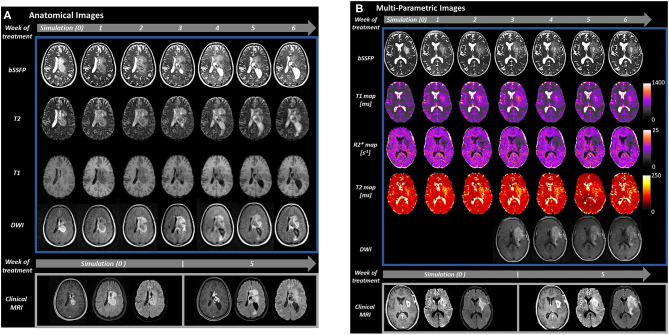
Figure 1.
Serial MRI of two patients with glioblastoma acquired during MRgRT on the 0.35 T MRIdian (Viewray, Cleveland, OH) combination MRI and RT system at the University of Miami (top of image, blue rectangle). Imaging was obtained at simulation (week 0) and daily on MRIdian through the course of treatment, though shown weekly for simplicity (gray arrows with treatment week number). Our MRIdian workflow for glioma patients includes 20 min for daily patient setup and intensity modulated RT which includes whole brain highly T2 weighted bSSFP (1.5 × 1.5 × 1.5 mm, 128 s) for positioning, 3D couch shifts applied by the therapist analogous to non-MRI guided RT systems, and cine MRI during RT for position verification through treatment. RT is then followed by 15 min per day of additional mpMRI imaging with the patient in the same position for a total daily time of about 35 min. Comparison images are shown for each patient from a 3 T Skyra (Siemens, Erlangen, Germany) clinical scanner (bottom of image, gray rectangle) during simulation and at week 5 (RT fraction 21) of treatment. (A) Anatomical images (bSSFP, T2, T1, and DWI) from a 29 year old woman with a centrally located glioblastoma (IDH-1 and IDH-2 mutations negative, MGMT non-hypermethylated, H3K27M mutation negative). The patient underwent biopsy 2 weeks prior to simulation, started RT 1 week after simulation, and received 6 weeks of radiation therapy to 60 Gy in 30 fractions on the MRIdian system with concurrent temozolomide. At the bottom of the figure, the clinical scans from the left to the right-hand side are T1 post-contrast, T2 FLAIR and DWI, respectively. During week 3 of treatment, the patient's left temporal lateral ventricle became obstructed by growth of the centrally located tumor and progressive enlargement was observed. The patient became symptomatic during week 4 with headache and nausea that was controlled with dexamethasone 2 mg twice daily. After consultation with neurosurgery, the patient's radiation therapy and chemotherapy course was completed without additional intervention. The gadolinium enhancing tumor at fraction 21 had grown 7 mm outside of the gross tumor volume defined at simulation. (B) Multi-parametric images of a 58 year old woman with partially resected glioblastoma (IDH-1 R132H wildtype, MGMT non-hypermethylated) of the left temporal lobe with unresected portions extending into the left basal ganglia and corona radiata as shown. From top to bottom, bSSFP, T1, R2*, and T2 maps, and DWI are presented. DWI data was not available on our MRIdian system until the third week of treatment when it was added to our acquisition protocol every other day. On the bottom of the image, comparison 3 T scans at simulation and week 5 (fraction 21) from the left to the right hand side are T1 post-contrast, T2 FLAIR and DWI, respectively. This patient had progressive growth throughout treatment that was particularly prominent on fraction 21 T1 post-contrast scan (enhancing gross tumor volume margin growth of 8 mm) and R2* mapping.