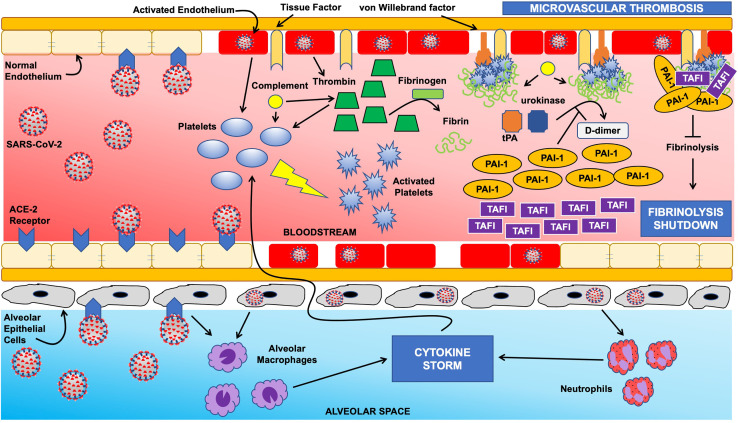
Figure 1.
Schematic of fibrinolysis shutdown mechanisms in COVID-19. The normal homeostasis between coagulation and fibrinolysis is severely disrupted in COVID-19. Infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) via the angiotensin converting enzyme 2 (ACE-2) receptor on endothelial cells results in activation of the endothelium, which in turn augments platelet activation and thrombin generation. Endothelial injury leads to exposure of tissue factor and von Willebrand factor, initiating the coagulation cascade, with the end result of platelet- and fibrin-rich thrombus on the endothelial surface. These mechanisms are further accentuated by a massive influx of cytokines (ie “cytokine storm”) as a result of alveolar macrophage and neutrophil activation secondary to viral invasion via ACE-2 receptors on alveolar epithelial cells. Normally, endothelial fibrin accumulation is prevented from progressing to microvascular thrombosis via the fibrinolytic agents tissue plasminogen activator (tPA) and urokinase; however, infection with SARS-CoV-2 results in overwhelming levels of plasminogen activator inhibitor 1 (PAI-1) and thrombin activatable fibrinolysis inhibitor (TAFI) with the net result of fibrinolysis shutdown.