannot exclude that cases of COVID-19 may have been underdiagnosed and also under-reported in residential care facilities despite the request of health care authorities. This is very unlikely because of the daily on-site presence of staff in these facilities and their high level of awareness to the risk of COVID-19 among the residents. Moreover, access to medical and laboratory care is very easy in these facilities, similar to nursing homes. Second, in this study, we estimated incidence and mortality using the maximum facility capacity as denominator. The use of the occupancy rates in the LTCFs would have allowed more precise estimates. Third, there could also have been a bias related to the practice of COVID-19 testing, which could have been different depending on the type of facilities. In nursing homes, wide testing among residents and staff should be carried out when an outbreak occurs in the facility, and thus making it possible to detect large number of cases, particularly asymptomatic cases. However, facility-wide testing for COVID-19 among residents and staff after the identification of the first case in the facility was not performed during the study period (first wave of the pandemic), because of unavailability of tests. In addition and to our knowledge, COVID-19 outbreaks occurring in residential care facilities were not frequent, unlike nursing homes. Nonetheless, it is unlikely that a possible bias related to differences in testing practices would have influenced mortality related to COVID-19. Finally, we included possible cases defined by clinical presentation but no PCR conformation, in a context of LTCF with 1 or more COVID-19 confirmed cases. Several studies reported that symptomatology is very similar among COVID-19 suspected cases that later turned out to be positive or negative.22 This suggests that we may have overestimated the number of COVID-cases in this study. However, we think that, overall, these limitations could not affect the large differences observed in our study.
Conclusions and Implications
Our findings may inform other studies to better understand the factors associated with COVID-19 in LTCFs and may help better organize infection prevention activities in these settings. Infection control policies for LTCF including vaccination need to be tailored to specific setting type, with nursing homes requiring a higher level of priority than residential care facilities. Other studies in residential care settings could provide more insight on other countries because there might be some country-specific characteristics and organizational differences of these facilities that might influence inter human contacts and the risk of SARS-CoV-2 transmission.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Applegate W.B., Ouslander J.G. COVID-19 presents high risk to older persons. J Am Geriatr Soc. 2020;68:681. doi: 10.1111/jgs.16426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu K., Chen Y., Lin R., Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect. 2020;80:e14–e18. doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ioannou G.N., Locke E., Green P. Risk factors for hospitalization, mechanical ventilation, or death among 10 131 US Veterans with SARS-COV-2 infection. JAMA Netw Open. 2020;3:e2022310. doi: 10.1001/jamanetworkopen.2020.22310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.D’Adamo H., Yoshikawa T., Ouslander J.G. Coronavirus disease 2019 in geriatrics and long-term care: The ABCDs of COVID-19. J Am Geriatr Soc. 2020;68:912–917. doi: 10.1111/jgs.16445. [DOI] [PubMed] [Google Scholar]
- 6.Fallon A., Dukelow T., Kennelly S.P., O’Neill D. COVID-19 in nursing homes. QJM Mon J Assoc Physicians. 2020;113:391–392. doi: 10.1093/qjmed/hcaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White E.M., Kosar C.M., Feifer R.A. Variation in SARS-CoV-2 prevalence in U.S. skilled nursing facilities. J Am Geriatr Soc. 2020;68:2167–2173. doi: 10.1111/jgs.16752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ladhani S.N., Chow J.Y., Janarthanan R. Increased risk of SARS-CoV-2 infection in staff working across different care homes enhanced CoVID-19 outbreak investigations in London care Homes. J Infect. 2020;81:621–624. doi: 10.1016/j.jinf.2020.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Belmin J., Um-Din N., Donadio C. Coronavirus disease 2019 outcomes in French nursing homes that implemented staff confinement with residents. JAMA Netw Open. 2020;3:e2017533. doi: 10.1001/jamanetworkopen.2020.17533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ECDC Public Health Emergency Team. Danis K., Fonteneau L., Georges S. High impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA, May 2020. Euro Surveill. 2020;25:2000956. doi: 10.2807/1560-7917.ES.2020.25.22.2000956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.République Française et Caisse Nationale de Solidarité pour l’Autonomie Portail national d’information pour les personnes âgées et leurs proches. Les Résidences Autonomie, pour qui? https://www.pour-les-personnes-agees.gouv.fr/changer-de-logement/vivre-dans-une-residence-avec-services-pour-seniors/les-residences-autonomie-pour-qui Available at:
- 12.Fisman D.N., Bogoch I., Lapointe-Shaw L. Risk factors associated with mortality among residents with Coronavirus Disease 2019 (COVID-19) in long-term care facilities in Ontario, Canada. JAMA Netw Open. 2020;3:e2015957. doi: 10.1001/jamanetworkopen.2020.15957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gardner W., States D., Bagley N. The coronavirus and the risks to the elderly in long-term care. J Aging Soc Policy. 2020;32:310–315. doi: 10.1080/08959420.2020.1750543. [DOI] [PubMed] [Google Scholar]
- 14.McMichael T.M., Clark S., Pogosjans S. COVID-19 in a long-term care facility—King County, Washington, February 27-March 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:339–342. doi: 10.15585/mmwr.mm6912e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muller M. Ministère de la Solidarité et de la Santé, Direction de la Recherche, Études Evaluation et Statistiques (DREES); 2017. L’accueil des personnes âgées en établissement: Entre progression et diversification de l’offre; pp. 1–22. [The housing of elderly people in institutions: between progression and diversification of the offer.] [Google Scholar]
- 16.Caisse Nationale Solidarité Autonomie Etablissements d'Hébergement pour Personnes Agées Dépendantes is the official name use by authorities and law for nursing home in France [The situation of the Etablissements d'Hébergement pour Personnes Agées Dépendantes (EHPAD) in 2016. Budgetary analysis of resident care in EHPAD] https://www.cnsa.fr/node/3701 Available at: Published 2017. Accessed February 15, 2020.
- 17.National Center for Health, Vital and Health Statistics Long-term care providers and services users in the United States, 2015–2016. https://www.cdc.gov/nchs/data/series/sr_03/sr03_43-508.pdf Available at: Published 2019. Accessed December 1, 2020. [PubMed]
- 18.Santé Publique France Définition de cas d'infection au SARS-CoV-2 (COVID-19) https://www.santepubliquefrance.fr/media/files/01-maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/definition-de-cas-21-01-2021 Mise à jour le 21/01/2021 [Case definition of infection by the SRAS-CoV-2 (COVID-19). Updated 21 January 2021]. Available at:
- 19.Haute Autorité de Santé Rapport d'évaluation: Place des tests sérologiques dans la stratégie de prise en charge de la maladie COVID-19 [Evaluation report: Place of serological testing in the management strategy for COVID-19] https://www.has-sante.fr/jcms/p_3182357/fr/place-des-tests-serologiques-dans-la-strategie-de-prise-en-charge-de-la-maladie-covid-19-rapport-d-evaluation-technologique Available at:
- 20.World Health Organization WHO COVID-19 case definition. https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2020.2 Updated in Public health surveillance for CONVID-19. Available at:
- 21.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19). 2020 Interim case definition, approved August 5, 2020. https://wwwn.cdc.gov/nndss/conditions/coronavirus-disease-2019-covid-19/case-definition/2020/08/05 Available at:
- 22.Rutten J.J.S., van Loon A.M., van Kooten J. Clinical suspicion of COVID-19 in nursing home residents: Symptoms and mortality risk factors. J Am Med Dir Assoc. 2020;21:1791–1797.e1. doi: 10.1016/j.jamda.2020.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]