Administrative and financial support provided by Paralyzed Veterans of America
These guidelines have been prepared based on scientific and professional information available in 2019. Users should periodically review this material to ensure that the advice herein is consistent with current reasonable clinical practice. The websites noted in this document were current at the time of publication; however, because web addresses and the information contained therein change frequently, the reader is encouraged to stay apprised of the most current information.
Consortium for Spinal Cord Medicine
Member Organizations and Steering Committee Representatives
Thomas Bryce, MD Chair
Academy of Spinal Cord Injury Professionals Nurses Section
Lisa A. Beck, MS, APRN, CNS, CRRN
Academy of Spinal Cord Injury Professionals Psychologists Social Workers and Counselors Section
Charles H. Bombardier, PhD
Academy of Spinal Cord Injury Professionals Physicians Section
Mary Ann Richmond, MD, DVM, MS
American Academy of Neurology
Peter Gorman, MD, FAAN
American Academy of Orthopedic Surgeons
E. Byron Marsolais, MD, PhD
American Academy of Physical Medicine and Rehabilitation
David Chen, MD
American Association of Neurological Surgeons
Gregory Hawryluk, MD, PhD, FRCSC
American College of Emergency Physicians
William C. Dalsey, MD, FACEP
American Congress of Rehabilitation Medicine
Casey Azuero, PhD
American Occupational Therapy Association
Theresa Gregorio-Torres, OTR, MA, ATP
American Physical Therapy Association
Rachel Tappan, PT, DPT
American Psychological Association Division 22
Charles H. Bombardier, PhD
American Spinal Injury Association
Gregory Nemunaitis, MD
Association of Academic Physiatrists
William O. McKinley, MD
Association of Rehabilitation Nurses
Donna Williams, MSN, RN, CRRN
Christopher and Dana Reeve Foundation
Bernadette Mauro
Congress of Neurological Surgeons
Paul C. McCormick, MD
Insurance Rehabilitation Study Group
Debra Mayo, RN, BS, CCM
International Spinal Cord Society
Denise G. Tate, PhD, ABPP
Paralyzed Veterans of America
Stephen Yerkovich, MD
PRAXIS
Colleen O'Connell, MD, FRCSC
Society of Critical Care Medicine
Pauline K. Park, MD, FCCM
United Spinal Association
Jane Wierbicky, RN
U.S. Department of Veterans Affairs
Stephen Burns, MD
Preface
Suicide is at least 3 times more common in individuals with spinal cord injury (SCI) than in individuals without SCI, and anxiety and posttraumatic stress disorder (PTSD) are at least twice as prevalent. Substance use is also significantly more prevalent. However, even though individuals with SCI usually have contact with health care professionals, these mental health disorders are often not recognized and therefore often not addressed optimally, perhaps because of the other more obvious physical health impairments caused by SCI and the stigma that surrounds mental health disorders.
This clinical practice guideline (CPG), which has been in development for over 15 years, is long overdue. Fortunately, however, during this time, progress has been made in recognizing the extent of the problem and beginning to evaluate potential treatments. This CPG has been rigorously developed with the thought that implementable things can be done to improve the recognition and treatment of mental health disorders, specifically depression and anxiety, PTSD, substance use disorders, and suicide prevention. It is anticipated that this important and practical work will educate clinicians about the scope of the problems and raise awareness about the availability of the means to accurately diagnose and treat these disorders.
We are fortunate to have the representation of all the various stakeholders in the development and peer review of this CPG, including all of the subspecialists who are impacted by these recommendations, ranging from experts in psychiatry and psychology to rehabilitation professionals. We hope that this wide- ranging representation will translate into uniform quality practice through the widespread use of this CPG to guide the detection and treatment of mental health and substance use disorders in all settings, which can only result in the best outcomes and least amount of morbidity and mortality for individuals who experience SCI.
On behalf of the consortium steering committee, I want first to acknowledge the leadership of the Chair, Charles Bombardier, in guiding this panel inexorably through the seemingly unending development process over the past decade. Next to be commended are the panel members themselves for keeping to task, even as many have retired along the way, and the many reviewers who provided valuable feedback from all areas. All these people, including the panel Chair, have volunteered their time to help produce this superb document. In addition, I wish to acknowledge the ongoing support of the Paralyzed Veterans of America, especially President David Zurfluh, Executive Director Carl Blake, and Director of Research and Education Cheryl Vines, as well as the rest of the leadership team without whose support these guidelines would not exist.Thomas BryceChair Consortium for Spinal Cord Medicine
Foreword
This clinical practice guideline (CPG) has had a long gestation period. We owe a great debt of gratitude to those who long ago envisioned and nurtured the idea of a broad psychosocial CPG that would further define and elevate standards of care for individuals with spinal cord injury (SCI). In March 2003, Lester Butt, PhD, presented a 5-phase proposal to the Consortium for Spinal Cord Medicine (“the Consortium”) to develop a psychosocial CPG. The proposal called for the establishment of a psychosocial workgroup led by Dr. Butt and joined by Helen Bosshart, LCSW, ACSW; Bob Sontag, MSW; Hugh Taylor, MSW; Pat Tracy, MSW; Chuck Bombardier, PhD; Scott Richards, PhD; and Dan Rohe, PhD. Don Kewman, PhD, and Romel Mackelprang, DSW, were identified as topic champions for the CPG. Dr. Butt and colleagues constructed a compendium of psychosocial issues from which the CPG topics could be chosen. They next developed 2 parallel surveys to identify the most important topics for inclusion in the CPG from the perspectives of individuals with SCI, as well as SCI physicians, psychologists, and social workers. Results of that survey were bundled into a CPG proposal that incorporated psychosocial comorbidities (e.g., pain, substance abuse, traumatic brain injury, diagnoses listed in the 4th edition of the Diagnostic and Statistical Manual of Mental Disorders [DSM-IV]), health/wellness/quality of life (e.g., coping, sexuality, family, aging, compliance), community reintegration, psychosocial treatment approaches, summary, and future directions. The proposed content was recognized by the Consortium as identifying important aspects of psychosocial care for individuals with SCI; however, the comprehensive nature of the proposal was felt by the Consortium to be overly ambitious and consequently impractical, given available time and resources. In 2005, the Consortium unsuccessfully sought support from the Agency for Healthcare Research and Quality, Evidence-based Practice Centers, to complete the literature reviews and evidence grading for the psychosocial CPG. In 2008, Don Kewman, Lester Butt, and I met to discuss potential ways forward. During that meeting, we decided to take a “Swiss cheese” approach and identify smaller, doable, but still meaningful psychosocial domains that could be the subject of several separate CPGs. The topic of sexuality had already been selected as a stand-alone CPG topic. Ultimately, the group decided to focus the second psychosocial CPG on common disorders in the American Psychiatric Association DSM-IV that were prevalent in SCI: depression, anxiety/posttraumatic stress disorder (PTSD), and substance use. We reasoned that these conditions were not only prevalent, but they were clinically important, clearly defined, and the subject of considerable research that could inform care and could benefit from a guideline to elevate and enhance current standards of care. In about 2010, I took over the leadership of the revised CPG. The Consortium approved of the more narrowly focused CPG proposal, but other new and revised CPGs were already in the pipeline and so a start date was deferred. The Great Recession, limited resources, and more urgent emerging priorities delayed the commencement of this CPG until 2016. Still, the Paralyzed Veterans of America (PVA) and their CPG directors and managers proved their mettle by sustaining the CPG program through difficult times and kept their commitment to see this CPG through to completion.
I am deeply grateful to the PVA for financial and institutional support. I am especially thankful for the PVA staff who have guided and enabled the development of this CPG over the years: Kim Nalle, Lana McKenzie, Christina Arenas, Caryn Cohen, Kera Lawson, Rita Obi, and Cheryl Vines, as well as PVA consultant J. Paul Thomas. Consortium chairs Larry Vogel and Tom Bryce have been ardent supporters of psychosocial research and this CPG. The methodology team at the Pacific Northwest Evidence-based Practice Center, Oregon Health & Science University, led by Shelly Selph, MD, MPH, along with Jessica Griffin, MS, and Ryan C. Stoner, PhD, produced an excellent systematic review of the literature and responded to comments and additional requests in a very collegial manner. I am also thankful for the Veterans Administration/Department of Defense guidelines on treating depression, substance use disorders, tobacco use, PTSD, acute stress disorder, and suicide management, which we have quoted heavily. These and other guidelines have formed the basis for many of the recommendations that we have provided where relevant information from individuals with SCI is lacking.
I also want to recognize at least a few of the pioneering researchers who embraced an empirical approach to understanding psychosocial aspects of SCI: Fiona Judd, Roberta Trieschmann, J. Scott Richards, Robert Frank, Timothy Elliott, Ashley Craig, Paul Kennedy, James Krause, Bryan Kemp, and Denise Tate. These individuals and their colleagues modeled evidence- based approaches and produced an early foundation of empirical support on which to base assessment and treatment practices. They inspired me and the next generation of psychosocial researchers to build on what they had discovered. No CPG provides final answers. May this CPG point us toward a higher standard of care for now, eventually to be challenged, updated, and replaced with better information, more effective methods, and improved standards of care.
This is what individuals living with SCI deserve from us.
Charles H. Bombardier, PhDPanel Chair
Acknowledgments
Paralyzed Veterans is proud to sponsor the development and dissemination of the SCI CPGs. For over twenty five years we have partnered with the Consortium of Spinal Cord Medicine in a shared mission to improve the health of individuals living with SCI. Today, hundreds of thousands of copies of the guidelines are used around the world by physicians and other medical professionals who provide care to individuals living with SCI at every level, from the emergency department to acute care, rehabilitation to community services.
We thank Dr. Bombardier for his leadership and perseverance in guiding this important new guideline into practice. Sincere thanks is also extended to each of the panel members who worked tirelessly, without remuneration, to bring this project to fruition. Dr. Thomas Bryce and the members of the SCI Consortium have provided vision, leadership and support bring this and many other clinical practice guidelines to completion. Their efforts and those of the field reviewers assure the high quality of the recommendations.
As with any project of this magnitude, many were involved in the process. Sincere appreciation goes to Dr. Shelly Selph and her team at the Pacific Northwest Evidence-based Practice Center, Oregon Health and Science University, who conducted the review of literature and methodology for this guideline.
Within Paralyzed Veterans, work on this guideline benefitted from the efforts of nearly every department. But special appreciation goes to our graphic designers Jonathan Franklin and Kevin Johnson.
Finally, it is only with the significant, mission-driven support of Paralyzed Veterans, our leadership and our members, that we are able to provide these services. Sincere thanks to Paralyzed Veterans President David Zurfluh, Past President Al Kovach, Executive Director Carl Blake and Deputy Executive Director Shaun Castle for their support.
Panel Members
Casey B. Azuero, PhD, MPH
Assistant Professor
Department of Physical Medicine and Rehabilitation University of Alabama at Birmingham
Birmingham, AL
Charles H. Bombardier, PhD, ABPP, Panel Chair
Professor
Department of Rehabilitation Medicine University of Washington
Seattle, WA
Jesse R. Fann, MD, MPH
Professor
Department of Psychiatry and Behavioral Sciences Adjunct Professor,
Department of Rehabilitation Medicine
Adjunct Professor, Department of Epidemiology University of Washington
Seattle, WA
Donald D. Kautz, RN, PhD
Associate Professor Emeritus School of Nursing
University of North Carolina - Greensboro Greensboro, NC
J. Scott Richards, PhD, ABPP
Professor Emeritus
Department of Physical Medicine and Rehabilitation University of Alabama at Birmingham
Birmingham, AL
Sunil Sabharwal, MD
Chief of Spinal Cord Injury
VA Boston Health Care System
Associate Professor of Physical Medicine and Rehabilitation
Harvard Medical School Boston, MA
Expert Reviewers
Academy of Spinal Cord Injury Professionals – Nurses Section
Lisa Beck MS, APRN, CNS, CRRN
Mayo Clinic Rochester, MN
Academy of Spinal Cord Injury Professionals – Physicians Section
M. Kristi Henzel, MD, PhD
Louis Stokes VA Medical Center
SCI&D Center
Cleveland, OH
Binnan Ong, DO
Louis Stokes VA Medical Center
Cleveland, OH
Academy of Spinal Cord Injury Professionals – Psychologists, Social Workers & Counselors Section
Catherine Smith Wilson, PsyD. ABPP
Denver, CO
American Academy of Physical Medicine and Rehabilitation
David Chen, MD
Shirley Ryan Abilities Lab
Chicago, IL
American Congress of Rehabilitation Medicine
Heather Asthagiri, MD
Charlottesville, VA
American Occupational Therapy Association
Theresa Gregorio – Torres, MA, OTR, ATP
TIRR Memorial Hermann Houston, TX
American Physical Therapy Association
Casey L. Holleran, MPY, DHS, NCS Washington University
St. Louis, MO
Rachel Tappan, PT, DPT Northwestern University Chicago, IL
American Psychological Association-Div. 22
Lisa A. Brenner, PhD
Rehabilitation Psychology
Denver VA Medical Center
Denver, CO
Tiffany Meites, PhD, ABPP
Barrow Neurological Institute
Phoenix, AZ
American Spinal Injury Association
Thomas M. Dixon, PhD ABPP
Louis Stokes VA Medical Center
Cleveland, OH
Angela M. Kuemmel, PhD, ABPP
Louis Stokes VA Medical Center
Cleveland, OH
Gregory Nemunaitis MD
MetroHealth Rehabilitation
Institute of Ohio Medical Center
Cleveland, OH
Department of Veterans Affairs
Stephen Burns, MD
Puget Sound VA Medical Center
Seattle, WA
Sarah Clay, PharmD
Richard L. Roudebush VA Medical Center
Indianapolis, IN
Karen Drexler, MD
Atlanta VA Medical Center Decatur, GA
Damon A. Gray, MD
Long Beach VA Medical Center SCI&D Center
Long Beach, CA
Randi Lincoln, PhD
Puget Sound VA Medical Center Seattle, WA
Catherine A. Rotolo, LISW-S Office of Mental Health & Suicide Prevention Washington, DC
Elizabeth A. Tammaro BSN, RN, CRRN
VA Boston Health Care system Boston, MA
Nicole Theriot, LCSW
Office of Mental Health & Suicide Prevention
Washington, DC
Insurance Rehabilitation Study Group
Andrew Phillips, MD Salt Lake City, UT
International Spinal Cord Society
Marcel Post, PhD Utrecht, The Netherlands
Denise Tate, PhD, ABPP
University of Michigan Ann Arbor, MI
Invited Expert Reviewers
Lester Butt, PhD, ABPP
Craig Hospital Englewood, CO
Ashley Craig, PhD
St. Leonards, NSW, Australia
Abbreviations
ASD – Acute Stress Disorder
AUDIT-C – Alcohol Use Disorders Identification Test-Consumption
BDI – Beck Depression Inventory
CAGE-AID – CAGE Adapted to Include Drugs
CBT – cognitive behavioral therapy
CDC HRQOL-14 – Centers for Disease Control and Prevention Health-Related Quality of Life Measure
CPG – clinical practice guideline
CRAFT - Community Reinforcement Approach and Family Training
C-SSRS – Columbia Suicide Severity Rating Scale
DoD – Department of Defense
DSM – Diagnostic and Statistical Manual of Mental Disorders
DSM-IV – Diagnostic and Statistical Manual of Mental Disorders, 4th edition
DSM-5 – Diagnostic and Statistical Manual of Mental Disorders, 5th edition
FDA – Food and Drug Administration
FIM – Functional Independence Measure
GAD – generalized anxiety disorder
GAD-7 – Generalized Anxiety Disorder 7-item scale
GRADE – Grading of Recommendations Assessment, Development and Evaluation
HADS – Hospital Anxiety and Depression Scale
MAT – medication-assisted treatment
MBC – measurement-based care
MDD – major depressive disorder
NPV – negative predictive value
OAHMQ – Older Adult Health and Mood Questionnaire
PC-MHI – Primary Care-Mental Health Integration
PD – panic disorder
PHQ – Patient Health Questionnaire
PHQ-2 – 2-item Patient Health Questionnaire-2
PHQ-4 – 4-item Patient Health Questionnaire-4
PHQ-9 – 9-item Patient Health Questionnaire-9
PPV – positive predictive value
PROMIS – Patient-Reported Outcomes Measurement Information System
PTSD – posttraumatic stress disorder
PVA – Paralyzed Veterans of America
QUIPS – Quality in Prognostic Studies
RCT – randomized controlled trial
SAMHSA – Substance Abuse and Mental Health Services Administration
SBIRT – Screening, Brief Intervention, and Referral to Treatment
SCI – spinal cord injury
SCID DSM-III-R – Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, 3rd edition, revised
SCID DSM-IV – Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, 4th edition
SCI-QOL – Spinal Cord Injury-Quality of Life
SF-36 – 36-Item Short Form Health Survey
SNRI – serotonin-norepinephrine reuptake inhibitor
SSRI – selective serotonin reuptake inhibitor
SUD – substance use disorder
TAPS – Tobacco, Alcohol, Prescription Medication, and Other Substance Use
TBI – traumatic brain injury
TICS – Two-Item Conjoint Screening test
VA – United States Department of Veterans Affairs
Zung SDS – Zung Self-Rating Depression Scale
Conditions Covered
- AD – Anxiety disorders
- GAD – Generalized anxiety disorder
- PD – Panic disorder
MDD – Major depressive disorder
SUDs – Substance use disorders
PTSD – Posttraumatic stress disorder
ASD – Acute stress disorder
Suicide
Grading of the Recommendations
The overall objective of this guideline is to improve the care of individuals with SCI by guiding clinicians and policy makers with its recommendations. The following recommendations use available evidence and—where evidence is limited—panel experience and consensus. The panel based its evidence ratings primarily on research in which the focus of the study was SCI. This information was supplemented by using evidence from trials, guidelines, and expert opinions contained in the scientific literature of non-SCI populations.
For individual patients, decisions are best made by considering these recommendations combined with clinical judgment, the latter based on specific knowledge about each patient’s risk factors, the potential for adverse effects, and the availability of various options within one’s center. The bracketed rating refers to the level of scientific evidence, the strength of the evidence, and the level of panel agreement with the recommendations (Tables 2–4).
Table 2.
Levels of Scientific Evidence
| Level | Description |
|---|---|
| I | Evidence based on randomized controlled clinical trials (or meta-analysis of such trials) of adequate size to ensure a low risk of incorporating false-positive or false-negative results. |
| II | Evidence based on randomized controlled trials that are too small to provide Level I evidence. These may show either positive trends that are not statistically significant or no trends and are associated with a high risk of false-negative results. |
| III | Evidence based on nonrandomized, controlled, or cohort studies; case series; case-controlled studies; or cross-sectional studies. |
| IV | Evidence based on the opinion of respected authorities or expert committees as indicated in published consensus conferences or guidelines. |
| V | Evidence that expresses the opinion of those individuals who have written and reviewed this guideline, based on experience, knowledge of the relevant literature, and discussions with peers. |
Sources: Adapted from Sackett DL. Rules of evidence and clinical recommendation on the use of antithrombotic agents. Chest. 1989 95(suppl 2):2S-4S;1 and U.S. Preventive Health Services Task Force. Guide to Clinical Preventive Services. 2nd ed. Baltimore, MD: Williams and Wilkins; 1996.2
Table 3.
Categories of the Strength of Evidence Associated with the Recommendations
| Category | Description |
|---|---|
| A | The guideline recommendation is supported by one or more Level I studies. |
| B | The guideline recommendation is supported by one or more Level II studies. |
| C | The guideline recommendation is supported by only one or more Level III, IV or V studies |
Table 4.
Levels of Panel Agreement with the Recommendations
| Level | Mean Agreement Score |
|---|---|
| Low | 1.0 to less than 2.33 |
| Moderate | 2.33 to less than 3.87 |
| Strong | 3.87 to 5.0 |
Nomenclature for Rating of Evidence and Strength of Panel Agreement
Executive Summary of the Recommendations
GENERAL CROSS-CUTTING RECOMMENDATIONS
1. Screening, Assessment, and Treatment
1.1 Integrate mental health professionals with education, training, and experience in spinal cord injury (SCI), as well as in general mental health and substance use disorders (SUDs) within comprehensive inpatient and outpatient SCI rehabilitation programs.
| Level IV | Strength C | Agreement strong |
1.2 Routinely screen all individuals with SCI for mental health disorders, SUDs, and suicide risk as part of inpatient and outpatient rehabilitation.
| Level IV | Strength C | Agreement strong |
1.3 Include current symptoms and lifetime history in screening and assessment of mental health disorders and SUDs.
| Level IV | Strength C | Agreement strong |
1.4 Refer individuals who screen positive for a mental health disorder or SUD to a mental health professional for a diagnostic assessment and initiation of treatment, if indicated.
| Leve IV | Strength C | Agreement strong |
1.5 Engage individuals with a mental health disorder or SUD in shared decision making for their treatment.
| Level IV | Strength C | Agreement strong |
1.6 Systematically evaluate valid and standardized measures of progress to inform care and adjust treatment (measurement-based care [MBC]) for mental health disorders or SUDs.
| Level IV | Strength C | Agreement strong |
1.7 Refer to follow-up treatment and coordinate care upon discharge or transition to the next phase of care, if indicated.
| Level IV | Strength C | Agreement strong |
DIAGNOSIS-SPECIFIC DISORDERS
2. Anxiety Disorders
2.1 Use a brief, valid measure that has good sensitivity to screen all patients for general anxiety and panic disorders (PDs): (a) early during initial inpatient hospital or rehabilitation stay; (b) as a repeat screen if indicated to assess persistence of symptoms or change in status; (c) at the first post-discharge follow-up point; and (d) at future time points, depending on risk stratification factors such as prior positive anxiety screening results or preinjury history of psychological disorder.
| Level IV | Strength C | Agreement strong |
2.2 Refer patients with positive screen results or those suspected of having an anxiety disorder to a mental health provider for a diagnostic assessment to assess for conditions such as generalized anxiety disorder (GAD) or PD. Rule out the possibility that the symptoms are better explained by the effects of the medical condition, medications, drugs, the environment, or other factors.
| Level IV | Strength C | Agreement strong |
2.3 To minimize anxiety, support anxious patients with specific and nonspecific therapeutic strategies, provided by all health care professionals (physicians, nurses, therapists, psychologists, social workers, and others) who work with them.
| Level IV | Strength C | Agreement strong |
2.4 Treat GAD, PD, or other clinically significant anxiety by using pharmacological and/or nonpharmacological interventions on the basis of salient clinical considerations and patient preferences.
| Level IV | Strength C | Agreement strong |
2.4.1 Consider pharmacological treatment for anxiety, if indicated.
| Level IV | Strength C | Agreement strong |
2.4.2 Consider nonpharmacological treatment for anxiety.
| Level IV | Strength C | Agreement strong |
3. Major Depressive Disorder (MDD)
3.1 Screen all individuals with SCI for major depression by using a brief, valid measure that has good sensitivity and specificity: (a) early during the initial inpatient hospital or rehabilitation stay; (b) as a repeat screen if indicated to assess persistence of symptoms or change in status; (c) at the first discharge follow-up point; and (d) at least annually or more frequently, depending on risk stratification factors such as prior positive screening results and chronic pain.
| Level IV | Strength C | Agreement strong |
3.2 Refer patients with positive screen results or those suspected of having a depressive disorder to a mental health provider for a diagnostic assessment.
| Level IV | Strength C | Agreement strong |
3.3 Follow up on positive screening test results by using a valid diagnostic assessment to confirm conditions such as major depressive disorder (MDD) or adjustment disorder (including sufficient persistence of symptoms and interference with rehabilitation or role functioning) and rule out the possibility that the symptoms are better explained by the effects of the medical condition, medications, drugs, the environment, or other factors.
| Level IV | Strength C | Agreement strong |
3.4 Support patients with major depression with nonspecific and depression-specific relationship skills, used by all health care professionals (physicians, nurses, therapists, psychologists, social workers, and others) who work with them.
| Level IV | Strength C | Agreement strong |
3.5 Treat major depression by using pharmacological and/or nonpharmacological approaches on the basis of clinical presentation (e.g., comorbid conditions), treatment efficacy, and patient preferences.
| Level I | Strength A | Agreement strong |
3.5.1 Consider pharmacological treatments for major depression.
| Level I | Strength A | Agreement strong |
3.5.2 Consider nonpharmacological treatments for major depression.
| Level I | Strength A | Agreement strong |
4. Substance Use Disorders (SUDs)
4.1 Screen all patients for common SUDs: (a) Before discharge from inpatient rehabilitation, use a brief, valid measure that has good sensitivity to screen for lifetime use of and problems with alcohol, other (illicit) drugs, tobacco, marijuana, and nonmedical use of prescription medications; and, (b) depending on initial screening results and other risk factors, rescreen patients for recent substance use in outpatient rehabilitation or primary care.
| Level IV | Strength C | Agreement strong |
4.2 Refer patients with positive screen results or those suspected of having an SUD to a mental health provider for a diagnostic assessment of SUD criteria.
| Level IV | Strength C | Agreement strong |
4.3 Support patients with SUD with nonspecific and SUD-specific relationship skills, used by all health care professionals (physicians, nurses, therapists, psychologists, social workers, and others) who work with them.
| Level IV | Strength C | Agreement strong |
4.4 Treat SUDs, within rehabilitation to the extent possible, by using pharmacological, nonpharmacological, and community-based approaches on the basis of clinical presentation (e.g., comorbid conditions), length of stay, treatment efficacy, and patient preferences.
| Level IV | Strength C | Agreement strong |
4.5 Use medication-assisted treatment (MAT) for SUDs, including opioid use and alcohol use disorders, when indicated.
| Level IV | Strength C | Agreement strong |
4.6 Consider nonpharmacological treatments for SUDs.
| Level IV | Strength C | Agreement strong |
4.7 Consider referral to community-based SUD treatment programs and self-help resources.
| Level IV | Strength C | Agreement strong |
5. Posttraumatic Stress Disorder (PTSD) and Acute Stress Disorder (ASD)
5.1 Screen all patients for ASD within 1 month of SCI and for PTSD after the first month. Screening should occur (a) early during initial inpatient hospital or rehabilitation stay; (b) as a repeat screen if indicated to assess persistence of symptoms or change in status; (c) at the first post-discharge follow-up point; and (d) at future time points beyond 6 months, depending on risk stratification factors, such as being a veteran or other trauma- exposed professional or having subthreshold symptom severity on prior screening examinations.
| Level IV | Strength C | Agreement strong |
5.2 Refer patients with positive screen results or those suspected of having ASD or PTSD to a mental health provider for a diagnostic assessment of ASD or PTSD criteria.
| Level IV | Strength C | Agreement strong |
5.3 Support patients with PTSD with nonspecific and PTSD-specific relationship skills, used by all health care professionals (physicians, nurses, therapists, psychologists, social workers, and others) who work with them.
| Level IV | Strength C | Agreement strong |
5.4 Treat ASD and PTSD, within rehabilitation to the extent possible, by using pharmacological and nonpharmacological approaches on the basis of treatment efficacy, clinical presentation (e.g., comorbid conditions), length of stay, and patient preferences.
| Level IV | Strength C | Agreement strong |
5.5 Offer patients with brief, evidence-based psychological interventions to treat ASD and prevent PTSD within the first 30 days after injury.
| Level IV | Strength C | Agreement strong |
5.6 Offer patients with PTSD evidence-based, trauma-focused psychological treatment.
| Level IV | Strength C | Agreement strong |
5.7 Offer patients with ASD pharmacological treatment if trauma-focused psychotherapies are not available or not preferred.
| Level IV | Strength C | Agreement strong |
5.8 Offer patients with PTSD pharmacological treatment if trauma-focused psychotherapies are not available or not preferred.
| Level IV | Strength C | Agreement strong |
6. Suicide
6.1 Formally screen individuals with SCI for suicidal ideation by using a brief, standardized, evidence-based screening tool. Screen for suicidal intent and behavior in individuals who report suicidal ideation. Screen (a) early during the initial inpatient hospital or rehabilitation stay, (b) as a repeat screen if indicated to assess persistence of symptoms or change in status, (c) at an early discharge follow-up point, and (d) at least annually or more frequently depending on risk stratification factors.
| Level IV | Strength C | Agreement strong |
6.2 Recognize warning signs for suicide and expedite evaluation of such signs by a trained professional. Take immediate follow-up action for anyone who displays direct warning signs for suicide (e.g., suicidal communication, preparation for suicide, and/or seeking access to or recent use of lethal means).
| Level IV | Strength C | Agreement strong |
6.3 Stratify suicide risk on the basis of severity and temporality (acute or chronic) to determine appropriate therapeutic interventions and care setting.
| Level IV | Strength C | Agreement strong |
6.3.1 Facilitate comprehensive assessment by a trained professional to integrate information about suicidal intent and behavior, warning signs, ability to maintain safety, and factors that impact risk of suicidal acts.
| Level IV | Strength C | Agreement strong |
6.3.2 Hospitalize individuals with high acute risk for suicide to maintain their safety, and aggressively target modifiable factors. Directly observe them in a secure environment with limited access to lethal means (e.g., kept away from items with sharp points or edges, cords/tubing, toxic substances).
| Level IV | Strength C | Agreement strong |
6.3.3 Address chronic increased risk for suicide in the context of long-term outpatient therapy with established providers, adjusting frequency of contact on the basis of risk level.
| Level IV | Strength C | Agreement strong |
6.4 Establish a treatment plan for high-risk individuals that fosters therapeutic alliance with mental health professionals and includes evidence-based suicide-focused psychotherapies.
| Level IV | Strength C | Agreement strong |
6.5 Optimize treatment for coexisting mental health and medical conditions that may impact the risk of suicide.
| Level IV | Strength C | Agreement strong |
6.6 Educate the at-risk individual, family, and caregivers on suicide risk and treatment options. Provide information on suicide prevention resources, including crisis lines and services, e.g., the National Suicide Prevention Lifeline number 1-800-273-8255 or 1-800-273-TALK. Provide information to veterans of the U.S. Armed Services about veteran-specific suicide prevention resources including a Veterans Crisis Line accessed by pressing 1 after dialing 1-800- 273-8255, online chatting at VeteransCrisisLine.net, or sending a text to 838255)”.
| Level IV | Strength C | Agreement strong |
6.7 Establish a safety plan for individuals considered to be at high risk for suicide. Limit access to lethal means (e.g., restricting access to firearms, making use of gun locks, limiting medication supply).
| Level IV | Strength C | Agreement strong |
6.8 Augment personal and environmental protective factors that may mitigate suicide risk. Enhance coping skills.
| Level IV | Strength C | Agreement strong |
Introduction
This guideline is the second Consortium for Spinal Cord Medicine clinical practice guideline (CPG) on mental health. The first mental health guideline, published in 1998, focused exclusively on depression after SCI. We now know that a number of mental health disorders and SUDs are prevalent and contribute to additional suffering and disability in individuals with SCI.3 Therefore, this guideline focuses on recognition and treatment of the most common mental health conditions in SCI: depression, anxiety, PTSD, and SUDs. The guideline also includes specific sections on detection and management of suicide because of the elevated risk of completed suicide among individuals living with SCI.
This CPG was designed for SCI rehabilitation professionals who are not mental health specialists a well as for those who are. Therefore, we need to begin with foundational concepts such as how mental health disorders and SUDs are defined. According to the most recent edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM), the 5th edition (DSM-5) published in 2013, mental illnesses are “health conditions involving changes in thinking, emotion or behavior (or a combination of these). Mental illnesses are associated with distress and/or problems functioning in social, work or family activities.”4 SUDs occur when the use of substances (e.g., alcohol, tobacco, cannabis, inhalants, stimulants, hallucinogens, and opioids) cause significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school, or home.4 In the DSM-5, mild, moderate, and severe SUDs replace the diagnoses of substance abuse and substance dependence found in the 4th edition of the DSM (DSM-IV).5
Mental health and SUDs are common in the general population and even more so in individuals with SCI. Each year, 1 in 5 Americans is affected by mental illness and 1 in 12 by an SUD. There is evidence to suggest that individuals with SCI are at greater risk of mental illness and substance use. Estimates of depression in the first year after SCI range from 20% to 40%.3,6 Estimates range from 13% to 40%7–10 for anxiety disorders following SCI. Between 25% and 96% of individuals with SCI used alcohol prior to injury and 32% to 35% used illegal drugs.11 Suicide is the cause of SCI in 0% to 6.8% of cases and is reported to be the cause of death in 5.8% to 11% of decedents with SCI.12 Comorbid mental illnesses and SUDs aversely influence SCI-related symptoms such as pain, as well as functioning, level of independence, community participation, quality of life, and mortality.3 Yet, mental health and SUDs seem to be underrecognized and undertreated in individuals with SCI.13,14
Under-recognition may occur because SCI is a catastrophic injury that blurs the lines between normal emotional responses and mental health disorders. Undertreatment may stem from poor recognition, as well as a failure to use rehabilitation as a window of opportunity to intervene in mental health and SUD conditions. Treatment of mental illness and SUDs is becoming more integrated into regular medical15 and trauma care.16 This is a trend that should be followed in SCI rehabilitation because it can be more effective17 and consistent with mental health treatment preferences in individuals with SCI.18 Consequently, we hope that consumers of this guideline—professionals, students, individuals with SCI and their loved ones—find a document that answers practical questions regarding the prevalence and risk factors for these disorders, how to screen for and assess these conditions, and what can be done to treat mental illness and SUDs, especially within rehabilitation settings.
This CPG does not address other psychological concepts such as adjustment, grief, resilience, coping, and so forth except to the extent that these variables are related to the included mental health conditions. While these other psychological factors may be important, they were judged to be too expansive and to lack consensus definitions to be included in this CPG.
The Consortium for Spinal Cord Medicine
The Consortium is a collaboration of professional and consumer organizations funded and administered by the Paralyzed Veterans of America (PVA). The Steering Committee, administratively supported by the PVA’s Research and Education Department, is made up of 1 representative from each Consortium-member organization. The Consortium’s mission is to direct the development and dissemination of evidence-based CPGs and companion consumer guides. This mission is solely directed to improving the health care and quality of life for individuals with SCI.
Summary of Guidelines Development Process
The development of these guidelines involved the following major steps: creating a list of formal questions to be addressed, systematic searches of published literature related to these questions, critical appraisal of the quality of the retrieved studies, abstraction of relevant study results, creation of evidence-based recommendations, writing and revising of various drafts of text that explain the recommendations, and multiple reviews by panel members and outside organizations. The Consortium’s CPG development process also involved extensive field review and a legal review.
Methodology
Literature Search
A medical librarian searched Ovid MEDLINE (through August 22, 2016), PsycINFO (through July, 2016), the Cochrane Central Register of Controlled Trials (through July, 2016), and the Cochrane Database of Systematic Reviews (through August 17, 2016) by using search terms related to chronic SCI. See Appendix A for complete search strategies. We also attempted to identify additional studies through hand searches of reference lists of included studies and reviews. All citations were imported into an electronic database (Endnote X7, Thomson Reuters).
Study Selection
Selection of included studies was based on inclusion criteria created in consultation with the PVA. Two reviewers independently assessed titles and abstracts of citations identified through literature searches for inclusion by using the criteria below. Full-text articles of potentially relevant citations were retrieved and assessed for inclusion by both reviewers.
Disagreements were resolved by consensus. Results published only in abstract form were not included because inadequate details were available for risk of bias assessment; we did consider for inclusion those abstracts that had additional information available in the form of slide sets from conference presentations, or those that provided supplemental data from published studies. When the data were sparse, we included studies conducted in countries that are less similar to the United States (e.g., Iran, Taiwan) and studies with smaller sample sizes (e.g., less than 100). See Appendix B for a list of included studies and Appendix C for a list of excluded studies.
Inclusion Criteria
In consultation with the PVA, we formulated 8 key questions. Key questions and inclusion criteria are as follows.
Key Questions
What is the prevalence of common mental health disorders and SUDs (e.g., MDD, PTSD, GAD, alcohol or other drug dependence, and alcohol or other drug abuse) in individuals with SCI?
What are the risks and protective factors for common mental health disorders and SUDs in individuals with SCI?
What is the evidence that common mental health disorders and SUDs influence body functions and structures, activities, participation, health, and quality of life in individuals with SCI?
What is the evidence that the presence and severity of common mental health disorders and SUDs can be reliably and validly assessed in individuals with SCI?
What is the evidence that common mental health disorders and SUDs can be effectively treated in indi- viduals with SCI? What is the comparative effectiveness of treatments for common mental health disorders and SUDs? What are the comparative harms of treatments for common mental health disorders and SUDs?
What is the evidence that mental health disorders and SUD treatment can be delivered to individuals with SCI in ways that are accessible, acceptable, and efficient?
What is the evidence that common mental health dis- orders and SUDs can be prevented in individuals with SCI?
Are there subgroups of patients within the SCI population based on demographics (e.g., gender, race/ ethnicity, age, socioeconomic status, geographic region), level of SCI, duration of injury, comorbidities (e.g., heart disease, chronic obstructive pulmonary disease, other mental health disorder) for which risk or protective factors, specific treatments, or preventive measures differ?
PICOTS
Population
Adults with traumatic SCI
Intervention
- Pharmacotherapy
-
□Antidepressants
-
□Antipsychotics
-
□Antiepileptics
-
□Anxiolytics
-
□Herbal medicines (e.g., S-adenosyl methionine, St. John’s wort)
-
□Cannabis
-
□Other pharmacotherapies
-
□
- Behavioral intervention
-
□Individual counseling
-
□Group counseling
-
□Peer counseling
-
□Cognitive behavioral therapy (CBT)
-
□Attendance at 12-step or similar meetings
-
□Lifestyle counseling
-
□Education
-
□Motivational interviewing
-
□Mindfulness training
-
□Stress management, coping skills training
-
□Rehabilitation
-
□Chinese medicine
-
□Massage
-
□Acupuncture
-
□Yoga, Tai Chi Chuan (or similar martial art)
-
□Physical exercise, physical activity
-
□Healthy eating
-
□
Comparators
Any other included intervention
Placebo
Usual care
Healthy controls
Wait list controls
Outcomes
Mortality
Suicide/Suicidal ideation
- Health
-
□36-Item Short Form Health Survey (SF-36)
-
□Oswestry Disability Index
-
□Other scales or questionnaires
-
□Hospital admissions
-
□Emergency department visits
-
□Sleep
- Duration
- Nocturnal awakenings
-
□
- Quality of Life
-
□Spinal Cord Injury-Quality of Life (SCI-QOL) Anxiety item bank and Depression item bank
-
□Centers for Disease Control and Prevention Health-Related Quality of Life Measure (CDC HRQOL-14)
-
□Other scales or questionnaires
-
□
Return to work/school
Participation in leisure activities
- Change on depression scales
-
□Hamilton Depression Rating Scale
-
□Beck Depression Inventory
-
□Patient Health Questionnaire (PHQ)
-
□Major Depression Inventory
-
□Center for Epidemiologic Studies Depression Scale
-
□Zung Self-Rating Depression Scale
-
□Geriatric Depression Scale
-
□Other scales or questionnaires
-
□
- Change on anxiety scales
-
□Hamilton Anxiety Rating Scale
-
□Beck Anxiety Inventory
-
□Zung Self-Rating Anxiety Scale
-
□Generalized Anxiety Disorder 7-item scale (GAD-7)
-
□Hospital Anxiety and Depression Scale (HADS)
-
□4-Item Patient Health Questionnaire-4 (PHQ-4)
-
□Multidimensional Anxiety Questionnaire
-
□Other scales or questionnaires
-
□
Perception of improvement
Meet criteria for DSM diagnosis (e.g., major depressive disorder, GAD)
- Substance abuse
-
□Drug/alcohol abuse (quantity, frequency, variability, abstinence)
-
□Urine/blood drug screen
-
□Blood alcohol level
-
□
- Perception of improvement
-
□Patient
-
□Clinician
-
□
Timing
Acute injury
Chronic injury
Setting
Inpatient
Outpatient
Community
- Rehabilitation
-
□Physical
-
□Substance abuse
-
□
Study Design
- Key Questions 1-3:
-
□Epidemiological database studies
-
□Cohort studies
-
□Case-control studies
-
□Before and after studies
-
□Systematic reviews
-
□
Key Question 4: Diagnostic accuracy studies
- Key Question 5:
-
□Intervention studies
- Randomized trials
- Cohort studies
- Before and after studies
- Systematic reviews
-
□
- Key Question 6:
-
□Same as Key Question 5
-
□Focus groups
-
□Surveys
-
□Other studies reporting accessibility and acceptability
-
□
- Key Question 7:
-
□Prevention studies
- Randomized trials
- Cohort studies
- Systematic reviews
-
□
Key Question 8: Studies reporting data on a subgroup of individuals with SCI or reporting results stratified by subgroup
Data Abstraction
We abstracted information on population characteristics, interventions, subject enrollment, prevalence, results for efficacy, effectiveness, and harms outcomes for trials, observational studies, and systematic reviews. We recorded intent-to-treat results when reported. Data abstraction was performed by one reviewer and independently checked by a second reviewer. Differences were resolved by consensus.
Validity Assessment (Risk of Bias)
We assessed the internal validity (risk of bias) of randomized trials, observational studies, and systematic reviews by using predefined criteria. These criteria are based on the U.S. Preventive Services Task Force and the National Health Service Centre for Reviews and Dissemination (United Kingdom) criteria19,20; the Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines21; and the Quality in Prognostic Studies (QUIPS) tool.22
We rated the internal validity of each randomized trial on the basis of the methods used for randomization, allocation concealment, blinding, the similarity of compared groups at baseline, loss to follow-up, and the use of intent-to-treat analysis. Observational studies were rated on nonbiased selection, loss to follow-up, pre-specification of outcomes, well-described and adequate ascertainment techniques, statistical analysis of potential confounders, and adequate duration of follow-up. For studies of risk factors, we used the QUIPS tool.22 This tool includes domains on study participants, attrition, measurement of the prognostic factor, statistical adjustment for confounding factors, and appropriate statistical analysis. Systematic reviews were rated on clarity of the review question, specification of inclusion and exclusion criteria, use of multiple databases and search for grey literature, sufficient detail of included studies, adequate assessment of risk of bias of included studies, and adequate summarization of primary studies.
Two reviewers independently assessed the risk of bias of each included study and differences were resolved by consensus. Studies were rated as “low risk of bias,” “medium risk of bias,” or “high risk of bias” from the presence and seriousness of methodological limitations. Risk of bias assessments for included studies are listed in Appendix D.
Studies that had a significant or “fatal” flaw were rated as having a high risk of bias, studies that met all criteria were rated as a low risk of bias, and the
remainder were rated as a medium risk of bias. As the medium risk of bias category is broad, studies with this rating vary in their strengths and weaknesses.
The results of some studies rated as having a medium risk of bias are likely to be valid, while others are only possibly valid. A fatal flaw is reflected by the failure to meet combinations of items from the risk of bias criteria. An example would be a study with high attrition (e.g., 60%) combined with inadequate handling of missing data, or one in which details of randomization and/or allocation concealment were lacking and there were baseline differences in important prognostic characteristics.
Grading the Quality of Evidence
We graded the quality of evidence by using the GRADE approach.23–27 Developed to grade the overall quality of a body of evidence, this approach incorporates 4 key domains: risk of bias (includes study design and aggregate risk of bias), consistency, directness, and precision of the evidence. It also considers other optional domains that may be relevant for some scenarios, such as a dose-response association, plausible confounding that would decrease the observed effect, strength of association (magnitude of effect), and publication bias.
Table 1 describes the grades of evidence that can be assigned. Grades reflect the quality of the body of evidence to answer key questions. Grades do not refer to the general efficacy or effectiveness of treatments, for example. Two reviewers independently assessed each domain for each outcome and differences were resolved by consensus.
Table 1.
Definitions of the Grades of Overall Quality of Evidence
| Grade | Definition |
|---|---|
| High | High confidence that the true effect lies close to that of the estimate of effect. |
| Moderate | Moderate confidence in the effect estimate. The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. |
| Low | Limited confidence in the effect estimate. The true effect may be substantially different from the estimate of the effect. |
| Very Low | Very little confidence in the effect estimate. The true effect is likely to be substantially different from the estimate of effect. |
The quality of the body of evidence was evaluated for each outcome by key question.
Data Synthesis
We constructed in-text tables that show the study characteristics, risk of bias ratings, and results for all included studies. We reviewed studies by using a hierarchy of evidence approach, in which the best evidence is the focus of our synthesis for each question, population, intervention, and outcome addressed. When possible, we pooled study results with meta-analyses by using Stata 14.28
RESULTS
Overview
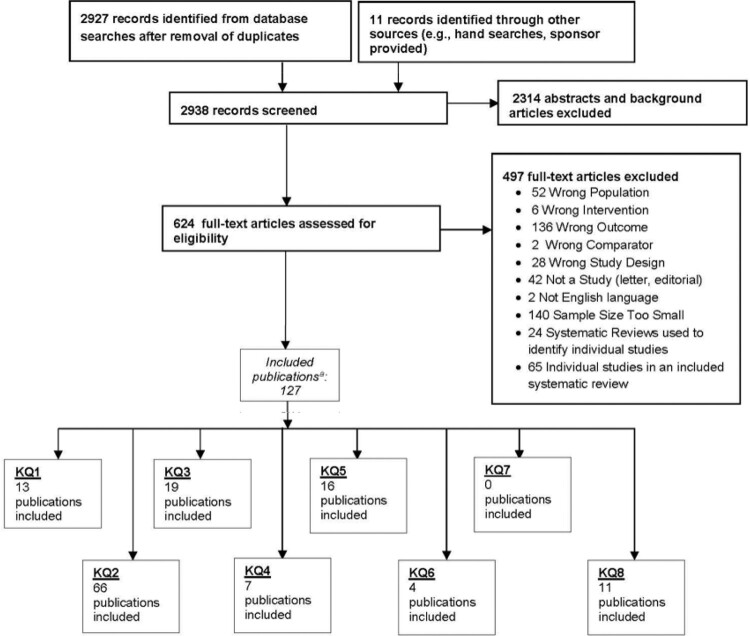
The search and selection of articles are summarized in the literature flow diagram (Figure 1). Database searches resulted in 2,927 potentially relevant articles. After dual review of abstracts and titles, 624 articles were selected for full-text dual review, and 127 studies were determined to meet inclusion criteria and were included in this review.
Figure 1.
Results of literature searches. aPublications may be included in more than one key question (KQ).
Recommendations and Rationales
GENERAL CROSS-CUTTING RECOMMENDATIONS
1. SCREENING, ASSESSMENT, AND TREATMENT
1.1 Integrate mental health professionals with education, training, and experience in spinal cord injury (SCI), as well as in general mental health and substance use disorders (SUDs) within comprehensive inpatient and outpatient SCI rehabilitation programs.
Rationale: Mental health disorders and SUDs are common comorbid conditions in individuals with SCI.10 These conditions can contribute to the overall suffering and disability of individuals with SCI,29,30 adversely affect outcomes,3,13,29–31 increase the costs and reduce the efficiency of rehabilitation,32,33 and lead to premature death.34 It is widely recognized that mental health disorders and SUDs are undertreated generally,35,36 including within SCI rehabilitation. For example, a minority of individuals with SCI are treated for major depression when it is present.13,14 To address mental health treatment disparities, health care organizations are adopting care models wherein screening, assessment, and treatment for mental health disorders and SUDs are integrated into regular health care settings. A good example is the United States Department of Veterans Affairs (VA) Primary Care-Mental Health Integration (PC-MHI) program that has demonstrated increased access to care for mental health disorders and SUDs.37 Integrated mental health and SCI rehabilitation care is already the standard in other countries.38 People with SCI can be affected by multiple interacting comorbid conditions (such as traumatic brain injury,39 substance use disorder, other mental health disorders40, and chronic pain41) as well as distinct adjustment patterns42 and the need to adopt many new SCI-specific health behaviors. Therefore, we recommend that mental health providers have education, training and experience in SCI rehabilitation and in as many of these other areas as possible.43
1.2 Routinely screen all individuals with SCI for mental health disorders, SUDs, and suicide risk as part of inpatient and outpatient rehabilitation.
Rationale: Screening all patients for common comorbid mental health and substance use issues is justified by the prevalence and impact of these conditions in SCI and by the availability of validated brief screening instruments.10,29,30 Routine screening is also critical to the integration of behavioral health care into other medical care and to overcoming undertreatment.11 Widely adopted effective programs for mental health integration such as collaborative care rely on universal screening for target problems.44 This CPG focuses on depression, anxiety, PTSD, SUDs, and suicide because there is evidence that these conditions are prevalent and disabling in individuals with SCI. Each section provides more specific recommendations regarding the timing of screening, screening measures, and responses to positive screening test results.
1.3 Include current symptoms and pre-injury history in screening and assessment of mental health disorders and SUDs.
Rationale: We also recommend that screening include preinjury history of mental health and substance use problems because individuals with SCI have high rates of pre-injury mental health disorders and SUDs, and a history of these disorders is predictive of post-SCI mental health.10 These investigators found that the odds of having a psychological disorder after SCI were 24 times greater if the individual had been treated for a psychological disorder before the SCI.10
1.4 Refer individuals who screen positive for a mental health disorder or SUD to a mental health professional for a diagnostic assessment and initiation of treatment, if indicated.
Rationale: As noted above, mental health disorders and SUDs are undertreated. A national survey showed that only 32.7% of individuals with mental health disorders or SUDs received adequate treatment, and of the individuals with a SUD, only 28.6% received adequate treatment.45 The VA’s PC-MHI program demonstrated that integrated care resulted in increased access to care37 and treatment initiation.46 In primary care, the collaborative care model of mental health integration led to more than double the percentage of patients who experienced at least a 50% reduction in depression severity compared with those who were treated with usual care (45% vs. 19%).47 A study of depression treatment preferences in SCI showed that patients tend to prefer depression treatment provided in medical or rehabilitation settings rather than in specialty mental health settings.18 A randomized controlled trial (RCT) of collaborative care for depression, pain, and physical inactivity in outpatients with SCI resulted in significantly improved pain interference and reduced depression severity, as well as increased treatment satisfaction among those who received collaborative care versus those who received usual care.48
1.5 Use principles of shared decision making to involve individuals with a mental health disorder or SUD in treatment planning.
Rationale: Consistent with the 2001 Institute of Medicine report, Crossing the Quality Chasm,49 clinicians are encouraged to inform their patients regarding treatment options, expected outcomes, and what treatment is available in order to facilitate informed choice and a collaborative decision-making process. These processes are thought to result in better treatment plans and greater patient engagement.49
1.6 Systematically use reliable and valid measures of progress to inform care and adjust treatment for mental health disorders or SUDs.
Rationale: There is a growing body of evidence showing that using repeated outcome assessment and decision rules to adjust treatment improves clinical outcomes, aids recognition of clinical worsening, and highlights residual symptoms that can be a risk factor for relapse.50–52 This approach, called measurement based care (MBC), can also enhance the therapeutic relationship and boost patient adherence and recognition of progress, especially early in treatment.50–52 The Joint Commission recommends the MBC standard (CTS.03.01.09). The VA has invested in MBC by creating a behavioral assessment software program and committing to the adoption of MBC.50
1.7 Refer to follow-up treatment and coordinate care upon discharge or transition to the next phase of care, if indicated.
Rationale: Mental health conditions and SUDs are often chronic, relapsing conditions that require prolonged treatment, relapse prevention efforts, and ongoing monitoring or rescreening.53,54 Consequently, it is vital to plan for continued treatment across transitions in care such as from inpatient rehabilitation to outpatient rehabilitation.
DISORDER-BASED RECOMMENDATIONS
2. ANXIETY DISORDERS
Background
Anxiety is a normal reaction to SCI, but anxiety can become overwhelming and interfere with daily functioning, consistent with anxiety disorders. Anxiety disorders are characterized by anticipation or worry about future threat and are typically accompanied by symptoms such as muscle tension, vigilance, and cautious or avoidant behaviors. These disorders are persistent (typically lasting 6 months or more); out of proportion to reality (taking cultural and contextual factors into account); and interfere with cognitive, emotional, social, and physical functioning.4 In individuals with SCI, anxiety is often studied generically without specifying diagnostic subtypes. Lack of SCI- specific data and the need for brevity have led to the limiting of this review to generalized anxiety disorder (GAD) and Panic Disorder (PD).
High-quality evidence from a meta-analysis of 18 studies shows that the overall weighted prevalence of anxiety symptoms using self-report measures is 27% in individuals with SCI.55 Longitudinal studies indicate that anxiety does not necessarily remit over time. However, longitudinal research specifically designed to detect prognostic subgroups revealed 3 patterns of anxiety over the first 2 years following SCI: stable low anxiety, anxiety improvement, and delayed anxiety.42 Two studies that used diagnostic interviews to identify specific types of anxiety found that the prevalence of GAD was 5%, as was the prevalence of PD.55 In comparison, the 12-month prevalence of GAD and PD in the general population is 3.1% and 2.7%, respectively.56
Anxiety is closely associated with respiratory symptoms in non-SCI populations57 and may be higher in females.58 High-quality evidence from a Chinese population-based cohort study of 3556 persons with SCI indicated that high Injury Severity Scores (ISS> 16) had an almost two-fold higher risk of anxiety than those with an ISS<16.59 Low-quality evidence suggests that participation in team sports as opposed to individual sports is associated with reduced levels of anxiety.60 Low-quality evidence also indicates that lower income and poorer health are associated with greater anxiety61 and that a sense of coherence and acceptance of the SCI appear to be protective against anxiety.62 Very low- quality evidence indicates that threat or loss appraisal, mental disengagement, behavioral disengagement, focus on emotions, and attachment avoidance are risk factors for anxiety.63 Higher anxiety is associated with greater odds of having pain and impaired occupational independence 10 and with lower gains in functional independence (motor scores on the Functional Independence Measure [FIM]).64
2.1 Use a brief, valid measure that has good sensitivity to screen all patients for general anxiety and panic disorder (PDs): (a) early during initial inpatient hospital or rehabilitation stay; (b) as a repeat screen if indicated to assess persistence of symptoms or change in status; (c) at the first post-discharge follow-up point; and (d) at future time points depending on risk stratification factors such as prior positive anxiety screening results or preinjury history of psychological disorder.
Rationale: Most screening measures of anxiety have not been normed for individuals with SCI and may be confounded by sequelae of the injury itself rather than reflecting anxiety (e.g., shortness of breath, sweating, increased blood pressure, and rapid heart rate). A positive screen therefore may or may not lead to an anxiety disorder diagnosis.
Three anxiety screening measures worth considering are the Hospital Anxiety and Depression Scale (HADS),65 the Spinal Cord Injury-Quality of Life (SCI-QOL) Anxiety item bank,66 and the Generalized Anxiety Disorder 7-item scale (GAD-7).66,67 The HADS has been used in numerous studies and has an internal consistency of 0.85.68–70 The 25-item SCI-QOL Anxiety scale (fixed-length version or computer adaptive test version, both adapted from and anchored to the Patient-Reported Outcomes Measurement Information System [PROMIS] v1.0 Anxiety bank and metrics) has an internal consistency of 0.95 and is unidimensional.66 All items have adequate or better model fit statistics, good 1-week test-retest reliability (0.80), and negligible differential item functioning. The 9-item short form has an internal reliability of 0.92. The GAD-7 is a 7-item measure of global anxiety developed for use in primary care.67 It was included in the SCI-QOL Anxiety study, which showed a mean GAD score of 3.86 (standard deviation 4.34) in a sample of 465 individuals with SCI. Correlation of the GAD-7 with the SCI-QOL Anxiety instrument was moderate (0.67). In primary care patients, a score of 10 or more on the GAD-7 has a sensitivity and specificity for GAD of .89 and .82, respectively.71 At a cutoff of 7 or more, the GAD-7 has a sensitivity and specificity of .82 and .75, respectively, for PD.71 The GAD-7 takes 1-2 minutes to administer, the HADS about 5 minutes, and the SCI-QL full 25 item anxiety item about 7-8 minutes.
2.2 Refer patients with positive screen results or those suspected of having an anxiety disorder to a mental health provider for a diagnostic assessment to assess for conditions such as generalized anxiety disorder (GAD) or PD. Rule out the possibility that the symptoms are better explained by the effects of the medical condition, medications, drugs, the environment, or other factors.
Rationale: As noted above, more than 1 in 4 individuals with SCI are affected by significant self-reported anxiety, which is associated with greater pain and poorer functioning. Mental health conditions tend to be undertreated and under recognized in individuals with SCI.13,14 A positive screen may not lead to a DSM-5 anxiety disorder; conversely, the absence of a positive screen does not rule out an ultimate anxiety disorder diagnosis. The person screening should always refer to a mental health provider if significant anxiety is suspected, particularly since screening items are self-report and can be susceptible to denial or minimization. The DSM-5 diagnostic criteria for GAD and PD are presented in Tables 5 and 6 because these 2 conditions are relatively common in SCI. GAD requires excessive anxiety and worry (apprehensive expectation) to have occurred more days than not for at least 6 months about a number of events or activities (such as work or school performance). In individuals for whom anxiety or other symptoms emerge within 3 months after injury, adjustment disorder with anxious mood (or other subtypes) may be a more appropriate diagnosis. In addition, other post-injury stressors such as care transitions or marital stress, as well as financial, housing, and social insecurity, may trigger an adjustment disorder.
Table 9.
DSM-5 Substance Use Disorder Diagnostic Criteria (generic)4
| A problematic pattern of substance use leading to clinically significant impairment or distress is manifested by two or more of the following within a 12-month period: |
| 1. Substance often taken in larger amounts or over a longer period than was intended. |
| 2. A persistent desire or unsuccessful efforts to cut down or control use of substance. |
| 3. A great deal of time is spent in activities necessary to obtain, use, or recover from the substance’s effects. |
| 4. Craving or a strong desire or urge to use the substance. |
| 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. |
| 6. Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by its effects. |
| 7. Important social, occupational, or recreational activities are given up or reduced because of use. |
| 8. Recurrent substance use in situations in which it is physically hazardous. |
| 9. Continued substance use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. |
| 10. Tolerance. |
| A. A need for markedly increased amounts of substance to achieve intoxication or desired effect. |
| B. A markedly diminished effect with continued use of the same amount of a substance. |
| Note: This criterion is not considered to be met for those taking substances solely under appropriate medical supervision. |
| 11. Withdrawal. |
| A. See DSM-5 for description of substance-specific withdrawal syndromes. |
| B. Substance is taken to relieve or avoid withdrawal symptoms. |
| Note: This criterion is not considered to be met for those individuals taking substances solely under appropriate medical supervision. |
| DSM5 severity specifiers: Mild – Two to three criteria met; Moderate – Four to five criteria met; Severe – Six or more criteria met |
Table 10.
Clinical Utility of Substance Use Disorder Screeners Compared with Diagnostic Assessment
| Study | Screening Measure | Cut Point | Sensitivity % | Specificity % | PPV | NPV | Prevalence % | N |
|---|---|---|---|---|---|---|---|---|
| Smith et al., 2009171 | Single-question alcohol screening test | ≥1 | 0.82 | 0.79 | 11.5 | 286 | ||
| Smith et al., 2010172 | Single-question screening test for drug use and drug use disorders (illicit and nonmedical use of prescription drugs) | ≥1 | 1.00 | 0.74 | 11.9 | 286 | ||
| Brown and Rounds, 1995174 | CAGE-AID | ≥1 ≥2 | 0.79, 0.77 | 0.77, 0.85 | ||||
| Brown et al., 2001175 | TICS | 0.79 | 0.78 | 23 | 434, 702 | |||
| Bradley et al., 2007176 | AUDIT-C for men and women | 0.86, 0.73 | 0.89, 0.91 | |||||
| Gryczynski et al., 2017176 | TAPS | 0.80, 0.85, 0.91, 0.85 | 0.92, 0.71, 0.89, 0.93 | 0.60, 0.44, 0.25, 0.49 | 0.97, 0.95, 1.0, 0.99 | 25, 14, 4, 17 | 1,995- 2,000 |
Abbreviations: PPV, positive predictive value; NPV, negative predictive value; CAGE-AID, CAGE Adapted to Include Drugs; TICS, Two-Item Conjoint Screening test; AUDIT-C, Alcohol Use Disorders Identification Test- Consumption; TAPS, Tobacco, Alcohol, Prescription Medication, and Other Substance use.
Other differential diagnoses to be considered for GAD include social anxiety disorder, post-traumatic stress disorder and obsessive-compulsive disorder. Substance/ medication induced anxiety disorder also should be ruled out. The DSM-5 manual lists alcohol, caffeine, cannabis, phencyclidine, hallucinogens, inhalants, opioids, sedative, hypnotic of anxiolytic medications, amphetamine (or other stimulant), and cocaine as substances which can induce anxiety symptoms.4 Differential diagnoses for PD include dizziness, cardiac arrhythmias, hyperthyroidism, asthma, and COPD, although the nature of the association (cause and effect) between PD and these conditions remains unclear.
2.3 To minimize anxiety, support anxious patients with specific and nonspecific therapeutic strategies, provided by all health care professionals (physicians, nurses, therapists, psychologists, social workers, and others) who work with them.
Rationale: Individuals with anxiety may present with unrealistic fears, worries about the future, and avoidance of fear-provoking situations based on their understanding and appraisal of their particular injury and its implications. They may express a heightened need for consistency and control, heavy reliance on staff for reassurance, and even anger when their fears are especially acute. Therefore, it is especially important and sometimes difficult for staff to express core nonspecific relationship factors such as interpersonal warmth, unconditional positive regard, understanding, empathy, and acceptance with these patients72, and to normalize anxiety-based concerns. Some additional anxiety- specific strategies that rehabilitation team members can implement include the following: (1) provide patients with enhanced informational control (e.g., extra details about the nature of rehabilitation, specifically which therapies, procedures, and medications are used and what they do), (2) increase trust through predictability and maintenance of a stable routine (keep schedule, therapists, nurses, and other aspects of care as consistent as possible and give advance warnings regarding anticipated changes to the team or schedule), (3) provide regular positive feedback and affirm all efforts to participate actively in goal setting and review of progress during therapies and training, (4) gradually expose patients to feared situations and prevent their escape from those situations when possible, (5) stay with patients and maintain a calm demeanor during episodes of high anxiety, (6) encouraging patients to actively engage in decision-making where possible such as determining the schedule for administering psychotropic medications and/or deciding between psychotropic vs. psychological approaches to anxiety management, (7) provide conditions for “errorless learning” to enhance confidence, (8) provide community outings prior to discharge to ease discharge anxiety, and (9) provide patients with extra support around transitions such as discharge from inpatient rehabilitation to manage perceived risks and uncertainties that may seem overwhelming (e.g., make sure follow-up appointments are made and occur soon after discharge, provide “warm hand-offs” and co-treatment if possible between inpatient and future outpatient therapists when possible, give patients a way to contact staff who can answer questions or provide referrals for urgent concerns between discharge and initiation of outpatient care).
2.4 Treat GAD, PD, or other clinically significant anxiety by using pharmacological and/or nonpharmacological interventions based on salient clinical considerations and patient preferences.
Rationale: There is minimal evidence of the effectiveness of pharmacological or nonpharmacological treatments for GAD or PD in SCI. For treatment of GAD and PD in the non-SCI population, the effectiveness of serotonergic antidepressants and cognitive behavioral therapy (CBT) are roughly equivalent.73 Therefore, treatment decisions should be based on patient preferences, polypharmacy, medication interactions and potential side effects, and availability from specialized mental health providers.
2.4.1 Consider pharmacological treatment for anxiety, if indicated.
Rationale: There is no evidence for the efficacy of pharmacotherapy for treating anxiety, including GAD or PD, in individuals with SCI. Therefore, we base this recommendation on evidence from other patient populations. For GAD, selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are considered first-line treatments.73 They are judged to have better combined safety and efficacy compared with alternatives such as tricyclic antidepressants and benzodiazepines. The efficacy of different SSRIs and SNRIs is similar.73 Thus, medication choice is based on anticipated side effects, interactions with other medications, and patient treatment history or preferences. Therapeutic dosages of these medications for treating anxiety are similar to those for treating depression. Clinical improvement is expected within 4 weeks on average, but may range from 2 to 6 weeks.
There is a case-report indicating that serotonergic agents may exacerbate spasticity.74 In that case, buspirone (for GAD) and pregabalin are considered second-line treatments and are sometimes used to augment treatment when patients have partially responded to maximum dosages of SSRIs or SNRIs.73 Benzodiazepines to simultaneously treat spasticity and anxiety have fallen out of favor because of the potential for the development of tolerance, dependence and other side effects, and because of the demonstrated effectiveness of other modalities such as baclofen.75 As a result, use of benzodiazepines should be reserved for short-term relief of acute severe anxiety or panic. Beta-blockers and antihistamines have been used for anxiety in other populations, but data do not exist for their use in SCI and potential cardiovascular and anticholinergic side effects, respectively, make their use in SCI problematic.
For PD, SSRIs are considered the first-line medical treatment.76 Other medications such as SNRIs, tricyclic antidepressants, monoamine oxidase inhibitors, and benzodiazepines have evidence of efficacy, but are less preferred because of the strength of evidence, side- effect profiles, and abuse potential.76 Chronic use of benzodiazepines is associated with poorer response to CBT and sustained PRN benzodiazepine use is associated with poorer outcomes generally.76 Prescribers should note the dangers of combining benzodiazepines and opioids and the anticholinergic and sedating effects of tricyclic antidepressants when considering the use of either class of drug for anxiety.76 A check on EKG for QTc prolongation due to frequent polypharmacy before selecting treatment including serotonergic agents should be considered, particularly with citalopram or concurrent use of other medications with pro- arrhythmic risk, such as prochlorperazine or methadone. Serotonin syndrome and the possibility of increased spasms and agitation are risks for polypharmacy as well, particularly when combined with indirectly or directly acting sympathomimetic agents.77
2.4.2 Consider nonpharmacological treatment for anxiety.
Rationale: There is very low-quality evidence that CBT improves symptoms of anxiety in individuals with SCI either directly or indirectly through treatment directed at reducing the impact of chronic pain.78,79 There is also very low-quality evidence that physical activity improves anxiety in individuals with SCI.80 However, there are no studies of SCI treated GAD or PD specifically. Drawing from the broader mental health literature, robust evidence shows that CBT is effective in the treatment of GAD81 and PD76, suggesting that this should be considered a first-line treatment option for patients who are receptive to it and where trained mental health providers are available. For individuals with PD, CBT has the advantage of reducing their risk of relapse compared with individuals treated with medications alone. Outcomes for psychodynamic, supportive, and behavioral therapies for the treatment of GAD are less robust.73 Clinicians should consider using adapted relaxation skills training, depending on the individual’s ability to breathe independently and the level of motor functioning and sensation. Clinicians should also be alert to the possibility of anxiety symptoms leading to avoidance of engagement in social activities and activities outside the home, which could further lead to depression and other negative outcomes. Graded exposure to social and activity situations hierarchically ordered in terms of anxiety symptoms they provoke, can be incorporated into the therapy treatment plan. Modalities like yoga, Taiichi, massage therapy and meditation may be helpful and are currently being offered in the VHA.
3. MAJOR DEPRESSIVE DISORDER (MDD)
Background
Feelings of sadness and depression are normal reactions to stress and loss. However, when these and associated psychological (e.g., anhedonia, guilt, suicidal ideation), cognitive (e.g., poor concentration), and physical (e.g., insomnia, low energy, anorexia) symptoms become severe, prolonged, and impair daily functioning, treatment for a clinically significant depressive disorder is indicated. See Table 7 for DSM-5 criteria for MDD. Data from 21 studies show there is high-quality evidence that the prevalence of depression is 22% globally in individuals with SCI and approximately 28% in U.S. veterans with SCI.82
Table 7.
DSM-5 Major Depressive Disorder Diagnostic Criteria4
| A. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure. Note: Do not include symptoms that are clearly attributable to another medical condition. |
| 1. Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, hopeless) or observation made by others (e.g., appears tearful). (Note: In children and adolescents, can be irritable mood.) |
| 2. Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation). |
| 3. Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month) or decrease or increase in appetite nearly every day. (Note: In children, consider failure to make expected weight gain.) |
| 4. Insomnia or hypersomnia nearly every day. |
| 5. Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down). |
| 6. Fatigue or loss of energy nearly every day. |
| 7. Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick). |
| 8. Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others). |
| 9. Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide. |
| B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| C. The episode is not attributable to the physiological effects of a substance or another medical condition. |
| Note: Criteria A–C represent a major depressive episode. |
| Note: Responses to a significant loss (e.g., bereavement, financial ruin, losses from a natural disaster, a serious medical illness or disability) may include the feelings of intense sadness, rumination about the loss, insomnia, poor appetite, and weight loss noted in Criterion A, which may resemble a depressive episode. Although such symptoms may be understandable or considered appropriate to the loss, the presence of a major depressive episode in addition to the normal response to a significant loss should also be carefully considered. This decision inevitably requires the exercise of clinical judgment based on the individual’s history and the cultural norms for the expression of distress in the context of loss. |
| In distinguishing grief from a major depressive episode (MDE), it is useful to consider that in grief the predominant affect is feelings of emptiness and loss, while in an MDE it is persistent depressed mood and the inability to anticipate happiness or pleasure. The dysphoria in grief is likely to decrease in intensity over days to weeks and occurs in waves, the so-called pangs of grief. These waves tend to be associated with thoughts or reminders of the deceased. The depressed mood of an MDE is more persistent and not tied to specific thoughts or preoccupations. The pain of grief may be accompanied by positive emotions and humor that are uncharacteristic of the pervasive unhappiness and misery characteristic of an MDE. The thought content associated with grief generally features a preoccupation with thoughts and memories of the deceased, rather than the self-critical or pessimistic ruminations seen in an MDE. In grief, self-esteem is generally preserved, whereas in an MDE feelings of worthlessness and self-loathing are common. If self-derogatory ideation is present in grief, it typically involves perceived failings vis-à-vis the deceased (e.g., not visiting frequently enough, not telling the deceased how much he or she was loved). If a bereaved individual thinks about death and dying, such thoughts are generally focused on the deceased and possibly about “joining” the deceased, whereas in an MDE such thoughts are focused on ending one’s own life because of feeling worthless, undeserving of life, or unable to cope with the pain of depression. |
| D. The occurrence of the major depressive episode is not better explained by schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder, or other specified and unspecified schizophrenia spectrum and other psychotic disorders. |
| E. There has never been a manic episode or a hypomanic episode. |
There is high quality evidence that pain and depression are associated in SCI.83 Moderate-quality evidence indicates that risk factors for depression in individuals with SCI include female gender40,61,84,85 and current unemployment or unemployment at injury.84–87 Moderate-quality evidence also suggests that protective factors include increased involvement with life, both socially88,89 and physically,90 and greater time since injury.61,91,92 Other risk factors for depression or increased depression severity include a history of mental illness or substance abuse, current mental illness other than depression, and current abuse of alcohol or illegal substances.88,93–96 One implication of these risk factor studies is that depression often precedes SCI and therefore can be conceptualized and treated as a recurrent mental health condition rather than simply a reaction to SCI.
General prevalence estimates obscure the fact that there are clinically distinct depression subgroup trajectories within the SCI population. Research suggests 3 to 4 trajectory groups: stable low depression, depression improvement, and delayed depression and chronic high depression.42,97 These groups can be identified through repeated screening and can be predicted by individual differences in cognitive appraisals about disability, ways of coping, preinjury mental health history, and grief.42,97
In addition to the direct suffering caused, depression is associated with multiple poor health outcomes in SCI. A systematic review83 and studies published since89,98,99,100–102,91 provide high-quality evidence that depression and pain are positively associated in the SCI population and that the relationship may be bidirectional. In addition, low-quality evidence suggests that depression is a risk factor for comorbid cardiovascular disease, pressure injuries, urinary tract infections, rehospitalization,103 and unemployment.103–105 Very low-quality evidence indicates that depression predicts other health outcomes, participation, and quality of life.106–107
3.1 Screen all individuals with SCI for major depression by using a brief, valid measure that has good sensitivity and specificity: (a) early during the initial inpatient hospital or rehabilitation stay; (b) as a repeat screen if indicated to assess persistence of symptoms or change in status; (c) at the first discharge follow-up point; and (d) at least annually or more frequently, depending on risk stratification factors such as prior positive screening results and chronic pain.
Rationale: Studies in SCI populations have demonstrated that depression screening instruments can be reliably and validly administered via self-report or face-to-face interview. Early depression screening is recommended because it helps predict risk for depression 1-2 years after injury.42,97 The 9-item Patient Health Questionnaire-9 (PHQ-9), Center for Epidemiologic Studies Depression Scale, and Older Adult Health and Mood Questionnaire have been studied most extensively in SCI (see Table 8).108,109
Table 8.
Validity of Depression Screeners Compared with Major Depression Diagnosis
| Study | Screening Measure | Cut Point | Criterion Measure | Sensitivity % | Specificity % | PPV | NPV | Prevalence % | N |
|---|---|---|---|---|---|---|---|---|---|
| Radnitz et al., 1996114 | BDI | ≥18 | SCID DSM-III-R | 83.3 | 90.8 | 50.0* | 98.1* | 9.7 | 124 |
| Tate et al., 1993115 | Zung SDS | ≥55 | DSM-III-R | 86.0 | 67.0 | 42.9* | 93.8* | 23 | 30 |
| Bombardier et al., 2012111 | PHQ-9 | ≥10 | SCID DSM-IV | 100 | 80 | 36.0 | 100 | 10 | 142 |
| Bombardier et al., 2012111 | PHQ-9 | ≥11 | SCID DSM-IV | 100 | 84 | 40.0 | 100 | 10 | 142 |
| Krause et al., 2009116 | OAHMQ | ≥11 | PHQ-9 | 89.7 | 88.8 | 48.4* | 98.6 | 10.7 | 727 |
Abbreviations: PPV, positive predictive value; NPV, negative predictive value; BDI, Beck Depression Inventory; SCID DSM-III-R, Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, 3rd edition, revised; SCID DSM-IV, Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, 4th edition; Zung SDS, Zung Self-Rating Depression Scale; PHQ-9, 9-item Patient Health Questionnaire-9; OAHMQ, Older Adult Health and Mood Questionnaire.
*Oregon Health & Science University calculations.
The SCI-QOL Depression item bank (28 items) is a new measure that was developed specifically for SCI by using the PROMIS metric.110 This measure is unidimensional and has excellent internal consistency (0.95), good 1- to 2-week test-retest reliability (0.83), and adequate or better model fit statistics. A computer adaptive test assessment format is available, as well as a 10-item short form. The SCI-QOL Depression item bank has a correlation of 0.76 with the PHQ-9 and yields greater precision of measurements across scores. Thus far, the SCI-QOL has not been validated against a structured diagnostic interview. The Hospital Depression and Anxiety Scale is used throughout the world but lacks validity data in SCI.
Among the instruments currently available in the public domain, the PHQ-9 is the best-performing measure when tested against an independent DSM diagnosis of MDD in individuals with SCI (see Table 8). The PHQ-9 also has the advantage of widespread clinical use in primary care and other medical settings, ease of use, strong psychometric properties for both screening and treatment monitoring, and items that correspond to those of the DSM-5 criteria for MDD.111,112 Research that uses differential item functioning has shown that somatic symptoms such as insomnia, low energy, and anorexia are not inflated in SCI and should not be discounted when screening for and diagnosing depression, as long as at least one of the cardinal symptoms—depressed mood or anhedonia—is endorsed.113 For greater efficiency, the 2-item Patient Health Questionnaire (PHQ-2) can be used as an initial screen. If neither anhedonia nor depressed mood are endorsed, screening can be discontinued, and if either are endorsed at any level, screening should continue with the remaining PHQ-9 items. PHQ item 9 can be added to cover screening for suicidal ideation. The optimal cutoff for detecting major depression with the PHQ-9 during inpatient rehabilitation is 11 or higher, resulting in 100% sensitivity and 84% specificity.111 The specificity of the screening process can be improved if the screener ensures at least one of the cardinal symptoms is endorsed.
3.2 Refer patients with positive screen results or those suspected of having a depressive disorder to a mental health provider for a diagnostic assessment.
Rationale: Optimally, mental health providers (social workers, psychologists, psychiatrists) will practice within the rehabilitation setting to ensure appropriate continuation of care after discharge. Studies have shown that only a minority of individuals with SCI and depression receive adequate treatment.13,14 For example, Fann et al.13,14 found that only 29% of depressed individuals with SCI received any pharmacotherapy for depression and only 11% received any psychotherapy, with rates of guideline level care at 11% and 6%, respectively. Integrating mental health care into standard medical care (e.g., by implementing a collaborative care model) has been shown to improve outcomes in primary care,47 other chronic diseases,117,118 and SCI care.48
3.3 Follow up on positive screening test results by using a valid diagnostic assessment to confirm conditions such as MDD or adjustment disorder (including sufficient persistence of symptoms and interference with rehabilitation or role functioning) and rule out the possibility that the symptoms are better explained by the effects of the medical condition, medications, drugs, the environment, or other factors.
Rationale: Depression screening with measures such as the PHQ-9 may over-diagnose MDD (i.e., false positives) and therefore require diagnostic interviews and/or reassessment after a short period to ensure the person meets diagnostic criteria. Depressive symptoms may arise in a number of contexts, ranging from stressful situations that may be transient (e.g., transitions in care, anniversaries of the injury, financial or housing difficulty) to chronic stressors such as physical disability, chronic medical illness barriers to participation in meaningful or enjoyable activities. Other contributing factors may include medication side effects, delirium, alcohol or drug use, or a comorbid mental health condition (e.g., bipolar disorder, dementia, schizophrenia). Because of this wide range of etiologies and contributors, a thorough history and diagnostic assessment is essential before deciding on a course of action. The differential diagnosis may include grief related to exposure to losses, demoralization, adjustment disorder, MDD, depression secondary to a medical condition (e.g., traumatic brain injury [TBI], pain, hypothyroidism), and delirium (e.g., due to alcohol withdrawal, corticosteroids). In some cases, somatic symptoms of depression may be better explained by the physical or medical effects of SCI. For example, early morning awakening and fatigue that is worst in the morning are more suggestive of depression, while middle insomnia (associated with turns) and fatigue later in the day may be related to SCI. Weight loss with a normal appetite suggests a medical condition. An important consideration when assessing the significance of depressive symptoms is whether they are impairing the individual’s functioning. When a biological or psychosocial cause or contributor to the symptoms can be identified, it should be addressed.
The use of DSM-5 diagnostic criteria is recommended to guide diagnosis and facilitate shared decision making. Although the presence of MDD typically warrants pharmacological and/or nonpharmacological treatment, adjustment disorder may remit spontaneously or with psychosocial support. However, anyone identified with depressive symptoms (e.g., PHQ-9 score > 5) should be followed to monitor symptom trajectory and determine appropriate management, as adjustment disorders or minor depression can still impair functioning and may evolve into an MDD.
3.4 Support patients with major depression with nonspecific and depression-specific relationship skills, used by all health care professionals (physicians, nurses, therapists, psychologists, social workers, and others) who work with them.
Rationale: Because of the multiple medical and psychosocial issues faced by individuals with medical comorbidity and the complexity (and often fragmentation) of the current health care system, team-based delivery of evidence-based treatment has emerged as a cost-effective approach to depression care.119 A recent study showed that the collaborative care model, a team-based approach to the management of chronic conditions centered around a care manager who is a core member of the medical team, is effective in managing symptoms of depression and pain among individuals with SCI.48 This approach is particularly compelling, given the preference of many individuals with SCI and depression to be treated within the rehabilitation or primary care setting as opposed to a mental health setting or via telephone.18
The Christopher Reeve Foundation has excellent information for members of the team, patients, and their families on understanding depression with SCI (https://www.christopherreeve.org/living-with-paralysis/health/depression). A key point is that team members can contribute to depression if they believe that individuals with SCI will have a low quality of life. Research shows that individuals with SCI have a much higher quality of life than health care providers anticipate.120
Specific strategies that all team members can use to inspire hope include setting small, easily achievable goals to promote self-efficacy and hope,121 engineering high success rates, providing access to activities that the individual finds to be meaningful or pleasant outside of therapies,122 promoting ongoing access to meaningful relationships, focusing on a future with meaning and purpose, and promoting a sense of “the possible,” as well as hope for the moment.123
When team members note depressive symptoms in individuals with SCI that have not been diagnosed, they should encourage and initiate referrals for treatment and tell these individuals and their families that medication and therapy, even for short periods, have been shown to be very effective.124 Evidence-based strategies for promoting family integrity when there is a new disability include maintaining meaningful family traditions during rehabilitation, facilitating open communication among family members, promoting a tone of togetherness, and relieving guilt. Implementing these strategies as a cluster may also promote hope for the moment.
An SCI may be transformative for patients and their families. In health psychology research, positive change and transcendence from challenging life experiences and disability are referred to as posttraumatic growth, benefit finding, stress-related growth, and thriving, all of which have been found to be correlated with a high quality of life.125 Assisting individuals with SCI and their families to experience transformation may also be transformative for the team.124
3.5 Treat major depression by using pharmacological and/or nonpharmacological approaches on the basis of clinical presentation (e.g., comorbid conditions), treatment efficacy, and patient preferences.
Rationale: Research in the mental health treatment literature shows that combined medical and psychotherapeutic treatment is more effective than either treatment alone.126,127 Therefore, for individuals with SCI, clinicians should offer combined medical and psychosocial treatment for major depression whenever possible. Otherwise, treatment recommendations can be based on other factors such as patient preferences because the efficacy of antidepressant medications and psychotherapy for depression are similar.128 A treatment preference study found that 78% to 80% of individuals with SCI and depression were very or somewhat likely to use antidepressants or individual counseling, whereas significantly fewer (48%) were willing to use group counseling.18 Individuals with SCI tend to prefer being treated for depression in rehabilitation or other medical settings rather than being referred to specialized mental health providers. Some guidelines recommend psychotherapy over medications for mild depression.129 Aggressively treating comorbid conditions that may exacerbate depression, such as using pregabalin for chronic neuropathic pain and treating hypothyroidism or obstructive sleep apnea, may also improve depression.130
3.5.1 Consider pharmacological treatments for major depression.
Rationale: One good-quality, randomized, double-blind, placebo-controlled trial conducted in individuals with SCI found that venlafaxine extended release (mean dose 186 mg per day), an SNRI, was effective in treating core symptoms of MDD (depressed mood, anhedonia, guilt, psychomotor agitation, psychomotor retardation, and psychic anxiety) diagnosed an average of 11 years follow- ing SCI.131 Venlafaxine extended release was also found to significantly decrease nociceptive pain and did not increase spasticity.
Because of the paucity of RCTs that use other antide- pressants, evidence-based treatment algorithms cannot be developed. However, from knowledge gained from nonrandomized studies in SCI populations132 and prac- tice guidelines and meta-analyses from other popula- tions,133–135 some general recommendations regarding pharmacotherapy can be made, including the following:
-
-
In general, SSRIs and SNRIs are likely the best- tolerated antidepressant classes. However, fluoxetine, an SSRI with a long half-life, should be used with caution because of case study data showing increased risk of spasticity in individuals with SCI.74 From studies in non-SCI populations, the efficacies of SSRIs and SNRIs are similar.73 Thus, medication choice is based on anticipated side effects, interactions with other medications, and patient treatment history or preferences.
-
-
As with treatment of anxiety, a check on EKG for QTc prolongation due to frequent polypharmacy before selecting treatment including serotonergic agents should be considered, particularly with citalopram or concurrent use of other medications with pro-arrhythmic risk, such as prochlorperazine or methadone. Serotonin syndrome and the possibility of increased spasms and agitation are risks for polypharmacy as well, particularly when combined with indirectly or directly acting sympathomimetic agents.
-
-
Tricyclic antidepressants can cause drowsiness and should be used with caution because of the risk of anticholinergic side effects that may exacerbate common SCI-related symptoms (e.g., hypotension, constipation, urinary retention).
-
-
Other antidepressant options such as bupropion, mirtazapine, vortioxetine, and vilazodone have not been systematically studied in SCI populations.
-
-
Antidepressant dosages should be started at about half the typical starting dose, and dose titration should occur at about half the rate of that typically used in non-medically ill populations.
-
-
Target doses and duration at that dose (i.e., 6 to 8 weeks) required to achieve full therapeutic effect are similar to the non-SCI population.
-
-
Monitoring of depressive symptoms and medication tolerability and efficacy should be performed at least at Health Effectiveness Data Information Set (HEDIS) guideline levels136 and likely more frequently because of the increased potential for adverse effects in medically complex patients.137
-
-Depression that is treatment resistant may require138,139
- Reconsideration of the diagnosis
- Switching to another antidepressant if there is no improvement
- Pharmacological or nonpharmacological (e.g., with psychotherapy) augmentation of the antidepressant
- Electroconvulsive therapy or repetitive transcranial magnetic stimulation
3.5.2 Consider nonpharmacological treatments for major depression.
Rationale: On the basis of 3 systematic reviews,79,140,141 low-quality evidence shows that 6 to 16 sessions of CBT (including coping effectiveness training) improves depression over 6 weeks to 6 months in individuals with SCI. The effect sizes of studies that used individual CBT were much larger than in those that used group CBT. There is very low-quality evidence that an automated, interactive voice response system improved depression at 6 months in a community setting142–144 and no evidence that telephone counseling improved depression.145 In addition, very low-quality evidence suggested that physical activity improved depression.146–151
Given that relatively little research is available on the efficacy of psychosocial treatments for depression in individuals with SCI, we recommend offering such individuals CBT or interpersonal therapy based on the their preferences and the available treatment expertise.152 In addition, a structured physical exercise program (3 times per week consisting of progressive resistance training and aerobic training) may be considered as an adjunct to other therapies.129
4. SUBSTANCE USE DISORDERS
Background
Alcohol and other SUDs are included in this CPG because these conditions are prevalent and associated with poor outcomes in individuals with SCI (see Table 9 for generic diagnostic criteria). Fourteen percent of individuals with SCI report significant alcohol-related problems and 19.3% report heavy drinking.153 Among U.S. veterans, approximately 9% were diagnosed with alcohol-related SUD and 8% had an SUD due to use of illegal drugs.40 Among civilians, the prevalence estimated for other drug use varied widely, from 0% to 14%.154 An estimated 35.3% of individuals with SCI smoke tobacco.155 Large studies of U.S. veterans156 and Canadians157 with SCI found that 55% to 79% were prescribed opioids, and low- quality evidence shows that risk of opioid misuse is higher in individuals with SCI than in those without.158 It is estimated that 35.2% of individuals with SCI use opioids daily159 and that 17.6% to 25.8% self-report significant misuse of pain medications.160,161
Risk factors for SUD include having paraplegia versus tetraplegia, chronic pain, and low income.40,141,162–163 High-quality evidence shows that being at least 65 years old, Latino, and married, as well as having a duration of injury of at least 10 years, are protective against SUD.40,141,162–163 Moderate-quality evidence shows that being older at injury and having higher satisfaction with life, lower education, and employment predicts less alcohol abuse or heavy drinking and that higher satisfaction with life is protective against use of illegal substances.40,141,162–163
Low-quality evidence suggests that alcohol abuse is associated with increased pain and fatigue, poor sleep, lower life satisfaction, and lower likelihood of gainful employment.107,141 Moderate-quality evidence shows that illicit drug use or prescription drug misuse is associated with developing pressure injuries.164 Low- quality evidence also links the use of illegal drugs to pain and lower satisfaction with life.103,141 Tobacco use is associated with poor health and increased mortality in SCI.165,166 Nicotine (2 mg) increases neuropathic pain severity in smokers compared with those receiving a placebo.167 Opioid use is associated with increased risk of upper and lower extremity fractures.168,169 Ominously, 2 studies have found that prescription pain medication use was associated with higher mortality rates in individuals with SCI.34,161
4.1 Screen all patients for common SUDs: (a) Before discharge from inpatient rehabilitation, use a brief, valid measure that has good sensitivity to screen for lifetime use of and problems with alcohol, other (illicit) drugs, tobacco, marijuana, and nonmedical use of prescription medications; and (b) depending on initial screening results and other risk factors, rescreen patients for recent substance use in outpatient rehabilitation or primary care.
Rationale: The CAGE screen95,164,170 and the Alcohol Use Disorders Identification Test-Consumption103,160 have been used in multiple alcohol misuse screening studies. However, substance use screening measures have not been tested for diagnostic validity in individuals with SCI. Therefore, screening recommendations are based on research in other medical populations.
Several single-item screens for harmful alcohol use have been developed. One valid measure asks, “How many times in the past year have you had X or more drinks in a day?” where X = 5 for men and 4 for women.171 Individuals who give an answer that is greater than 0 or respond that they are not sure are considered a positive screen. The test is 82% sensitive and 79% specific for unhealthy alcohol use. Valid single-item drug abuse questions also exist, including one that asks, “How many times in the past year have you used an illegal drug or used a prescription medication for non-medical reasons?”172 At a cutoff of greater than 0, this measure is 100% sensitive and 74% specific for detection of a drug use disorder. One relatively new measure called the Tobacco, Alcohol, Prescription Medication, and Other Substance use covers 4 key drug classes with just 4 questions.173 Information on valid brief screening measures is included in Table 10.
4.2 Refer patients with positive screen results or those suspected of having a SUD to a mental health provider for a diagnostic assessment of SUD criteria.
Rationale: Individuals who screen positive for SUD should undergo a more comprehensive assessment. Standard elements of SUD assessment include determining the type, frequency, and amount of substance use (including route of administration); DSM-5 diagnosis of SUD severity and readiness to change substance use; comorbid psychiatric conditions and relevant medical conditions; and barriers and facilitators to reducing substance use.177 An exception to the recommendation is for persons who obtain screening results indicating risky alcohol use without other signs of alcohol use disorder e.g., AUDIT-C >3 and <8. For thee individuals, brief education on risks of alcohol use tailored to the individual along with recommendations to decrease alcohol to within recommended limits or to abstain are effective.178
4.3 Support patients with SUD with nonspecific and SUD-specific relationship skills, used by all health care professionals (physicians, nurses, therapists, psychologists, social workers, and others) who work with them.
Rationale: Individuals with SUDs can be stigmatized by unscientific beliefs about the cause, course, and treatment of these conditions. Educate the team that SUDs are often chronic, relapsing biopsychosocial conditions that require episodic or continuous care, similar that required for other chronic diseases such as diabetes.179 Conceptualize readiness to change SUD in non-moralistic terms, for example, by using the transtheoretical stages of change model (precontemplation, contemplation, determination, action, maintenance, relapse).180 Reframe relapse as a normal phase in the overall change process and encourage an empathic, nonjudgmental approach to outreach and reengagement in treatment.179 Familiarize rehabilitation staff with common evidence-based psychological and pharmacological treatments for SUDs. Engage staff in educating patients about the adverse health effects of substances, particularly the specific risks of substances in SCI and potential interactions with prescribed medications. Staff can focus on socially reinforcing all abstinence, moderation, and harm reduction efforts, as well as any other positive substance use-related changes made by patients.
4.4 Treat SUDs, within rehabilitation to the extent possible, by using pharmacological, nonpharmacological, and community-based approaches on the basis of clinical presentation (e.g., comorbid conditions), length of stay, treatment efficacy, and patient preferences.
Rationale: SUD treatment involves a spectrum of medical and psychosocial services: screening and referral; early intervention; and outpatient services, intensive outpatient services, inpatient services, and residential services.178 However, only about 1 in 10 individuals with SUD will attend specialized addiction treatment programs.181 Therefore, almost 3 decades ago, the Institute of Medicine called for nonspecialists to deliver briefer, less intensive addiction treatment in settings where individuals with substance use problems are found.182 Treatment delivered in nonspecialist settings can be effective, especially for less severe SUDs. For example, meta-analyses show that brief interventions reduce risky drinking and number of drinks per week in primary care settings.183,184 Brief substance abuse treatment integrated within acute medical/surgical trauma programs also can be effective, especially for individuals with mild-to-moderate SUD severity.185 Brief interventions can function as the initial phase in a stepped-care approach and increase an individual’s readiness for formal treatment.186
Not only are substance abuse problems prevalent within rehabilitation settings, but trauma rehabilitation can also represent a window of opportunity within which individuals with SUDs are more open to change and receptive to treatment.33,187,188 Rehabilitation physicians and psychologists are highly concerned about SUDs in their patients and are increasingly prepared to identify and treat individuals with comorbid SUD.189,190 The American College of Surgeons Committee on Trauma already recommends universal SUD Screening, Brief Intervention, and Referral to Treatment (SBIRT) in trauma services.16 Medically assisted treatment and psychosocial interventions can be delivered within rehabilitation settings. Therefore, we recommend that SUD screening, assessment, and first-line interventions be integrated within SCI rehabilitation programs.
4.5 Use medication-assisted treatment (MAT) for SUDs, including opioid use disorders and alcohol use disorders, when indicated.
Rationale: No literature is available on the efficacy of using MATs for SUDs in individuals with SCI. Therefore, we rely on evidence-based practices in other populations. MATs are used especially for tobacco, alcohol, and opioid use disorders. Numerous CPGs are available online that cover the rationale and implementation of MATs for these disorders. Excellent examples of guidelines include the VA’s Primary Care & Tobacco Cessation Handbook191 and the VA/DoD Clinical Practice Guideline for the Management of Substance Use Disorders.178
For individuals with tobacco use disorder, nicotine replacement therapies are Food and Drug Administration (FDA) approved and include the nicotine patch, gum, lozenge, oral inhaler, and nasal spray.178 These therapies help reduce withdrawal symptoms such as anger and irritability but have little effect on craving. Combining a nicotine patch with another medication such as nicotine gum or lozenges or bupropion significantly increases abstinence rates over monotherapy. Bupropion (Zyban, Wellbutrin) is an FDA-approved dopamine-norepinephrine reuptake-blocking antidepressant that is effective for tobacco cessation. Varenicline (Chantix, Champix) is a nicotine partial agonist that reduces craving and withdrawal and facilitates smoking cessation (close monitoring is advised, as serious psychiatric symptoms such as increased depression [3% to 11%] and suicidal behavior/ideation [6% to 11%] have been reported).192,193 SCI experts recommend combining medical and psychosocial treatments for smoking cessation, using telehealth to follow patients over time, and treating associated conditions such as depression to improve outcomes.194
The VA SUD guideline strongly recommends acamprosate, disulfiram, naltrexone, or topiramate for alcohol use disorder.178 The applicability of these MATs in the context of SCI is to be determined by individual prescribers. Acamprosate works by increasing the GABA-ergic system and decreasing glutamate activity. Acamprosate reduces symptoms of prolonged withdrawal.195 However, acamprosate increases the risk of death by suicide and should be used with caution.195 Disulfiram works by increasing acetaldehyde levels when alcohol is consumed, resulting in a number of uncomfortable adverse affects including flushing, nausea, diaphoresis, palpitations, tachycardia, blurred vision, and hypotension.195 Autonomic dysfunction may be a contraindication to the use of disulfiram after SCI. Naltrexone is an opioid antagonist that blocks endogenous opioids that are released when alcohol is ingested.195 Naltrexone is available in daily pill form or monthly injectable form. Topiramate reduces craving for alcohol by increasing GABA receptor activity, acting as a glutamate receptor antagonist and inhibiting dopamine release.195
The VA SUD guideline recommends buprenorphine and methadone for treatment of opioid use disorder, while extended-release injectable naltrexone as well as methadone and buprenorphine are recommended for maintenance phase treatment.178 Pharmacotherapy is recommended over psychosocial treatments alone on the basis of existing evidence.
Methadone is an opioid agonist that prevents opioid withdrawal, reduces craving, and reduces the effects of illicit opioids.178 Decades of work with methadone maintenance shows that it also improves social, vocational, and other health outcomes. Methadone can be administered, and dose adjusted for pain management during inpatient rehabilitation. Consider baseline electrocardiogram and physical examination for patients at risk for QT prolongation or arrhythmias.178 However, methadone maintenance therapy for addiction is available only through federally regulated outpatient treatment programs. Therefore, careful coordination with methadone treatment programs is necessary to continue therapy and prevent relapse upon discharge from inpatient settings.
Buprenorphine is a partial opioid agonist and comes in the form of a monotherapy or in an agonist/ antagonist form combined with naloxone.178 Buprenorphine treatment is effective in specialty addiction settings, as well as in other clinical settings. It reduces withdrawal symptoms and cravings without producing euphoria or other dangerous side effects such as respiratory suppression. Physicians who complete 8 hours of specialized training can perform buprenorphine induction and maintenance therapy. Buprenorphine induction can occur during inpatient or outpatient rehabilitation, and patients receiving buprenorphine can be followed by providers who have office-based treatment programs.
Naltrexone, an opioid antagonist, is an effective treatment for opioid use disorder only in its long-acting injectable form.178 Naltrexone acts by blocking the effects of opioids. Patients must be opioid free for 7-10 days when naltrexone is started because it is an opioid antagonist and may precipitate withdrawal.195
In addition to the VA/Department of Defense (DoD) guideline, updated guidelines for the use of medications to manage opioid stabilization and withdrawal, tapering, and maintenance are available through the Substance Abuse and Mental Health Services Administration (SAMHSA) website (https://www.samhsa.gov/medication-assisted-treatment). To facilitate access to specialist programs and providers, SAMHSA provides an online methadone treatment program locator (https://dpt2.samhsa.gov/treatment/directory.aspx) and a website dedicated to locating physicians who are certified to provide buprenorphine treatment (https://www.samhsa.gov/medication-assisted-treatment/physician-program-data/treatment-physician-locator). Lastly, consistent with national Veterans Health Administration guidelines, overdose education and naloxone distribution should be provided for anyone who is prescribed opioids.196
4.6 Consider nonpharmacological treatments for SUDs.
Rationale: SCI intervention research is limited to low-quality evidence that multimodal inpatient/ outpatient treatment reduces self-reported alcohol and drug abuse in veterans with SCI.197 Therefore, we rely on the general treatment literature to guide recommendations in this section. A complete review of the SUD treatment literature is beyond the scope of this CPG (see the VA/DoD guideline for a review of the psychosocial treatment literature).178 Instead, we list examples of evidence-based treatment for SUDs that can be implemented within rehabilitation settings.
Moderate-quality evidence shows that brief interventions (1 to 5 sessions and less than 1 hour total time), typically consisting of feedback, information, advice, motivation enhancement, and development of a change plan, reduce alcohol consumption after 1 year in primary care and in patients in emergency departments who are hazardous and harmful drinkers.198 One brief intervention, the SBIRT,199 has numerous online educational modules and videos from which to learn the intervention. Motivational interviewing, often delivered within 1 to 4 sessions, is an evidence-based treatment with demonstrated efficacy across a range of SUDs.200 CBT, contingency management, and relapse prevention are effective treatments across a wide range of SUDs.201,202 Community Reinforcement Approach and Family Training (CRAFT) is a nonconfrontational, positive-reinforcement intervention delivered through concerned family members or friends to motivate individuals with SUDs to engage in addiction treatment. CRAFT is 2 to 3 times more effective than other approaches such as Al-Anon or the Johnson Institute Intervention in overcoming resistance to formal substance abuse treatment.203 For tobacco cessation, interventions lasting 3 minutes or more can have an effect.204 Counseling lasting 4 to 30 minutes can double abstinence rates, while counseling lasting more than 30 minutes can triple abstinence rates. Step-by- step tobacco cessation counseling approaches are described in the VA Primary Care & Tobacco Cessation Handbook191 and there is a companion patient workbook to go along with this program.205
With regard to opioid use disorder, there is little evidence that psychosocial interventions improve outcomes beyond the effects of MAT alone, although treatment dropout is high and keeping patients engaged is critical. The strongest evidence to date comes from a trial that combined MAT and CBT. Abstinence was significantly longer in prescription opioid-dependent patients who were randomized to primary care physician-managed MAT plus CBT than it was in those randomized to physician-managed MAT alone.206 However, there was no abstinence effect of CBT for patients who were heroin dependent. One effectiveness trial showed that a collaborative care intervention consisting of buprenorphine/naloxone plus a 6-session motivation enhancement CBT program significantly improved access to treatment and 6-month abstinence from alcohol or opioids compared with usual primary care.207 The CBT program for that study is available online from the Rand Corporation.208
4.7 Consider referral to community-based SUD treatment programs and self-help resources.
Rationale: Although we recommend SUD treatment delivered as part of standard physical rehabilitation, referral to specialized SUD programs is strongly encouraged for patients who are willing and able to participate in these programs.33,187 Community-based programs are indicated for individuals with more severe SUD, for those who do not fully recover with physical rehabilitation-based treatment, and for those who need maintenance of follow-up treatment for extended periods. Physical rehabilitation providers can use the SAMHSA treatment finder website https://findtreatment.samhsa.gov/ to help patients find appropriate, accessible treatment programs. Unfortunately, in our opinion it remains difficult to find residential SUD treatment programs that can accommodate persons with SCI, especially those with tetraplegia who require assistance with personal care.
Give patients the option of participating in 12-step programs (e.g., Alcoholics Anonymous) as an adjunct to or continuation of SUD treatment. Refer patients, family, and friends to Al-Anon and similar groups for support if using CRAFT is not feasible or not preferred.
5. POSTTRAUMATIC STRESS DISORDER (PTSD) AND ACUTE STRESS DISORDER (ASD)
Background
An SCI often involves exposure to a life-threatening traumatic event. The emotional responses that individuals have to trauma exposure tend to follow 1 of 4 trajectories: resilient, recovering, chronically distressed, and delayed.209,210 Overall, about 5% to 20% of individuals experience symptoms of ASD during the first 3 to 30 days after exposure (see Table 11 for diagnostic criteria).211 ASD was originally conceptualized as a precursor of PTSD, and between 40% and 80% of individuals with ASD go on to develop PTSD.212 Yet, ASD has been found to be a poor predictor of PTSD and most individuals who develop PTSD had not previously met ASD criteria.213 Therefore, ASD is included in the DSM-5 as a severe stress reaction that merits clinical attention of its own.214
Table 11.
DSM-5 Acute Stress Disorder Diagnostic Criteria4
| A. Exposure to actual or threatened death, serious injury, or sexual violence violation in one (or more) of the following ways: |
| 1. Directly experiencing the traumatic event(s). |
| 2. Witnessing, in person, the event(s) as it occurred to others. |
| 3. Learning that the event(s) occurred to a close family member or close friend. Note: In cases of actual or threatened death of a family member or friend, the event(s) must have been violent or accidental. |
| 4. Experiencing repeated or extreme exposure to aversive details of the traumatic event(s) (e.g., first responders collecting human remains, police officers repeatedly exposed to details of child abuse). Does not apply to exposure through electronic media, television, movies, or pictures, unless this exposure is work related. |
| B. Presence of nine (or more) of the following symptoms from any of the five categories of intrusion, negative mood, dissociation, avoidance, and arousal, beginning or worsening after the traumatic event(s) occurred: |
| Intrusion Symptoms |
| 1. Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s). |
| 2. Recurrent distressing dreams in which the content and/or affect of the dream are related to the event(s). |
| 3. Dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event(s) were recurring. (Such reactions may occur on a continuum, with the most extreme expression being a complete loss of awareness of present surroundings.) |
| 4. Intense or prolonged psychological distress or marked physiological reactions in response to internal or external cues that symbolize or resemble an aspect of the traumatic event(s). |
| Negative Mood |
| 5. Persistent inability to experience positive emotions (e.g., inability to experience happiness, satisfaction, or loving feelings). |
| Dissociative Symptoms |
| 6. An altered sense of the reality of one’s surroundings or oneself (e.g., seeing oneself from another’s perspective, being in a daze, time slowing). |
| 7. Inability to remember an important aspect of the traumatic event(s) (typically due to dissociative amnesia and not to other factors such as head injury, alcohol, or drugs). |
| Avoidance Symptoms |
| 8. Efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s). |
| 9. Efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s). |
| Arousal Symptoms |
| 10. Sleep disturbance (e.g., difficulty falling or staying asleep, restless sleep). |
| 11. Irritable behavior and angry outbursts (with little or no provocation), typically expressed as verbal or physical aggression toward people or objects. |
| 12. Hypervigilance. |
| 13. Problems with concentration. |
| 14. Exaggerated startle response. |
| C. Duration of disturbance (symptoms in Criterion B) is 3 days to 1 month after trauma exposure. |
| Note: Symptoms typically begin immediately after the trauma, but persistence for at least 3 days and up to a month is needed to meet disorder criteria. |
| D. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| E. The disturbance is not attributable to the physiological effects of a substance (e.g., medication or alcohol) or another medical condition (e.g., mild traumatic brain injury) and is not better explained by brief psychotic disorder. |
PTSD is viewed as a state of non-recovery from or inability to extinguish the fear experienced during a traumatic event.215 The symptoms of PTSD are captured by 4 symptom clusters: intrusion, avoidance, negative alterations in cognitions and mood, and alterations in arousal and reactivity (see Table 12 for diagnostic criteria). To qualify for a diagnosis of PTSD, an individual must have symptoms for at least 1 month that cause significant distress or impairment.4 Low-quality evidence suggests that the prevalence of PTSD following SCI is 10%, similar to the rate in the general population.3
Table 12.
DSM-5 Posttraumatic Stress Disorder Diagnostic Criteria4
| A. Exposure to actual or threatened death, serious injury, or sexual violence in one (or more) of the following ways: |
| 1. Directly experiencing the traumatic event(s). |
| 2. Witnessing, in person, the event(s) as it occurred to others. |
| 3. Learning that the event(s) occurred to a close family member or close friend. Note: In cases of actual or threatened death of a family member or friend, the event(s) must have been violent or accidental. |
| 4. Experiencing repeated or extreme exposure to aversive details of the traumatic event(s) (e.g., first responders collecting human remains, police officers repeatedly exposed to details of child abuse). Does not apply to exposure through electronic media, television, movies, or pictures, unless this exposure is work related. |
| B. Presence of nine (or more) of the following symptoms from any of the five categories of intrusion, negative mood, dissociation, avoidance, and arousal, beginning or worsening after the traumatic event(s) occurred: |
| Intrusion Symptoms |
| 1. Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s). |
| 2. Recurrent distressing dreams in which the content and/or affect of the dream are related to the event(s). |
| 3. Dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event(s) were recurring. (Such reactions may occur on a continuum, with the most extreme expression being a complete loss of awareness of present surroundings.) |
| 4. Intense or prolonged psychological distress or marked physiological reactions in response to internal or external cues that symbolize or resemble an aspect of the traumatic event(s). |
| 5. Marked physiological reactions to internal or external cues that symbolize or resemble an aspect of the traumatic event(s). |
| C. Persistent avoidance of stimuli associated with the traumatic event(s), beginning after the traumatic event(s) occurred, as evidenced by one or both of the following: |
| 1. Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s). |
| 2. Avoidance of or efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s). |
| D. Negative alterations in cognitions and mood associated with the traumatic event(s), beginning or worsening after the traumatic event(s) occurred, as evidenced by two (or more) of the following: |
| 1. Inability to remember an important aspect of the traumatic event(s) (typically due to dissociative amnesia and not to other factors such as head injury, alcohol, or drugs). |
| 2. Avoidance of or efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s). |
| 3. Persistent, distorted cognitions about the cause or consequences of the traumatic event(s) that lead the individual to blame himself/herself or others. |
| 4. Persistent negative emotional state (e.g., fear, horror, anger, guilt, or shame). |
| 5. Markedly diminished interest or participation in significant activities. |
| 6. Feelings of detachment/estrangement from others. |
| 7. Persistent inability to experience positive emotions (e.g., inability to experience happiness, satisfaction, or loving feelings). |
| E. Marked alterations in arousal and reactivity associated with the traumatic event(s), beginning or worsening after the traumatic event(s) occurred, as evidenced by two (or more) of the following: |
| 1. Irritable behavior and angry outbursts (with little or no provocation) typically expressed as verbal or physical aggression toward people or objects. |
| 2. Reckless or self-destructive behavior. |
| 3. Hypervigilance. |
| 4. Exaggerated startle response. |
| 5. Problems with concentration. |
| 6. Sleep disturbance (e.g., difficulty falling or staying asleep or restless sleep). |
| F. Duration of the disturbance (Criteria B, C, D, and E) is more than 1 month. |
| G. The disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| H. The disturbance is not attributable to the physiological effects of a substance (e.g., medication, alcohol) or another medical condition. |
A recent systematic review of 17 studies concluded that multiple posttraumatic factors had clinically important associations with increased PTSD symptoms: depression, lower levels of acceptance or adjustment, psychological distress, anxiety, negative appraisal, neuroticism, and pain.216,217 Women tended to report more severe PTSD symptoms.216 A large, multisite study (n=1,062) that oversampled Hispanics and non-Hispanic Blacks and was not included in the meta-analysis reported an overall prevalence of PTSD of 24.9% and significantly higher PTSD prevalence among individuals who were Hispanic (31.3%) and non-Hispanic Black (24.7%) than among those who were non-Hispanic White (19.4%).218
There is a dearth of information on the relationship of PTSD to outcomes after SCI. However, PTSD is related to lower social participation.219
5.1 Screen all patients for ASD within 1 month of SCI and for PTSD after the first month. Screening should occur (a) early during initial inpatient hospital or rehabilitation stay; (b) as a repeat screen if indicated to assess persistence of symptoms or change in status; (c) at the first post-discharge follow-up point; and (d) at future time points beyond 6 months, depending on risk stratification factors, such as being a veteran or other trauma-exposed professional or having subthreshold symptom severity on prior screening examinations.
Rationale: On February 1, 2018, the American College of Surgeons Committee on Trauma adopted a resolution to foster screening and early intervention for PTSD in patients with trauma.220 Their recommendations are based on emerging evidence that demonstrates the feasibility of identifying ASD/ PTSD early in trauma survivors221 and on promising research that suggests that early interventions integrated within trauma care can improve outcomes.17 The window of time during which ASD can be treated and PTSD prevented and treated overlaps with the time that individuals with SCI are typically undergoing inpatient or outpatient rehabilitation. Recent research demonstrates the feasibility of identifying PTSD soon after SCI;222 therefore, it seems prudent to have the SCI rehabilitation policies follow the Committee on Trauma recommendations for ACS.
No research has validated ASD or PTSD screens or symptom severity measures in SCI. However, the Injured Trauma Survivor Screen (ITSS), which can be administered acutely after injury and has been shown to predict those most at risk for developing PTSD and/ or depression 6 months after admission to a Level I trauma center following traumatic injury.223 The Purdue Post-Traumatic Stress Disorder Scale-Revised has been used in SCI,224,225 as has the Traumatic Life Events Scale226 and the Clinician-Administered PTSD Scale for DSM 5.82 According to a recent systematic review of PTSD measures, the PTSD Checklist and the Primary Care PTSD Screen are the best-performing screening measures overall (See Table 13).227
Table 13.
PTSD Screening Measures
| Study | Screening Measure | Cut Point | Sensitivity % | Specificity % | PPV | NPV | Prevalence % | N |
|---|---|---|---|---|---|---|---|---|
| Geier et al., 2018228 | Posttraumatic Checklist-5 | ≥30 | 0.94 | 0.94 | 0.80 | 0.98 | 28.3 | 251 |
| Prins et al., 2016229 | Primary Care PTSD Screen | ≥3 | 0.95 | 0.85 | 0.51 | 0.99 |
Abbreviations: PPV, positive predictive value; NPV, negative predictive value.
5.2 Refer patients with positive screen results or those suspected of having ASD or PTSD to a mental health provider for a diagnostic assessment of ASD or PTSD criteria.
Rationale: Individuals who screen positive for ASD or PTSD should undergo a more comprehensive assessment by using the DSM-5 criteria. Optimally, the mental health provider will be practicing within acute trauma care or rehabilitation to improve early detection, intervention, and care coordination, as well as to reduce environmental and other barriers to receipt of services. ASD and PTSD often co-occur with another mental health disorder such as SUD or anxiety disorder. Note that PTSD can be preexisting, caused by the index injury, or caused by peritraumatic events during acute care and delirium. Approximately 25% of individuals with PTSD can have late onset (beyond 6 months).230
5.3 Support patients with PTSD with non-specific and PTSD-specific relationship skills, used by all health care professionals (physicians, nurses, therapists, psychologists, social workers, and others) who work with them.
Rationale: By nature of the disorder, individuals with PTSD may have difficulty trusting others and accepting help. Moreover, many individuals who sustain trauma have a prior history of trauma and/ or adverse childhood experiences. The trauma-informed movement provides resources and strategies that nursing and other non-mental health specialist staff can use to care for patients with historical and recent trauma.231,232 The basic premise of trauma- informed care is that the team ask “What happened to this person?” rather than “What is wrong with this person?” The 5 guiding principles and primary goals for the team are fostering safety, trustworthiness, choice, collaboration, and empowerment.233 These principles highlight the importance of asking, listening, and accepting the patient as a significant intervention for the patient each time this occurs with any team member. Team members can also encourage journaling, reorienting the patient during care, engaging families in caregiving, and using pharmacological interventions.
5.4 Treat ASD and PTSD, within rehabilitation to the extent possible, by using pharmacological and nonpharmacological approaches on the basis of treatment efficacy, clinical presentation (e.g., comorbid conditions), length of stay, and patient preferences.
Rationale: Overall, research on treating ASD and PTSD in SCI is limited. What has been shown appears to be similar to that for the general population. Therefore, we can extrapolate that evidence-based treatments in the general population may be appropriate and effective within the SCI population.
For ASD, trauma-focused psychotherapies are considered first-line treatment, as there is insufficient evidence that medications are effective.234 For PTSD, trauma-focused therapies should be recommended first, unless these therapies are unavailable or not preferred, or if the patient prefers pharmacotherapy.234 The timing of trauma-focused therapy should take into consideration other stressors and the environment.
For example, if a patient is medically unstable or overwhelmed by intense inpatient rehabilitation, it may not be appropriate to initiate treatment. Nevertheless, certain treatment elements may be appropriate, such as education and normalization, acute symptom management, social support, rehabilitation-oriented exposure experiences, and, as needed, cognitive restructuring.234 Psychological debriefing should not be used due to lack of efficacy and evidence of potential harms.234
5.5 Offer patients with ASD brief, evidence-based psychological interventions (trauma-focused CBT) to treat ASD and prevent PTSD within the first 30 days after injury.
Rationale: Several meta-analyses show that early trauma-focused CBT significantly limits subsequent PTSD.235,236 These interventions typically comprise 5 to 6 sessions of education on psychological trauma, anxiety management training, exposure therapy, and cognitive restructuring.214
5.6 Offer patients with PTSD evidence-based, trauma-focused psychological treatment.
Rationale: From the weight of evidence for these treatments, the VA/DoD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder strongly recommends individual, manualized therapies that combine exposure and/or cognitive restructuring with prolonged exposure such as the following: cognitive processing therapy, eye movement desensitization and reprocessing, brief eclectic psychotherapy, narrative exposure, CBT, cognitive therapy, and prolonged exposure therapy.234 Cognitive approaches work to correct maladaptive thought patterns, while behavioral approaches aim to decrease physiological arousal through exposure to triggering stimuli. Trauma-focused CBT typically includes education, cognitive restructuring, and exposure. CBT has been found to reduce the likelihood of developing PTSD.237
5.7 Offer patients with ASD pharmacological treatment if trauma-focused psychotherapies are not available or not preferred.
Rationale: Limited evidence indicates that pharmacotherapy is effective for ASD. The largest pharmacotherapy trial to date found that escitalopram was not effective for early PTSD symptoms.238 A meta- analysis of propranolol concluded that it did not reduce later PTSD symptoms.239 Early administration of hydrocortisone is a promising treatment worthy of additional research.214 Benzodiazepines may be helpful for acute anxiety, agitation, or sleep disturbance in the immediate period following the traumatic event, but prolonged use may be detrimental for adaptation, increasing the risk for development of PTSD.234 In addition, benzodiazepines should be avoided if the patient has a history of substance abuse, and all patients prescribed these medications should be closely monitored for signs of abuse.234 Benzodiazepines should also be limited if patients are prescribed opiates due to risk for respiratory depression.
5.8 Offer patients with PTSD pharmacological treatment if trauma-focused psychotherapies are not available or not preferred.
Rationale: According to the VA/DoD CPG on PTSD, there is strong evidence for the efficacy of sertraline, paroxetine, fluoxetine, or venlafaxine as monotherapy for PTSD in individuals diagnosed with PTSD who choose not to engage in or are unable to access trauma-focused psychotherapy (see VA DoD CPG for details).The VA/DOD determined mirtazapine, prazosin for sleep/nightmares, nefazodone, phenelzine, and the TCAs to have fair evidence in treating PTSD.234 Prazosin is an alpha-1 blocker so there is risk for orthostatic hypotension episodes in patients with SCI; therefore, patients should not be started on this medication if they have unstable low blood pressure.
6. SUICIDE
Background
Routine screening for suicide and systematic suicide risk management in individuals with SCI are supported by the increased reported prevalence of suicidal ideation, suicide attempts, and suicidal deaths in this population. In U.S. studies, individuals with SCI were reported to be 3 to 5 times more likely to die of suicide than were those in the general population,240,241 although data for those injured in the last 2 decades are limited. One study reported a decreasing trend of suicide mortality in SCI cohorts from the 1970s to the 1990s, but the observed suicide rate was still at least 3 times that of the general population even in the later cohorts.241 Suicidal ideation is common after SCI. Over 13% of an SCI cohort reported suicidal ideation in the prior 2 weeks in a cross-sectional analysis, and 7.4% reported a lifetime suicide attempt.242 Studies in non-U.S. populations also found increased suicidal ideation and suicidal attempts in individuals with SCI.243
While SCI in itself increases suicide risk, higher risk of death by suicide after SCI has been associated with certain demographic (non-Hispanic White race) and injury characteristics (paraplegia, T1-S3 level with American Spinal Injury Association Impairment Scale A, B, or C),240 as well as a history of drug abuse or current alcohol abuse.244 Psychotherapy for depression, treatment for bipolar disorder or schizophrenia, or worse PHQ-9 scores are related to increased lifetime suicide attempts.242 Having suicidal ideation in the past year was a risk factor for a suicide attempt in that year.243 Deaths by suicide are significantly higher in individuals whose SCI is caused by an attempted suicide when compared with all other SCI causes.245
6.1 Formally screen individuals with SCI for suicidal ideation by using a brief, standardized, evidence- based screening tool. Screen for suicidal intent and behavior in individuals who report suicidal ideation. Screen (a) early during the initial inpatient hospital or rehabilitation stay, (b) as a repeat screen if indicated to assess persistence of symptoms or change in status, (c) at an early discharge follow-up point, and (d) at least annually or more frequently depending on risk stratification factors.
Rationale: Although suicidal thoughts do not result in suicidal acts in most cases, the incidence of suicide attempts and suicidal deaths in individuals with SCI is significantly higher among those who report suicidal ideation.243 All individuals identified as having suicidal thoughts need further evaluation, including examination of suicidal intent and behavior.
Item 9 of the PHQ-9 (“Over the past two weeks, how often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?”) can be used as an initial screen for suicidal ideation.246 A positive response (i.e., a response other than “not at all”) to Item 9 of the PHQ-9 should generate inquiry about suicidal intent and behavior. The Columbia Suicide Severity Rating Scale (C-SSRS) is a standardized tool that screens for suicidal ideation, quantifies the severity of suicidal ideation and behavior, and further evaluates for suicidal intent or plan if questions for suicidal ideation generate a positive response (See Appendix 1).247 The diagnostic accuracy of suicide risk assessment instruments requires additional study.248 Anyone with a positive screen should undergo more in- depth mental or behavioral health assessment.
Evidence-based guidance on optimal frequency or effectiveness of screening in SCI is lacking. Screening frequency may be influenced by identified risk. More frequent screening may be indicated for individuals with multiple risk factors or previous history of suicide ideation or attempt. The highest reported risk of death by suicide is in the first 6 years post-injury.240,241 The risk subsequently decreases, although the decline does not reach statistical significance until 10 years post-injury and the risk continues to be higher than the general population.241 It is, therefore, prudent to consider routine periodic screening especially during the first 6 to 10 years post-injury.
6.2 Recognize warning signs for suicide and expedite evaluation of such signs by a trained professional. Take immediate follow-up action for anyone displaying direct warning signs for suicide (e.g., suicidal communication, preparation for suicide, and/ or seeking access to or recent use of lethal means).
Rationale: Warning signs for suicide differ from risk factors.249 While risk factors are chronic or long-standing circumstances known to elevate suicide risk, warning signs are the things happening now or very recently that indicate a heightened or imminent risk for suicide. Direct warning signs include suicidal communication (writing or talking about death or suicide); preparations for suicide (suspected when individuals give away possessions, divest themselves of responsibility for dependents, update their will, or indicate in some way that they are “saying goodbye”); or seeking access to lethal means such as guns, medications, or toxins.250 While not always the case, a majority of individuals who attempt or die by suicide give some warning of their intentions.250
Those who talk about suicide must be taken seriously. Individuals who present with direct warning signs must be evaluated expeditiously by a trained professional with expertise in suicide prevention. If an individual seems acutely suicidal, he or she should not be left alone; safety should be ensured while determining the most appropriate treatment setting.
Indirect warning signs may include recently increasing or excessive substance abuse, hopelessness (feels that nothing can be done to improve the situation); burdensomeness (talking about being a burden to others); purposelessness (no reason for living); feeling trapped with no way out; social withdrawal (from family, friends, society); dramatic mood changes; overwhelming guilt, self-blame, or shame; or neglecting bowel, bladder, skin and other aspects of self-care.
Suicidal thoughts or behaviors may be identified in many different clinical settings. Sometimes an individual will approach a primary care provider, nurse, or other member of the rehabilitation team with mental health issues, or an individual may make suicidal statements in the context of despair over health concerns. Other times, a clinician is simply able to detect emotional distress. Regardless of the circumstances, it is important that concerns regarding the individual’s mental health be explored. Those caring for individuals with SCI must be conscientious about recognizing warning signs for suicide and asking directly about thoughts of suicide when indicated. Some providers fear that by asking about suicide, they may prompt the individual to feel suicidal. However, evidence shows that direct assessment of suicidal ideation and intent does not increase the risk for suicide.250 On the other hand, there is a risk of ignoring or missing suicidality if the topic is avoided. Questions should be framed in a direct and nonjudgmental way to enhance the probability of eliciting a truthful response, for example, “Have you had thoughts about taking your own life?”. The question should not be asked as though looking for a “no” answer (“You aren’t thinking of killing yourself, are you?”). Anyone endorsing suicidal thoughts should undergo more in-depth mental or behavioral health assessment.
6.3 Stratify suicide risk on the basis of severity and temporality (acute or chronic) to determine appropri- ate therapeutic interventions and care setting.
6.3.1 Facilitate comprehensive assessment by a trained professional to integrate information about suicidal intent and behavior, warning signs, ability to maintain safety, and factors that impact risk of suicidal acts.
6.3.2 Hospitalize individuals with high acute risk for suicide to maintain their safety, and aggressively target modifiable factors. Directly observe them in a secure environment with limited access to lethal means (e.g., kept away from items with sharp points or edges, cords/tubing, toxic substances).
6.3.3 Address chronic increased risk for suicide in the context of long-term outpatient therapy with established providers, adjusting frequency of contact on the basis of risk level.
Rationale: The stakes when managing suicidal patients are high. Underestimation of risk can lead to inadequate treatment planning and a missed opportunity to prevent death. On the other hand, overestimation of risk leads to unnecessary hospital admissions, with a significant potential for infringement of civil liberties. The seriousness of the risk assessment process can place the goals of safety at odds with patient autonomy and create significant tension between the patient, the clinician, the health care system, and the law. Hence, it is imperative that the evaluation be guided by objectivity and evidence.250
Suicide risk assessment is not absolute. Determination of suicide risk includes gathering information related to the individual’s intent to engage in suicide-related behavior, evaluating factors that elevate or reduce the risk of acting on that intent, and integrating all available information to determine the level of risk and appropriate setting for care.
Although specific protocols for managing suicide risk in individuals with SCI are lacking, guidelines and protocols developed for other at-risk populations can be adapted and applied. For example, the VA has developed established protocols and algorithms to manage different levels of severity and temporality of suicide risk.251 The guidelines are available at https://www.healthquality.va.gov/guidelines/MH/srb/VADoDSuicideRiskFullCPGFinal5088212019.pdf.
Essential features of high acute risk include suicidal ideation with intent to die by suicide and inability to maintain safety independent of external support or help. A plan for suicide, access to lethal means, and recent or ongoing preparatory behaviors and/or suicidal attempts are often present in such situations and contribute to the severity of suicide risk. Hospitalization is typically required for individuals identified as high acute risk for suicide in order to maintain their safety and aggressively target the modifiable factors driving the acute spike in suicide risk.
Observation in a secure environment is needed. Access to lethal means should be eliminated as much as feasible; individuals should be kept away from items with sharp points or edges, cords or tubing, and toxic substances, and medication administration should be supervised. Lack of trained staff to provide SCI-related care (e.g., bowel and bladder management) may sometimes preclude admission to a secure psychiatric unit that would often otherwise be recommended. An alternative would be to observe in as secure an environment as feasible in an inpatient setting where the needed SCI care can be provided, which may sometimes include a 1:1 sitter. Close collaboration between mental health and SCI providers is critical in these situations.
Individuals at intermediate acute risk for suicide may share many of the same clinical features with those at high acute risk, but the essential difference is the perceived ability to maintain safety independent of external support or help. This involves a clinical judgment based on the totality of available clinical data. It is prudent and often preferable to consider hospitalization for these individuals to address suicidal thoughts and/or behaviors. Outpatient management, if considered in these instances, should be intensive, with frequent contact, regular reassessment of suicide risk, and a well-articulated safety plan.
Low acute risk typically involves clinical presentations in which current suicidal intent, a suicide plan, and preparatory behaviors are all absent. There is high collective confidence in the ability of the individual to independently maintain his or her own safety and hospitalization is not indicated. Some of these individuals may still be considered to be at increased chronic risk for suicide on the basis of identified risk factors.
Chronic risk for suicide is appropriately addressed through long-term outpatient therapy with established providers, with the appropriate frequency of contact based on risk level. These individuals require a well-articulated safety plan and routine screening regarding risk for suicide.
6.4 Establish a treatment plan for high-risk individuals that fosters therapeutic alliance with mental health professionals and includes evidence-based suicide-focused psychotherapies.
Rationale: Individuals who are identified as high risk should receive intensive treatment that includes appropriate, evidence-based, suicide-focused psychotherapies, in addition to addressing coexisting psychiatric disorders. Therapeutic techniques that have been used to decrease suicide risk incorporate different combinations of cognitive, emotional, behavioral, and interpersonal approaches, including CBT, problem- solving therapy, dialectical behavioral therapy, and interpersonal therapy. Details of specific psychotherapies can be found elsewhere and are beyond the scope of these guidelines.250,252 The specific type and focus of treatment will vary from patient to patient, based on presentation, patient preference, and practitioner skill and experience in particular techniques.
6.5 Optimize treatment for coexisting mental health and medical conditions that may impact the risk of suicide.
Rationale: Modifiable risk factors should be identified and addressed, including evidence-based treatment for any mental health and medical conditions that may be related to the risk of suicide, including SUDs, MDD, schizophrenia, bipolar disorder, PTSD, TBI, and chronic pain. Major depression should be identified and adequately treated. When prescribing antidepressants for patients at risk for suicide, it is prudent to use medications with a low risk of lethal overdose (e.g., SSRI, SNRI) and to limit the amount of medication dispensed and refilled if medications with a higher risk of lethal overdose are prescribed (e.g., tricyclic antidepressants).
Chronic non-cancer pain has been associated with an elevated risk for suicide,253 although studies specific to SCI-related pain are lacking. After controlling for other psychiatric disorders, the association between pain and suicide remains significant, although it is partially attenuated in consistency with the interpretation that pain increases suicide risk above and beyond the association between pain and depression. High doses of opioids have been associated with increased suicide risk in individuals with non-SCI chronic pain, although that relationship is complex and the effects of confounding factors and of opioid weaning on suicide risk require further investigation.254 Comprehensive evaluation and management of individuals with chronic pain is important, including attention to pain interference with function and life participation, as is awareness of the increased suicide risk in this population and monitoring of suicidal thoughts or plans.255
A strong interplay exists between SUDs, psychiatric illness, psychosocial stressors, and suicide potential.256,257 The integration of psychiatric assessment and care, along with addiction treatment, plays an important role in stabilizing and supporting the individual with a dual diagnosis who has substantial risk for suicide. Assessment of social risk factors such as disruptions in relationships and legal and financial difficulties are important aspects of care.
TBI, including mild TBI, has been associated with suicide risk even after accounting for the relative influence of confounding risk factors,258,259 although the precise mechanisms are unclear. Although the influence of coexisting TBI and SCI on suicide risk has not been reported, it is important to identify TBI in individuals with SCI, to be aware of its potential contribution to suicide risk, and to attend to its sequelae in conjunction with SCI and other health care follow-up.
6.6 Educate the at-risk individual, family, and caregivers on suicide risk and treatment options. Provide information on suicide prevention resources, including crisis lines and services, e.g., the National Suicide Prevention Lifeline number 1-800-273-8255 or 1-800-273-TALK. Provide information to veterans of the U.S. Armed Services about veteran-specific suicide prevention resources including a Veterans Crisis Line accessed by pressing 1 after dialing 1-800- 273-8255, online chatting at VeteransCrisisLine.net, or sending a text to 838255.
Rationale: Effective communication about suicide prevention can help shift knowledge, attitudes, and behaviors by dispelling misconceptions about mental health treatment, raising awareness of available resources, and encouraging help-seeking and healthy behaviors. Suicidal individuals may benefit from education about the way that their emotional responses, thoughts, and behavioral responses to negative life events may be associated with suicidal crises. Family education, with appropriate patient consent, is a recommended practice when providers become aware that an individual is at risk of self- directed violence or is engaging in suicidal behaviors. For individuals who are not considered to be at risk, family member education may unnecessarily induce anxiety within the support system and is typically limited to providing general awareness about resources.
There is a need to increase awareness of the role of crisis lines in providing services and support to individuals in crisis. The National Suicide Prevention Lifeline (1-800- 273-TALK [8255]) is a U.S.-based suicide prevention network of crisis centers that provides a 24/7, toll-free hotline available to anyone in suicidal crisis or emotional distress. This crisis line supports individuals who call for themselves or someone they care about.260 Callers are routed to their nearest crisis center to receive immediate counseling and local mental health referrals. Crisis line brochures and wallet cards are available at www.suicidepreventionlifeline.org. For veterans and active duty service members, the VA has partnered with the National Suicide Prevention Lifeline to provide a veteran-specific crisis line that can be accessed by pressing 1 after dialing 1-800-273-TALK, chatting online at VeteransCrisisLine.net, or sending a text to 838255.
6.7 Establish a safety plan for individuals considered to be at high risk for suicide. Limit access to lethal means (e.g., restricting access to firearms, use of gun locks, limited medication supply).
Rationale: Discussion between clinicians and at-risk individuals for developing strategies and skills that support the individual’s ability to avoid acting on thoughts of suicide is an important component of suicide prevention. Putting this process in writing for the anticipation of a suicidal crisis and how to manage it constitutes a patient’s safety plan or crisis response plan. These plans are tailored to the individual on the basis of his or her specific warning signs and past effective coping strategies. Components of a safety plan include recognizing warning signs of an impending suicidal crisis, using internal coping strategies, using social contacts and social settings as a means of distraction from suicidal thoughts, using family members or friends to help resolve the crisis, contacting mental health professionals or agencies, and restricting access to lethal means. The plan should be included in the medical record, and the patient should have received a copy of the plan. It should be shared with family members and others if the patient consents. Safety plans should be updated to remain relevant during changes in clinical state and transitions of care. Safety planning is a provider-patient collaborative process, not a “no-harm” contract. There is no empirical evidence for the use of “no-harm” or “no-suicide” contracts, and a safety plan is a preferred strategy for preventing suicide.261
Firearms are the most common means of suicidal deaths in the United States, both in the general population and in individuals with SCI. Gunshots accounted for 50% of all suicides among individuals with SCI in one study, followed by overdose/poisoning at 16% and cutting, hanging/suffocation, drowning, and fall from heights as other reported means.240
Professionals who provide health care and other services to individuals at risk for suicide are in a unique position to ask about the availability of lethal means and work with these individuals and their support networks to reduce access. Means restriction and means safety counseling are important aspects of suicide prevention, especially given the impulsive nature of many suicide attempts.262 Lethal means safety includes, among other things, restriction of access to firearms and ammunition, safer prescribing and dispensing of medications to prevent intentional overdoses, and modifying the environment of care in clinical settings to prevent suicide attempts by falls, strangulation or hanging. Practices to reduce risk of suicide by medication overdose include prescription of drugs with a low risk of lethal overdose when feasible and limiting the amount of medication dispensed and refilled when prescribing drugs with a higher risk of lethal overdose, such as opioids, tricyclic antidepressants, benzodiazepines, and other sedative- hypnotics. Naloxone prescription should be considered for those at risk for opioid overdose.184 Compared with those who store their firearms unlocked or loaded, individuals who store their firearms locked and/or unloaded are less likely to die from suicide by firearms, and so making gunlocks available and encouraging their use could be an important safety measure for those who have firearms at home.262,263
6.8 Augment personal and environmental protective factors that may mitigate suicide risk. Enhance coping skills.
Rationale: Protective factors are those things that have the potential to prevent individuals from attempting suicide, in other words, their identified reasons for living. Strengthening existing protective factors can help offset suicide risk by promoting physical, mental, emotional, and spiritual wellness. Research on the effect of individual protective factors on suicide risk is sparse.250 However, social interaction and connectedness with the community have been associated with lower suicide risk,264,265 and connectedness to others, including family members, co-workers, community organizations, and social institutions, has been identified as an important protective factor.266,267 These positive relationships can help increase an individual’s sense of belonging, foster a sense of personal worth, and provide access to sources of support. Advancements in physical and societal accessibility, with improved social participation, community integration, and social support for individuals with SCI, have been suggested as protective factors that have possibly contributed to the reported decline in suicide rates between the 1970s and 1990s in the United States.241
Engagement in pleasurable and rewarding activities, such as adaptive sports or other enjoyable avocational or vocational pursuits; cultural, spiritual, and religious beliefs about the meaning and value of life; and access to supportive health care relationships that foster engagement in one’s own wellness are all examples of potential protective factors. Chaplains, pastors, benefits counselors, recreational therapists, vocational rehabilitation specialists, and peer support groups, as well as other members of the rehabilitation team and health care support network, may be valuable in bolstering protective factors.
Development of coping skills is an important component of suicide risk mitigation. Training in skills, attitudes, and behaviors may allow individuals with SCI to interact more appropriately with their environment, thereby lessening the impact of modifiable risk factors for suicide. For example, replacing maladaptive coping skills with more adaptive coping skills may have a direct impact on the quality of relationships with significant others. Skills such as anger management, conflict resolution, stress and anxiety management, financial planning, career guidance, assertiveness, relationship building, relaxation, self-care, communication, and mindfulness can potentially help individuals better cope with life challenges, improve their quality of life, and decrease suicide risk.
Table 5.
DSM-5 Generalized Anxiety Disorder Diagnostic Criteria4
| A. Excessive anxiety and worry (apprehensive expectation), occurring more days than not for at least 6 months, about a number of events or activities (such as work or school performance). |
| B. The individual finds it difficult to control the worry. |
| C. The anxiety and worry are associated with three (or more) of the following six symptoms (with at least some ymptoms having been present for more days than not for the past 6 months): |
| 1. Restlessness or feeling keyed up or on edge. |
| 2. Being easily fatigued. |
| 3. Difficulty concentrating or mind going blank. |
| 4. Irritability. |
| 5. Muscle tension. |
| 6. Sleep disturbance (difficulty falling or staying asleep, or restless, unsatisfying sleep). |
| D. The anxiety, worry, or physical symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| E. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition (e.g., hyperthyroidism). |
F. The disturbance is not better explained by another mental disorder (e.g.:
|
Table 6.
DSM-5 Panic Disorder Diagnostic Criteria4
| A. Recurrent unexpected panic attacks. A panic attack is an abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which time four (or more) of the following symptoms occur: Note: The abrupt surge can occur from a calm state or an anxious state. |
| 1. Palpitations, pounding heart, or accelerated heart rate. |
| 2. Sweating. |
| 3. Trembling or shaking. |
| 4. Sensations of shortness of breath or smothering. |
| 5. Feelings of choking. |
| 6. Chest pain or discomfort. |
| 7. Nausea or abdominal distress. |
| 8. Feeling dizzy, unsteady, light-headed, or faint. |
| 9. Chills or heat sensations. |
| 10. Paresthesias (numbness or tingling sensations). |
| 11. Derealization (feelings of unreality) or depersonalization (being detached from oneself). |
| 12. Fear of losing control or “going crazy.” |
| 13. Fear of dying. |
| Note: Culture-specific symptoms (e.g., tinnitus, neck soreness, headache, uncontrollable screaming or crying) may be seen. Such symptoms should not count as one of the four required symptoms. |
| B. At least one of the attacks has been followed by 1 month (or more) of one or both of the following: |
| 1. Persistent concern or worry about additional panic attacks or their consequences (e.g., losing control, having a heart attack, “going crazy”). |
| 2. A significant maladaptive change in behavior related to the attacks (e.g., behaviors designed to avoid having panic attacks, such as avoidance of exercise or unfamiliar situations). |
| C. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition (e.g., hyperthyroidism, cardiopulmonary disorders). |
| D. The disturbance is not better explained by another mental disorder (e.g., |
|
|
|
|
|
Future Research
Overarching
Further research, such as trajectory and risk factor studies,42,97 is needed to identify individuals soon after SCI who are most likely to benefit from heightened surveillance or early interventions.
We need studies that examine ways to improve the transition from inpatient to outpatient settings and on how transition strategies can prevent and mitigate mental health problems.
We need comparative effectiveness studies that help health care providers and patients choose the best treatment for each individual.
We need studies that compare the effectiveness of traditional mental health service delivery (e.g., screen and refer) to integrated forms of mental health care within rehabilitation.
In addition to the efficacy studies mentioned below, we need effectiveness and implementation studies of patient-centered, multifaceted, stepped-care approaches that focus the limited mental health resources on the individual’s level of need.
Research is needed on the efficacy and effectiveness of alternative mental health treatment delivery models such as telephone, videoconference, web-based, and app-based interventions.
Because mental health disorders and SUDs tend to be chronic relapsing conditions, the effectiveness of patient- based relapse prevention (e.g., education, skills training) and system-based relapse prevention (e.g., ongoing continuous or intermittent care) merits research.
Because mental health disorders, especially depression, are associated with increased rehabilitation costs,32 research is needed on the effect of mental health and SUD treatment on the overall cost and effectiveness of SCI rehabilitation.
Research is needed on use of peer-led interventions for mental health disorders, SUD, and suicide risk.
Anxiety
There are no studies with adequate sample sizes that have examined the criterion validity of anxiety measures in SCI. Strong, valid assessments normed within the SCI population is the first step in identifying individuals at risk and in measuring benefits from treatment.
No evidence has been shown for the efficacy of pharmacotherapy for treating anxiety, including GAD or PD, in individuals with SCI. Further research is needed to test the efficacy of medications in treating anxiety in individuals with SCI, as well as comparison trials for pharmacotherapy versus psychotherapies in this population.
Validated psychotherapies have demonstrated limited benefit in this population; however, many known treatments for anxiety have not yet been investigated for individuals with SCI and among the treatments that have been investigated, the sample size has been small.
Depression
Specific SCI depression screens (i.e., SCI-QOL) should be validated against a structured diagnostic interview.
RCTs that use antidepressants other than venlafaxine will help develop evidence-based treatment algorithms for individuals with SCI and MDD.
Further research is needed on the efficacy of evidence- based psychosocial treatments for depression, including physical activity or exercise interventions,
in individuals with SCI.
Studies of combined treatments and alternative treatments are needed, such as transcranial magnetic stimulation and ketamine for treatment- resistant depression.
Substance Use Disorder
Substance use screening measures have not been tested for diagnostic validity in individuals with SCI.
Studies of the acceptability, feasibility, efficacy, and effectiveness of integrated SUD treatment during inpatient or outpatient rehabilitation for individuals with SCI are warranted.
Research on the efficacy of psychosocial treatments and MATs alone and in combination for SUD in individuals with SCI is warranted.
Research is needed on the effects of nonopioid and nonpharmacological pain interventions on opioid use, opioid addiction, and other mental health outcomes.
PTSD/ASD
Little information is available on the association of PTSD with outcomes after SCI, including factors that promote posttraumatic development. Long-term follow-up is needed to determine the effects of trauma on physical recovery following SCI.
There is no research that validates ASD or PTSD screens or symptom severity measures in SCI. This is a needed area of research, considering that many individuals acquire SCI secondary to a traumatic event.
Treatment studies are needed for evidence-based pharmacotherapy and psychotherapy for ASD and PTSD in individuals with SCI.
Suicide
Evidence-based guidance on the optimal frequency or effectiveness of screening for individuals with SCI is lacking. Further research that supports screening protocols is warranted.
Pain has been demonstrated to be a strong indicator for suicidal ideation in other populations; however, studies specific to psychological effects and suicide risk associated with SCI-related pain are lacking.
Research is needed on measures to mitigate suicide risk following SCI, including the role and effectiveness of efforts to augment protective factors.
Supplementary Material
Appendices.
Appendix 1. Substance Use Disorder Screening Measures
Single-question alcohol screening test: “How many times in the past year have you had X or more drinks in a day?”, where X is 5 for men and 4 for women, and a response of ≥1 is considered positive. Subjects responding negatively to the pre-screening question were still asked the single screening question. If asked to clarify, the research associate provided definitions of a standard drink (12 ounces of beer, 5 ounces of wine, or 1.5 ounces of 80 proof spirits).
Single-question screening test for drug use and drug use disorders: “How many times in the past year have you used an illegal drug or used a prescription medication for non-medical reasons?” A response of at least 1 time was considered positive for drug use. If asked to clarify the meaning of “non-medical reasons,” the research associate added “for instance because of the experience or feeling it caused.”
CAGE-AID Questionnaire: “When thinking about drug use, include illegal drug use and the use of prescription drug use other than prescribed.”
1. Have you ever felt that you ought to cut down on your drinking or drug use?
YES NO
2. Have people annoyed you by criticizing your drinking or drug use?
YES NO
3. Have you ever felt bad or guilty about your drinking or drug use?
YES NO
4. Have you ever had a drink or used drugs first thing in the morning to steady your nerves or to get rid of a hangover?
YES NO
Two-Item Conjoint Screening (TICS) test: “In the last year, have you ever drank or used drugs more than you meant to?” and “Have you felt you wanted or needed to cut down on your drinking or drug use in the last year?” (yes to at least one question is considered positive).
TOBACCO, ALCOHOL, PRESCRIPTION MEDICATIONS, AND OTHER SUBSTANCES (TAPS) TOOL
| Daily or almost daily | Weekly | Monthly | Less than monthly | Never | |
|---|---|---|---|---|---|
| In the PAST 12 MONTHS, how often have you used any tobacco product (for example, cigarettes, e-cigarettes, cigars, pipes, or smokeless tobacco)? | |||||
| In the PAST 12 MONTHS, how often have you had (5 or more drinks for men; 4 or more drinks for women) containing alcohol in one day? One standard drink is about 1 small glass of wine (5 oz), 1 beer (12 oz), or 1 single shot of liquor. | |||||
| In the PAST 12 MONTHS, how often have you used any drugs including marijuana, cocaine or crack, heroin, methamphetamine (crystal meth), hallucinogens, ecstasy/MDMA? | |||||
| In the PAST 12 MONTHS, how often have you used any prescrip- tion medications just for the feeling, more than prescribed, or that were not prescribed for you? Prescription medications that may be used this way include opiate pain relievers (for example, OxyContin, Vicodin, Percocet, methadone), medications for anxiety or sleeping (for example, Xanax, Ativan, Klonopin), or medications for ADHD (for example, Adderall or Ritalin). |
Appendix 2. PTSD Screening Measures
Primary Care PTSD Screen
| Sometimes things happen to people that are unusually or especially frightening, horrible, or traumatic (fire, abuse, earthquake, flood, war, death) Have you ever experienced this kind of event? If no, stop If yes, proceed to ask, “In the past month have you … ” |
Yes | No |
| 1. had nightmares about the event(s) or thought about the event(s) when you did not want to? | Yes | No |
| 2. tried hard not to think about the event(s) or went out of your way to avoid situations that reminded you of the event(s)? | Yes | No |
| 3. been constantly on guard, watchful, or easily startled? | Yes | No |
| 4. felt numb or detached from people, activities, or your surroundings? | Yes | No |
| 5. felt guilty or unable to stop blaming yourself or others for the event(s) or any problems the event(s) may have caused? | Yes | No |
INSTRUCTIONS: In the following table is a list of problems that people sometimes have in response to a very stressful experience. Please read each problem carefully and then circle one of the numbers to the right to indicate how much you have been bothered by the problem in the past month.

The Posttraumatic Checklist-5 can determine a provisional diagnosis in 2 ways:
Treating each item rated as 2 = “Moderately” or higher as a symptom endorsed, and then following the DSM-5 diagnostic rule, which requires at least 1 Criterion B item (Questions 1-5), 1 Criterion C item (Questions 6-7), 2 Criterion D items (Questions 8-14), and 2 Criterion E items (Questions 15-20).
Summing all 20 items (range 0-80) and using a cut-point score of 33 appears to be reasonable based on current psychometric work. However, when choosing a cut-point score, it is essential to consider the goals of the assessment and the population being assessed. The lower the cut-point score, the more lenient the criteria for inclusion, increasing the possible number of false positives. The higher the cut-point score, the more stringent the inclusion criteria and the more potential for false negatives.
If a patient meets a provisional diagnosis by using either of the methods above, he or she needs further assessment (e.g., Clinician-Administered PTSD Scale for DSM 5) to confirm a diagnosis of PTSD.
PCL-5 (14 August 2013) National Center for PTSD
| In the past months, how much were you bothered by: | Not at all | A little bit | Moderately | Quite a bit | Extremely |
|---|---|---|---|---|---|
| 1. Repeated, disturbing, and unwanted memories of the stressful experience? | 0 | 1 | 2 | 3 | 4 |
| 2. Repeated, disturbing dreams of the stressful experience? | 0 | 1 | 2 | 3 | 4 |
| 3. Suddenly feeling or acting as if the stressful experience was actually happening again (as if you were back reliving it)? | 0 | 1 | 2 | 3 | 4 |
| 4. Feeling very upset when someone reminded you of the stressful experience? | 0 | 1 | 2 | 3 | 4 |
| 5. Having strong physical reactions to when someone reminded you of the stressful experience (for example, heart pounding, trouble breathing, sweating)? | 0 | 1 | 2 | 3 | 4 |
| 6. Avoiding memories, thoughts, or feelings related to the stressful experience? | 0 | 1 | 2 | 3 | 4 |
| 7. Avoiding external reminders of the stressful experience (for example, people, places, conversations, activities, objects, or situations)? | 0 | 1 | 2 | 3 | 4 |
| 8. Trouble remembering important parts of the stressful experience? | 0 | 1 | 2 | 3 | 4 |
| 9. Having stong negative beliefs about yourself, other people, or the world (for example, having thoughts such as: I am bad, there is something seriously wrong with me, no one can be trusted, the world is completely dangerous)? | 0 | 1 | 2 | 3 | 4 |
| 10. Blaming yourself or someone else for the stressful experience or what happened afte it? | 0 | 1 | 2 | 3 | 4 |
| 11. Having strong negative feelings such as fear, horror, anger, guilt, or shame? | 0 | 1 | 2 | 3 | 4 |
| 12. Loss of interest in activities that you used to enjoy? | 0 | 1 | 2 | 3 | 4 |
| 13. Feeling distant or cut off from people? | 0 | 1 | 2 | 3 | 4 |
| 14. Trouble experiencing positive feelings (for example, being unable to feel happiness or have loving feelings for people close to you)? | 0 | 1 | 2 | 3 | 4 |
| 15. Irritable behavior, angry outbursts, or acting aggressively? | 0 | 1 | 2 | 3 | 4 |
| 16. Taking too many risks or doing things that could cause you harm? | 0 | 1 | 2 | 3 | 4 |
| 17. Being “superalert” or watchful, on guard? | 0 | 1 | 2 | 3 | 4 |
| 18. Feeling jumpy or easily startled? | 0 | 1 | 2 | 3 | 4 |
| 19. Having diffuculty concentrating? | 0 | 1 | 2 | 3 | 4 |
| 20. Trouble falling or staying asleep? | 0 | 1 | 2 | 3 | 4 |
Appendix 3. Depression Screening Measures
Patient Health Questionnaire-9
Over the last two weeks, how often have you been bothered by any of the following problems?
| Not at all | Several days | More than half the days | Nearly every day | |
|---|---|---|---|---|
| 1. Little interest or pleasure in doing things | 0 | 1 | 2 | 3 |
| 2. Feeling down, depressed or hopeless | 0 | 1 | 2 | 3 |
| 3. Trouble falling or staying asleep, or sleeping too much | 0 | 1 | 2 | 3 |
| 4. Feeling tired or having little energy | 0 | 1 | 2 | 3 |
| 5. Poor appetite or overeating | 0 | 1 | 2 | 3 |
| 6. Feeling bad about yourself – or that you are a failure or have let yourself or your family down | 0 | 1 | 2 | 3 |
| 7. Trouble concentrating on things, such as reading the newspaper or watching television | 0 | 1 | 2 | 3 |
| 8. Moving or speaking so slowly that other people could have noticed? Or the opposite – being so fidgety or restless that you have been moving around a lot more than usual | 0 | 1 | 2 | 3 |
| 9. Thoughts that you would be better off dead or of hurting yourself in some way | 0 | 1 | 2 | 3 |
| PHQ9 Total Score |
Developed by Drs Robert L. Spitzer, Janet B. W. Williams, Kurt Kroenke, and colleagues, with an educational grant from Pfizer Inc.
Appendix 4. Anxiety Disorder Screening Measures
Generalized Anxiety Disorder-7 (GAD-7)
Over the last two weeks, how often have you been bothered by any of the following problems?
| Not at all | Several days | More than half the days | Nearly every day | |
|---|---|---|---|---|
| 1. Feeling nervous, anxious or on edge | 0 | 1 | 2 | 3 |
| 2. Not being able to stop or control worrying | 0 | 1 | 2 | 3 |
| 3. Worrying too much about different things | 0 | 1 | 2 | 3 |
| 4. Trouble relaxing | 0 | 1 | 2 | 3 |
| 5. Being so restless that it is hard to sit still | 0 | 1 | 2 | 3 |
| 6. Becoming easily annoyed or irritable | 0 | 1 | 2 | 3 |
| 7. Feeling afraid as if something awful might happen | 0 | 1 | 2 | 3 |
| GAD7 Total Score | ||||
Developed by Drs Robert L. Spitzer, Janet B. W. Williams, Kurt Kroenke, and colleagues, with an educational grant from Pfizer Inc.
Appendix 5. Suicide Severity Screening Measures
COLUMBIA-SUICIDE SEVERITY RATING SCALE-SCREEN VERSION
 |
For inquiries and training information contact: Kelly Posner, Ph. D. New York State Psychiatric Institute, 1051 Riverside Drive, New York, New York, 10032; posnerk@nyspi.columbia.edu © 2008 The Research Foundation for Mental Hygiene, Inc.
Appendix 6: Panel Conflict of Interest Statement
CONSORTIUM FOR SPINAL CORD MEDICINE
Steering Committee Member and Guideline Development Panel Member please read the following policies on Conflicts of Interest and Confidentiality and sign below to indicate acceptance.
POLICY ON CONFLICTS OF INTEREST
The Consortium for Spinal Cord Medicine (hereafter referred to as “the Consortium”) is a collaboration of professional and consumer organizations funded and administered through Paralyzed Veterans of America (hereafter referred to as “PVA”). PVA wants to ensure that regular business of the Consortium’s Steering Committee and the guideline development process are free from conflicts of interest. PVA recognizes that those on the Steering Committee and Guidelines Development Panels are involved in a variety of organizations and projects, and may hold financial investments which might create actual or potential conflicts of interest or the appearance of a conflict (each a “conflict” or “conflict of interest”).
To achieve that result, the following policy is adopted:
1. Applicability. This Policy applies to the Consortium’s Steering Committee Members, including the Chair and Vice-Chair, in addition to those members on the Guideline Development Panels (collectively, “Covered Persons”).
2. Term. This agreement is effective for the term the Covered Person is a member of the Steering Committee and/or a Guideline Development Panel, notwithstanding how active or passive a role he or she may play as a member of the Steering Committee or a Guideline Development Panel.
3. Determining the Existence of a Conflict. The guidelines set forth below shall be used to determine the existence of a conflict. The guidelines are meant to be illustrative and not exclusive; a conflict may exist even though the situation in question is not included below. Each Covered Person bears the personal responsibility for initially determining if a conflict of interest exists with respect to such Covered Person. If a Covered Person has any questions regarding the existence of a conflict, such Covered Person should promptly contact the Steering Committee Chair.
4. Guidelines for Determining Existence of Conflict. A conflict may exist if the Covered Person is unduly influenced by others (i.e. his/her spouse, parent, child, or other individual with whom such Covered Person has a close personal, business or professional relationship (including persons with whom such Covered Person is a partner, shareholder in a closely held corporation, coauthor or other close professional coworker or colleague) to the detriment of and against the mission of the Consortium, the Steering Committee, the Guideline Development Panels, and PVA.
5. Disclosure of Conflict: Recusal. If a Covered Person determines that a conflict exists, then he or she shall notify immediately the Steering Committee Chair or the Director of PVA’s Research and Education Department. The Chair, with input from the Director of Research and Education, shall determine whether a conflict exists (except that in cases of conflicts involving the Chair, the Vice Chair shall decide). The decision on conflicts and the basis of that decision shall be reported to the Steering Committee and recorded in the minutes. Unless otherwise determined by the Chair (or, as appropriate, the Vice Chair) in individual cases, if a conflict is found to exist, the affected person shall recuse himself/herself from all discussions, determinations and votes with respect to the matter with which the conflict exists, and shall excuse him/herself from all meetings at which any discussions regarding the matter take place. Following the termination of such determinations and discussions involving the conflict, such Covered Person may rejoin the meeting.
POLICY ON CONFIDENTIALITY
In the course of conducting regular business for the Consortium and/or Guideline Development Panel(s), Steering Committee Members and Panel Members may receive and be given access to confidential information concerning PVA or another entity working with the Consortium. To ensure that the confidentiality of the information will be maintained, the following Policy on Confidentiality is adopted.
1. Applicability. This Policy applies to the Consortium’s Steering Committee Members, including the Chair and Vice-Chair, in addition to those members on the Guideline Development Panels (collectively, “Covered Persons”).
2. Term. This agreement is effective for the term the Covered Person is a member of the Steering Committee and/or a Guideline Development Panel, notwithstanding how active or passive a role they
may play as a member of the Steering Committee or a Guideline Development Panel.
3. Definition of Confidential Information. “Confidential Information” means (i) all written business, financial, technical and scientific information relating to the Consortium and which PVA has marked conspicuously “CONFIDENTIAL,” “PROPRIETARY,” or similar marking; or (ii) oral information which is specified as confidential by the Steering Committee and/or PVA. All documents derived during the guideline development process are confidential, and they remain so until 1) the document has been approved for publication by a vote of the Steering Committee and 2) the document is released by PVA as a printed document.
“Confidential Information” shall exclude information which (a) is in the public domain at the time of disclosure; (b) is in the possession of the Consortium (including any Covered Person) free of any obligation of confidence prior to the time of disclosure; (c) though originally within the definition of “Confidential Information”, subsequently becomes part of the public
knowledge through no fault of the Consortium (including any Covered Person), as of the date of its becoming part of the public knowledge; (d) though originally within the definition of “Confidential Information”, subsequently
is received by the Consortium (including any Covered Person) without any obligation of confidentiality from a third party who is free to disclose the information, as of the date of such third-party disclosure; or (e) is independently developed by the Consortium without the use of any Confidential Information.
4. Nondisclosure of Confidential Information. Each Covered Person agrees not to disclose to any person outside the Consortium or its affiliates (including for these purposes Chapters and International Affiliates) any Confidential Information, except as provided below. Each Covered Person agrees that he/she will use the Confidential Information only for the purpose of Consortium business. Notwithstanding the foregoing, a Covered Person may disclose the Confidential Information (i) to employees, professional advisors, volunteer scientists and other Covered Persons asked to participate in Consortium business, consultants and agents of the Consortium who have a need to know and who have been informed of this Policy on Confidentiality; or (ii) to the extent required by a court order or by law. Each Covered Person shall use the same degree of care, but not less than a reasonable degree of care, that he/ she uses to protect the Consortium’s own most highly confidential information to prevent any unauthorized or inadvertent disclosure of Confidential Information.
Any individual having question(s) concerning this policy or its applicability in a given situation(s) should address those question(s) to the Director of Research and Education (PVA).
5. Return of Confidential Information.
Each Covered Person agrees to return to the Chair of the Steering Committee or the Director of Research and Education, all tangible materials incorporating Confidential Information made available or supplied to such Covered Person and all copies and reproductions thereof upon request of the Chair of the Committee and/or the Director of Research and Education (PVA).
References
- 1.Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest. Feb 1989;95(2 Suppl): 2S-4S. [PubMed] [Google Scholar]
- 2.U.S . Task force for preventive services: Guide to clinical preventive services. 2nd ed. Baltimore, MD: Williams & Wilkins; 1996. [Google Scholar]
- 3.Craig A, Tran Y, Middleton J.. Psychological morbidity and spinal cord injury: A systematic review. Spinal Cord. Feb 2009;47(2):108-114. [DOI] [PubMed] [Google Scholar]
- 4.American Psychiatric Association DSM-5 Taskforce . Diagnostic and statistical manual of mental disorders. Fifth ed. Arlington, VA: American Pychiatric Association; 2013. [Google Scholar]
- 5.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Fourth, Text Revision. ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 6.Affairs USDoV . Depression and spinal cord injuries and disorders. Veterans Health Library 2017. Accessed March 16, 2017.
- 7.Craig AR, Hancock KM, Dickson HG.. A longitudinal investigation into anxiety and depression in the first 2 years following a spinal cord injury. Paraplegia. 1994;32(10):675-679. [DOI] [PubMed] [Google Scholar]
- 8.Scivoletto G, Petrelli A, Di Lucente L, Castellano V.. Psychological investigation of spinal cord injury patients. Spinal Cord. Aug 1997;35(8):516-520. [DOI] [PubMed] [Google Scholar]
- 9.Chung MC, Preveza E, Papandreou K, Prevezas N.. The relationship between posttraumatic stress disorder following spinal cord injury and locus of control. J Affect Disord. Jul 2006;93(1-3):229-232. [DOI] [PubMed] [Google Scholar]
- 10.Kennedy P, Evans MJ.. Evaluation of post traumatic distress in the first 6 months following sci. Spinal Cord. 2001;39(7):381-386. [DOI] [PubMed] [Google Scholar]
- 11.Tetrault M, Courtois F.. Use of psychoactive substances in persons with spinal cord injury: A literature review. Ann Phys Rehabil Med. Dec 2014;57(9-10):684-695. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy P, Garmon-Jones L.. Self-harm and suicide before and after spinal cord injury: A systematic review. Spinal Cord. Jan 2017;55(1):2-7. [DOI] [PubMed] [Google Scholar]
- 13.Craig A, Nicholson Perry K, Guest R, Tran Y, Dezarnaulds A, Hales A, Ephraums C, Middleton J.. Prospective study of the occurrence of psychological disorders and comorbidities after spinal cord injury. Arch Phys Med Rehabil. Aug 2015;96(8):1426-1434. [DOI] [PubMed] [Google Scholar]
- 14.Fann JR, Bombardier CH, Richards JS, Tate DG, Wilson CS, Temkin N.. Depression after spinal cord injury: Comorbidities, mental health service use, and adequacy of treatment. Arch Phys Med Rehab. Mar 2011;92(3):352-360. [DOI] [PubMed] [Google Scholar]
- 15.Katzelnick DJ, Williams MD.. Large-scale dissemination of collaborative care and implications for psychiatry. Psychiatr Serv. Sep 2015;66(9):904-906. [DOI] [PubMed] [Google Scholar]
- 16.American College of Surgeons CoT . Alcohol screening and brief intervention for trauma patients. undated.
- 17.Zatzick D, Roy-Byrne P, Russo J, Rivara F, Droesch R, Wagner A, Dunn C, Jurkovich G, Uehara E, Katon W.. A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Arch Gen Psychiatry. May 2004;61(5):498-506. [DOI] [PubMed] [Google Scholar]
- 18.Fann JR, Crane DA, Graves DE, Kalpakjian CZ, Tate DG, Bombardier CH.. Depression treatment preferences after acute traumatic spinal cord injury. Arch Phys Med Rehabil. Dec 2013;94(12):2389-2395. [DOI] [PubMed] [Google Scholar]
- 19.Undertaking systematic reviews of research on effectiveness: Crd’s guidance for those carrying out or commissioning reviews. York: Centre for Reviews and Dissemination: University of York; 2001.
- 20.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D, Methods Work Group TUSPSTF. Current methods of the us preventive services task force: A review of the process. Am J Prev Med. Apr 2001;20(3 Suppl): 21-35. [DOI] [PubMed] [Google Scholar]
- 21.Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, Montori V, Akl EA, Djulbegovic B, Falck-Ytter Y, Norris SL, Williams JW, Jr., Atkins D, Meerpohl J, Schunemann HJ.. Grade guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). J Clin Epidemiol. Apr 2011;64(4):407-415. [DOI] [PubMed] [Google Scholar]
- 22.Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C.. Assessing bias in studies of prognostic factors. Ann Intern Med. Feb 19 2013;158(4):280-286. [DOI] [PubMed] [Google Scholar]
- 23.Guyatt G, Oxman AD, Sultan S, Brozek J, Glasziou P, Alonso-Coello P, Atkins D, Kunz R, Montori V, Jaeschke R, Rind D, Dahm P, Akl EA, Meerpohl J, Vist G, Berliner E, Norris S, Falck-Ytter Y, Schunemann HJ.. Grade guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol. Feb 2013;66(2):151-157. [DOI] [PubMed] [Google Scholar]
- 24.Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso- Coello P, Rind D, Devereaux PJ, Montori VM, Freyschuss B, Vist G, Jaeschke R, Williams JW, Jr., Murad MH, Sinclair D, Falck-Ytter Y, Meerpohl J, Whittington C, Thorlund K, Andrews J, Schunemann HJ.. Grade guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol. Dec 2011;64(12):1283-1293. [DOI] [PubMed] [Google Scholar]
- 25.Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, Alonso-Coello P, Djulbegovic B, Atkins D, Falck-Ytter Y, Williams JW, Jr., Meerpohl J, Norris SL, Akl EA, Schunemann HJ.. Grade guidelines: 5. Rating the quality of evidence--publication bias. J Clin Epidemiol. Dec 2011;64(12):1277-1282. [DOI] [PubMed] [Google Scholar]
- 26.Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH.. Grade guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. Apr 2011;64(4):401-406. [DOI] [PubMed] [Google Scholar]
- 27.Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, Alonso-Coello P, Glasziou P, Jaeschke R, Akl EA, Norris S, Vist G, Dahm P, Shukla VK, Higgins J, Falck-Ytter Y, Schunemann HJ, Group GW.. Grade guidelines: 7. Rating the quality of evidence--inconsistency. J Clin Epidemiol. Dec 2011;64(12):1294-1302. [DOI] [PubMed] [Google Scholar]
- 28.Stata statistical software: Release 14 [computer program]. College Station, TX: StataCorp LP; 2015.
- 29.Tate D, Forchheimer M, Maynard F, Dijkers M.. Predicting depression and psychological distress in persons with spinal cord injury based on indicators of handicap. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. Jun 1994;73(3):175-183. [DOI] [PubMed] [Google Scholar]
- 30.Frank RG, Elliott TR, Corcoran J, Wonderlich S.. Depression after spinal cord injury: Is it necessary? Clin Psychol Rev. 1987;7(6):611-630. [Google Scholar]
- 31.Craig A, Tran Y, Siddall P, Wijesuriya N, Lovas J, Bartrop R, Middleton J.. Developing a model of associations between chronic pain, depressive mood, chronic fatigue, and self-efficacy in people with spinal cord injury. J Pain. Sep 2013;14(9):911-920. [DOI] [PubMed] [Google Scholar]
- 32.Dobrez D, Heinemann AW, Deutsch A, Durkin EM, Almagor O.. Impact of mental disorders on cost and reimbursement for patients in inpatient rehabilitation facilities. Arch Phys Med Rehabil. Feb 2010;91(2):184-188. [DOI] [PubMed] [Google Scholar]
- 33.Stroud MW, Bombardier CH, Dyer JR, Rimmele CT, Esselman PC.. Preinjury alcohol and drug use among persons with spinal cord injury: Implications for rehabilitation. J Spinal Cord Med. 2011;34(5):461-472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cao Y, Clark JMR, Krause JS.. Changes in psychotropic prescription medication use and their relationship with mortality among people with traumatic spinal cord injury. Spinal Cord. Feb 26 2018. [DOI] [PubMed] [Google Scholar]
- 35.Young AS, Klap R, Shoai R, Wells KB.. Persistent depression and anxiety in the united states: Prevalence and quality of care. Psychiatr Serv. Dec 2008;59(12):1391-1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rodriguez BF, Weisberg RB, Pagano ME, Machan JT, Culpepper L, Keller MB.. Mental health treatment received by primary care patients with posttraumatic stress disorder. J Clin Psychiatry. Oct 2003;64(10):1230-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnson-Lawrence V, Zivin K, Szymanski BR, Pfeiffer PN, McCarthy JF.. Va primary care-mental health integration: Patient characteristics and receipt of mental health services, 2008-2010. Psychiatr Serv. Nov 2012;63(11):1137-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Craig A, Nicholson Perry K.. Guide for health profes- sionals on the psychosocial care of adults with spinal cord injury. In: AfC Innovation, ed. Chatswood, NSW Australia: ACI State Spinal Cord Injury Service; 2014. [Google Scholar]
- 39.Macciocchi S, Seel RT, Warshowsky A, Thompson N, Barlow K.. Co-occurring traumatic brain injury and acute spinal cord injury rehabilitation outcomes. Arch Phys Med Rehabil. Oct 2012;93(10):1788-1794. [DOI] [PubMed] [Google Scholar]
- 40.Banerjea R, Findley PA, Smith B, Findley T, Sambamoorthi U.. Co-occurring medical and mental illness and substance use disorders among veteran clinic users with spinal cord injury patients with complexities. Spinal Cord. 2009;47(11):789-795. [DOI] [PubMed] [Google Scholar]
- 41.Van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J.. Pain prevalence and its determinants after spinal cord injury: A systematic review. Eur J Pain. Jan 2015;19(1):5-14. [DOI] [PubMed] [Google Scholar]
- 42.Bonanno G, Kennedy P, Galatzer-Levy I, Lude P, Elfström M.. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabil Psychol. 2012;57:236-247. [DOI] [PubMed] [Google Scholar]
- 43.Russell HF, Richardson EJ, Bombardier CH, Dixon TM, Huston TA, Rose J, Sheaffer D, Smith SA, Ullrich PM.. Professional standards of practice for psychologists, social workers, and counselors in sci rehabilitation. J Spinal Cord Med. 2016;39(2):127-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Coventry PA, Hudson JL, Kontopantelis E, Archer J, Richards DA, Gilbody S, Lovell K, Dickens C, Gask L, Waheed W, Bower P.. Characteristics of effective collaborative care for treatment of depression: A systematic review and meta-regression of 74 randomised controlled trials. PLoS One. 2014;9(9):e108114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang PS, Berglund P, Kessler RC.. Recent care of common mental disorders in the united states : Prevalence and conformance with evidence- based recommendations. J Gen Intern Med. May 2000;15(5):284-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Szymanski BR, Bohnert KM, Zivin K, McCarthy JF.. Integrated care: Treatment initiation following positive depression screens. J Gen Intern Med. Mar 2013;28(3):346-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Unutzer J, Katon W, Callahan CM, Williams JW, Jr., Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noel PH, Lin EH, Arean PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C.. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA. Dec 11 2002;288(22):2836-2845. [DOI] [PubMed] [Google Scholar]
- 48.Bombardier CH, Fann J, Ehde D, Reyes R, Hoffman J.. Collaborative care for pain, depression and physical inactivity in an outpatient sci clinic: The sci-care study. Arch Phys Med Rehabil. 2016;97(10):e78-e79. [Google Scholar]
- 49.Medicine. Io. Crossing the quality chasm: A new health system for the 21st century. Washington DC2001.
- 50.Fortney JC, Unutzer J, Wrenn G, Pyne JM, Smith GR, Schoenbaum M, Harbin HT.. A tipping point for measurement-based care. Psychiatr Serv. Feb 1 2017;68(2):179-188. [DOI] [PubMed] [Google Scholar]
- 51.Landes SJ, Carlson EB, Ruzek JI, Wang D, Hugo E, DeGaetano N, Chambers JG, Lindley SE.. Provider-driven development of a measurement feedback system to enhance measurement-based care in va mental health. Cognitive and Behavioral Practice. 2015;22:87-100. [Google Scholar]
- 52.Guo T, Xiang YT, Xiao L, Hu CQ, Chiu HF, Ungvari GS, Correll CU, Lai KY, Feng L, Geng Y, Feng Y, Wang G.. Measurement-based care versus standard care for major depression: A randomized controlled trial with blind raters. Am J Psychiatry. Oct 2015;172(10):1004-1013. [DOI] [PubMed] [Google Scholar]
- 53.Frank E, Prien RF, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, Rush AJ, Weissman MM.. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. Sep 1991;48(9):851-855. [DOI] [PubMed] [Google Scholar]
- 54.Hunt WA, Barnett LW, Branch LG.. Relapse rates in addiction programs. J Clin Psychol. Oct 1971;27(4):455-456. [DOI] [PubMed] [Google Scholar]
- 55.Le J, Dorstyn D.. Anxiety prevalence following spinal cord injury: A meta-analysis. Spinal Cord. Aug 2016;54(8):570-578. [DOI] [PubMed] [Google Scholar]
- 56.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE.. Prevalence, severity, and comorbidity of 12-month dsm-iv disorders in the national comorbidity survey replication. Arch Gen Psychiatry. Jun 2005;62(6):617-627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leander M, Lampa E, Rask-Andersen A, Franklin K, Gislason T, Oudin A, Svanes C, Toren K, Janson C.. Impact of anxiety and depression on respiratory symptoms. Respir Med. Nov 2014;108(11):1594-1600. [DOI] [PubMed] [Google Scholar]
- 58.McLean CP, Asnaani A, Litz BT, Hofmann SG.. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. Aug 2011;45(8):1027-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lim SW, Shiue YL, Ho CH, Yu SC, Kao PH, Wang JJ, Kuo JR.. Anxiety and depression in patients with traumatic spinal cord injury: A nationwide population- based cohort study. PLoS One. 2017;12(1):e0169623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tasiemski T, Brewer BW.. Athletic identity, sport participation, and psychological adjustment in people with spinal cord injury. Adapted physical activity quarterly: APAQ. Jul 2011;28(3):233-250. [DOI] [PubMed] [Google Scholar]
- 61.Migliorini CE, New PW, Tonge BJ.. Comparison of depression, anxiety and stress in persons with traumatic and non-traumatic post-acute spinal cord injury. Spinal Cord. Nov 2009;47(11):783-788. [DOI] [PubMed] [Google Scholar]
- 62.Jones K, Simpson GK, Briggs L, Dorsett P.. Does spirituality facilitate adjustment and resilience among individuals and families after sci? Disabil Rehabil. 2016;38(10):921-935. [DOI] [PubMed] [Google Scholar]
- 63.Van Leeuwen CM, Kraaijeveld S, Lindeman E, Post MW.. Associations between psychological factors and quality of life ratings in persons with spinal cord injury: A systematic review. Spinal cord. Mar 2012;50(3):174-187. [DOI] [PubMed] [Google Scholar]
- 64.Abdul-Sattar AB. Predictors of functional outcome in patients with traumatic spinal cord injury after inpatient rehabilitation: In saudi arabia. Neurorehabilitation. Jan 1 2014;35(2):341-347. [DOI] [PubMed] [Google Scholar]
- 65.Zigmond AS, Snaith RP.. The hospital anxiety and depression scale. Acta Psychiatr Scand. Jun 1983;67(6):361-370. [DOI] [PubMed] [Google Scholar]
- 66.Kisala PA, Tulsky DS, Kalpakjian CZ, Heinemann AW, Pohlig RT, Carle A, Choi SW.. Measuring anxiety after spinal cord injury: Development and psychometric characteristics of the sci-qol anxiety item bank and linkage with gad-7. J Spinal Cord Med. May 2015;38(3):315-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Spitzer RL, Kroenke K, Williams JB, Lowe B.. A brief measure for assessing generalized anxiety disorder: The gad-7. Archives of internal medicine. May 22 2006;166(10):1092-1097. [DOI] [PubMed] [Google Scholar]
- 68.Woolrich RA, Kennedy P, Tasiemski T.. A preliminary psychometric evaluation of the hospital anxiety and de- pression scale (hads) in 963 people living with a spinal cord injury. Psychol Health Med. Feb 2006;11(1):80-90. [DOI] [PubMed] [Google Scholar]
- 69.Paker N, Bugdayci D, Midik M, Celik B, Kesiktas N.. Reliability of the turkish version of the hospital anxiety and depression scale in the people with traumatic spinal cord injury. NeuroRehabilitation. 2013;33(2):337-341. [DOI] [PubMed] [Google Scholar]
- 70.Muller R, Cieza A, Geyh S.. Rasch analysis of the hospital anxiety and depression scale in spinal cord injury. Rehabil Psychol. Aug 2012;57(3):214-223. [DOI] [PubMed] [Google Scholar]
- 71.Kroenke K, Spitzer RL, Williams JB, Lowe B.. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen Hosp Psychiatry. Jul-Aug 2010;32(4):345-359. [DOI] [PubMed] [Google Scholar]
- 72.Grencavage LM, Norcross JC.. Where are the commonalities among the therapeutic common factors? Professional Psychology: Research and Practice. 1990;21(5):372-378. [Google Scholar]
- 73.Craske M, Bystritsky A.. Approach to treating generalized anxiety disorder in adults. UpToDate Inc. 2017. https://www-uptodate-com.offcampus.lib. washington.edu. Accessed December 3, 2017.
- 74.Stolp-Smith KA, Wainberg MC.. Antidepressant exacerbation of spasticity. Arch Phys Med Rehab. Mar 1999;80(3):339-342. [DOI] [PubMed] [Google Scholar]
- 75.Rabchevsky AG, Kitzman PH.. Latest approaches for the treatment of spasticity and autonomic dysreflexia in chronic spinal cord injury. Neurotherapeutics. Apr 2011;8(2):274-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Roy-Byrne PP, Craske M.. Approach to treating panic disorder with or without agoraphobia in adults. UpToDate Inc. 2017. https://www-uptodate-com.offcampus.lib.washington.edu. Accessed December 3, 2017.
- 77.Sobieraj DM, Martinez BK, Hernandez AV, Coleman CI, Ross JS, Berg KM, Steffens DC, Baker WL.. Adverse effects of pharmacologic treatments of major depression in older adults. J Am Geriatr Soc. Aug 2019;67(8):1571-1581. [DOI] [PubMed] [Google Scholar]
- 78.Dorstyn D, Mathias J, Denson L.. Efficacy of cognitive behavior therapy for the management of psychological outcomes following spinal cord injury: A meta-analysis. J Health Psychol. Mar 2011;16(2):374-391. [DOI] [PubMed] [Google Scholar]
- 79.Mehta S, Orenczuk S, Hansen KT, Aubut JA, Hitzig SL, Legassic M, Teasell RW, Spinal Cord Injury Rehabilitation Evidence Research T. An evidence-based review of the effectiveness of cognitive behavioral therapy for psychosocial issues post-spinal cord injury. Rehabil Psychol. Feb 2011;56(1):15-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kennedy P, Taylor N, Hindson L.. A pilot investigation of a psychosocial activity course for people with spinal cord injuries. Psychol Health Med. Feb 2006;11(1):91-99. [DOI] [PubMed] [Google Scholar]
- 81.Hunot V, Churchill R, de Lima M Silva, Teixeira V.. Psychological therapies for generalised anxiety disorder. Cochrane Database Syst Rev. Jan 24 2007(1):CD001848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Williams R, Murray A.. Prevalence of depression after spinal cord injury: A meta-analysis. Arch Phys Med Rehabil. Jan 2015;96(1):133-140. [DOI] [PubMed] [Google Scholar]
- 83.van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J.. Pain prevalence and its determinants after spinal cord injury: A systematic review. Eur J Pain. Jan 2015;19(1):5-14. [DOI] [PubMed] [Google Scholar]
- 84.Arango-Lasprilla JC, Ketchum JM, Starkweather A, Nicholls E, Wilk AR.. Factors predicting depression among persons with spinal cord injury 1 to 5 years post injury. Neurorehabilitation. 2011;29(1):9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bailey J, Dijkers MP, Gassaway J, Thomas J, Lingefelt P, Kreider SE, Whiteneck G.. Relationship of nursing education and care management inpatient rehabilitation interventions and patient characteristics to outcomes following spinal cord injury: The scirehab project. Journal of Spinal Cord Medicine. Nov 2012;35(6):593-610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Riggins MS, Kankipati P, Oyster ML, Cooper RA, Boninger ML.. The relationship between quality of life and change in mobility 1 year postinjury in individuals with spinal cord injury. Arch Phys Med Rehabil. Jul 2011;92(7):1027-1033. [DOI] [PubMed] [Google Scholar]
- 87.Hwang M, Zebracki K, Chlan KM, Vogel LC.. Longitudinal employment outcomes in adults with pediatric-onset spinal cord injury. Spinal Cord. Jun 2014;52(6):477-482. [DOI] [PubMed] [Google Scholar]
- 88.January AM, Zebracki K, Chlan KM, Vogel LC.. Symptoms of depression over time in adults with pediatric-onset spinal cord injury. Arch Phys Med Rehabil. Mar 2014;95(3):447-454. [DOI] [PubMed] [Google Scholar]
- 89.Hartoonian N, Hoffman JM, Kalpakjian CZ, Taylor HB, Krause JK, Bombardier CH.. Evaluating a spinal cord injury-specific model of depression and quality of life. Arch Phys Med Rehabil. Mar 2014;95(3):455-465. [DOI] [PubMed] [Google Scholar]
- 90.Tasiemski T, Brewer BW.. Athletic identity, sport participation, and psychological adjustment in people with spinal cord injury. Adapt Phys Act Q. Jul 2011;28(3):233-250. [DOI] [PubMed] [Google Scholar]
- 91.Saunders LL, Krause JS, Focht KL.. A longitudinal study of depression in survivors of spinal cord injury. Spinal Cord. Jan 2012;50(1):72-77. [DOI] [PubMed] [Google Scholar]
- 92.Burns SM, Hough S, Boyd BL, Hill J.. Sexual desire and depression following spinal cord injury: Masculine sexual prowess as a moderator. Sex Roles. Jul 2009;61(1-2):120-129. [Google Scholar]
- 93.Bombardier CH, Fann JR, Tate DG, Richards JS, Wilson CS, Warren AM, Temkin NR, Heinemann AW, Investigators P.. An exploration of modifiable risk factors for depression after spinal cord injury: Which factors should we target? Arch Phys Med Rehabil. May 2012;93(5):775-781. [DOI] [PubMed] [Google Scholar]
- 94.Dryden DM, Saunders L, Rowe BH, May LA, Yiannakoulias N, Svenson LW, Schopflocher DP, Voaklander DC.. Depression following traumatic spinal cord injury. Neuroepidemiology. Jul 2005;25(2):55-61. [DOI] [PubMed] [Google Scholar]
- 95.Hassanpour K, Hotz-Boendermaker S, Dokladal P, European Multicenter Study for Human Spinal Cord Injury Study g, Curt A. Low depressive symptoms in acute spinal cord injury compared to other neurological disorders. J Neurol. Jun 2012;259(6):1142-1150. [DOI] [PubMed] [Google Scholar]
- 96.Williams RT, Wilson CS, Heinemann AW, Lazowski LE, Fann JR, Bombardier CH.. Identifying depression severity risk factors in persons with traumatic spinal cord injury. Rehabilitation psychology. 2014;59(1):50-56. [DOI] [PubMed] [Google Scholar]
- 97.Bombardier CH, Adams LM, Fann JR, Hoffman JM.. Depression trajectories during the first year after spinal cord injury. Archives of Physical and Medical Rehabilitation. 2016;97:196-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cuff L, Fann JR, Bombardier CH, Graves DE, Kalpakjian CZ.. Depression, pain intensity, and interference in acute spinal cord injury. Topics in Spinal Cord Injury Rehabilitation. 2014;20(1):32-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ullrich PM, Lincoln RK, Tackett MJ, Miskevics S, Smith BM, Weaver FM.. Pain, depression, and health care utilization over time after spinal cord injury. Rehabilitation Psychology. May 2013;58(2):158-165. [DOI] [PubMed] [Google Scholar]
- 100.Tsai IH, Graves DE, Lai CH, Hwang LY, Pompeii LA.. Association of internet use and depression among the spinal cord injury population. Arch Phys Med Rehabil. Feb 2014;95(2):236-243. [DOI] [PubMed] [Google Scholar]
- 101.Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS.. A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil. Mar 2011;92(3):411-418. [DOI] [PubMed] [Google Scholar]
- 102.Alschuler KN, Jensen MP, Sullivan-Singh SJ, Borson S, Smith AE, Molton IR.. The association of age, pain, and fatigue with physical functioning and depressive symptoms in persons with spinal cord injury. Journal of Spinal Cord Medicine. Sep 2013;36(5):483-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.January AM, Zebracki K, Chlan KM, Vogel LC.. Mental health and risk of secondary medical complications in adults with pediatric-onset spinal cord injury. Topics in Spinal Cord Injury Rehabilitation. 2014;20(1):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lin MR, Hwang HF, Yu WY, Chen CY.. A prospective study of factors influencing return to work after traumatic spinal cord injury in taiwan. Arch Phys Med Rehabil. Oct 2009;90(10):1716-1722. [DOI] [PubMed] [Google Scholar]
- 105.Burns SM, Boyd BL, Hill J, Hough S.. Psychosocial predictors of employment status among men living with spinal cord injury. Rehabilitation Psychology. Feb 2010;55(1):81-90. [DOI] [PubMed] [Google Scholar]
- 106.Pakpour AH, Kumar S, Scheerman JF, Lin CY, Fridlund B, Jansson H.. Oral health-related quality of life in iranian patients with spinal cord injury: A case- control study. Injury. Jun 2016;47(6):1345-1352. [DOI] [PubMed] [Google Scholar]
- 107.Craig A, Nicholson Perry K, Guest R, Tran Y, Middleton J.. Adjustment following chronic spinal cord injury: Determining factors that contribute to social participation. Br J Health Psychol. Nov 2015;20(4):807-823. [DOI] [PubMed] [Google Scholar]
- 108.Kalpakjian CZ, Bombardier CH, Schomer K, Brown PA, Johnson KL.. Measuring depression in persons with spinal cord injury: A systematic review. The journal of spinal cord medicine. 2009;32(1):6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sakakibara BM, Miller WC, Orenczuk SG, Wolfe DL, Team SR.. A systematic review of depression and anxiety measures used with individuals with spinal cord injury. Spinal Cord. Dec 2009;47(12):841-851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tulsky DS, Kisala PA, Kalpakjian CZ, Bombardier CH, Pohlig RT, Heinemann AW, Carle A, Choi SW.. Measuring depression after spinal cord injury: Development and psychometric characteristics of the sci-qol depression item bank and linkage with phq-9. J Spinal Cord Med. May 2015;38(3):335-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bombardier CH, Kalpakjian CZ, Graves DE, Dyer JR, Tate DG, Fann JR.. Validity of the patient health questionnaire-9 in assessing major depressive disorder during inpatient spinal cord injury rehabilitation. Arch Phys Med Rehabil. Oct 2012;93(10):1838-1845. [DOI] [PubMed] [Google Scholar]
- 112.Bombardier CH, Richards JS, Krause JS, Tulsky D, Tate DG.. Symptoms of major depression in people with spinal cord injury: Implications for screening. Arch Phys Med Rehabil. Nov 2004;85(11):1749-1756. [DOI] [PubMed] [Google Scholar]
- 113.Cook KF, Kallen MA, Bombardier C, Bamer AM, Choi SW, Kim J., Salem R, Amtman D.. Do measures of depressive symptoms function differently in people with spinal cord injury versus primary care patients: The ces-d, phq-9, and promis-d. Qual Life Res. 2016. [DOI] [PubMed] [Google Scholar]
- 114.Radnitz CL, Broderick CP, Perez-Strumolo L, Tirch DD, Festa J, Schlein IS, Walczak S, Willard J, Lillian LB, Binks M.. The prevalence of psychiatric disorders in veterans with spinal cord injury: A controlled comparison. J Nerv Ment Dis. Jul 1996;184(7):431-433. [DOI] [PubMed] [Google Scholar]
- 115.Tate DG, Forchheimer M, Maynard F, Davidoff G, Dijkers M.. Comparing two measures of depression in spinal cord injury. Rehabilitation Psychology. Spr 1993;38(1):53-61. [Google Scholar]
- 116.Krause JS, Saunders LL, Reed KS, Coker J, Zhai Y, Johnson E.. Comparison of the patient health questionnaire and the older adult health and mood questionnaire for self-reported depressive symptoms after spinal cord injury. Rehabil Psychol. Nov 2009;54(4):440-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Katon W, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, Peterson D, Rutter CM, McGregor M, McCulloch D.. Collaborative care for patients with depression and chronic illnesses. The New England journal of medicine. Dec 30 2010;363(27):2611-2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Atlantis E, Fahey P, Foster J.. Collaborative care for comorbid depression and diabetes: A systematic review and meta-analysis. BMJ Open. 2014;4(4):e004706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Huffman JC, Niazi SK, Rundell JR, Sharpe M, Katon WJ.. Essential articles on collaborative care models for the treatment of psychiatric disorders in medical settings: A publication by the academy of psychosomatic medicine research and evidence-based practice committee. Psychosomatics. Mar-Apr 2014;55(2):109-122. [DOI] [PubMed] [Google Scholar]
- 120.Gerhart KA, Koziol-McLain J, Lowenstein SR, Whiteneck GG.. Quality of life following spinal cord injury: Knowledge and attitudes of emergency care providers. Ann Emerg Med. Apr 1994;23(4):807-812. [DOI] [PubMed] [Google Scholar]
- 121.Dorsett P, Geraghty T, Sinnott A, Acland R.. Hope, coping and psychosocial adjustment after spinal cord injury. Spinal Cord Ser Cases. 2017;3:17046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bombardier CH, Fann JR, Tate DG, Richards JS, Wilson CS, Warren AM, Temkin NR, Heinemann AW.. An exploration of modifiable risk factors for depression after spinal cord injury: Which factors should we target? Arch Phys Med Rehabil. May 2012;93(5):775-781. [DOI] [PubMed] [Google Scholar]
- 123.Kautz CM, Gittell JH, Weinberg DB, Lusenhop RW, Wright J.. Patient benefits from participating in an integrated delivery system: Impact on coordination of care. Health Care Manage Rev. Jul-Sep 2007;32(3):284-294. [DOI] [PubMed] [Google Scholar]
- 124.Kautz LM, Kautz DD.. Transforming our patients, their families, and ourselves: Share the experience. International Journal for Human Caring. 2017;21(3):159-160. [Google Scholar]
- 125.Arpawong TE, Richeimer SH, Weinstein F, Elghamrawy A, Milam JE.. Posttraumatic growth, quality of life, and treatment symptoms among cancer chemotherapy outpatients. Health Psychol. Apr 2013;32(4):397-408. [DOI] [PubMed] [Google Scholar]
- 126.Cuijpers P, Dekker J, Hollon SD, Andersson G.. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: A meta- analysis. J Clin Psychiatry. Sep 2009;70(9):1219-1229. [DOI] [PubMed] [Google Scholar]
- 127.Cuijpers P, van Straten A, Warmerdam L, Andersson G.. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: A meta-analysis. Depress Anxiety. 2009;26(3):279-288. [DOI] [PubMed] [Google Scholar]
- 128.Cuijpers P, Reynolds CF, 3rd, Donker T, Li J, Andersson G, Beekman A.. Personalized treatment of adult depression: Medication, psychotherapy, or both? A systematic review. Depress Anxiety. Oct 2012;29(10):855-864. [DOI] [PubMed] [Google Scholar]
- 129.Ravindran AV, Balneaves LG, Faulkner G, Ortiz A, McIntosh D, Morehouse RL, Ravindran L, Yatham LN, Kennedy SH, Lam RW, MacQueen GM, Milev RV, Parikh SV, Group CDW.. Canadian network for mood and anxiety treatments (canmat) 2016 clinical guidelines for the management of adults with major depressive disorder: Section 5. Complementary and alternative medicine treatments. Can J Psychiatry. Sep 2016;61(9):576-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Cardenas DD, Nieshoff EC, Suda K, Goto S, Sanin L, Kaneko T, Sporn J, Parsons B, Soulsby M, Yang R, Whalen E, Scavone JM, Suzuki MM, Knapp LE.. A randomized trial of pregabalin in patients with neuropathic pain due to spinal cord injury. Neurology. Feb 5 2013;80(6):533-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fann JR, Bombardier CH, Richards JS, Wilson CS, Heinemann AW, Warren AM, Brooks L, McCullumsmith CB, Temkin NR, Warms C, Tate DG, Investigators P.. Venlafaxine extended-release for depression following spinal cord injury: A randomized clinical trial. JAMA Psychiatry. Mar 1 2015;72(3):247-258. [DOI] [PubMed] [Google Scholar]
- 132.Judd FK, Stone J, Webber JE, Brown DJ, Burrows GD.. Depression following spinal cord injury. A prospective in-patient study. Br J Psychiatry. May 1989;154:668-671. [DOI] [PubMed] [Google Scholar]
- 133.National Institute for Health and Care Excellence . Depression in adults: Recognition and management. National Collaborating Centre for Mental Health; 2016. [PubMed]
- 134.Gelenberg AJ, Freeman MP, Markowitz JC, Rosenbaum JF, Thase ME, Trivedi MH, van Rhoads RS. Practice guideline for the treatment of patients with major depressive disorder. 2010. https://psychiatryonline.org/guidelines. Accessed February 2, 2019.
- 135.Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y, Leucht S, Ruhe HG, Turner EH, Higgins JPT, Egger M, Takeshima N, Hayasaka Y, Imai H, Shinohara K, Tajika A, Ioannidis JPA, Geddes JR.. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Lancet. Apr 7 2018;391(10128):1357-1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Antidepressant medication management . Healthcare Effectiveness Data and Information Set 2018; https://www.ncqa.org/hedis/measures/antidepressant-medication-management/. Accessed February2, 2019. [Google Scholar]
- 137.National Institute for Health and Care Excellence . Depression in adults: Recognition and management. National Collaborating Centre for Mental Health;2009. [PubMed] [Google Scholar]
- 138.Gelenberg AJ, Freeman MP, KMarkowitz JC, Rosenbaum JF, Thase ME, Trivedi MH, Rhoads RS.. Practice guideline for the treatment of patients with major depressive disorder. American Psychiatric Association;2010. [Google Scholar]
- 139.Trivedi MH, Rush AJ, Wisniewski SR, Nieren- berg AA, Warden D, Ritz L, Norquist G, Howland RH, Lebowitz B, McGrath PJ, Shores-Wilson K, Biggs MM, Balasubramani GK, Fava M, Team SDS.. Evaluation of outcomes with citalopram for depression using mea-surement-based care in star*d: Implications for clinical practice. Am J Psychiatry. Jan 2006;163(1):28-40. [DOI] [PubMed] [Google Scholar]
- 140.Perkes SJ, Bowman J, Penkala S.. Psychological therapies for the management of co-morbid depression following a spinal cord injury: A systematic review. J Health Psychol. Dec 2014;19(12):1597-1612. [DOI] [PubMed] [Google Scholar]
- 141.Dorstyn D, Mathias J, Denson L.. Efficacy of cognitive behavior therapy for the management of psychological outcomes following spinal cord injury: A meta-analysis. J Health Psychol. Mar 2011;16(2):374-391. [DOI] [PubMed] [Google Scholar]
- 142.Houlihan BV, Jette A, Friedman RH, Paasche-Orlow M, Ni P, Wierbicky J, Williams K, Ducharme S, Zazula J, Cuevas P, Rosenblum D, Williams S.. A pilot study of a telehealth intervention for persons with spinal cord dysfunction. Spinal Cord. Sep 2013;51(9):715-720. [DOI] [PubMed] [Google Scholar]
- 143.Houlihan BV, Jette A, Paasche-Orlow M, Wierbicky J, Ducharme S, Zazula J, Cuevas P, Friedman RH, Williams S.. A telerehabilitation intervention for persons with spinal cord dysfunction. Am J Phys Med Rehabil. Sep 2011;90(9):756-764. [DOI] [PubMed] [Google Scholar]
- 144.Mercier HW, Ni P, Houlihan BV, Jette AM.. Differ- ential impact and use of a telehealth intervention by persons with ms or sci. Am J Phys Med Rehabil. Nov 2015;94(11):987-999. [DOI] [PubMed] [Google Scholar]
- 145.Dorstyn D, Mathias J, Denson L.. Applications of telecounselling in spinal cord injury rehabilitation: A systematic review with effect sizes. Clinical Rehabilitation. Dec 2013;27(12):1072-1083. [DOI] [PubMed] [Google Scholar]
- 146.Nooijen CF, de Groot S, Postma K, Bergen MP, Stam HJ, Bussmann JB, van den Berg-Emons RJ.. A more active lifestyle in persons with a recent spinal cord injury benefits physical fitness and health. Spinal cord. Apr 2012;50(4):320-323. [DOI] [PubMed] [Google Scholar]
- 147.Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J, McCartney N.. Long-term exercise training in persons with spinal cord injury: Effects on strength, arm ergometry performance and psychological well-being. Spinal Cord. 2003;41(1):34-43. [DOI] [PubMed] [Google Scholar]
- 148.Ginis KA Martin, Latimer AE, McKechnie K, Ditor DS, McCartney N, Hicks AL, Bugaresti J, Craven BC.. Using exercise to enhance subjective well-being among people with spinal cord injury: The mediating influences of stress and pain. Rehabil Psychol. 2003;48(3):157-164. [Google Scholar]
- 149.Diego MA, Field T, Hernandez-Reif M, Hart S, Brucker B, Burman I.. Spinal cord paitents benefit from massage therapy. International Journal of Neuroscience. 2002;112(2):133-142. [DOI] [PubMed] [Google Scholar]
- 150.Kennedy P, Taylor N, Hindson L.. A pilot investigation of a psychosocial activity course for people with spinal cord injuries. Psychol Health Med. Feb 2006;11(1):91-99. [DOI] [PubMed] [Google Scholar]
- 151.Bradley MB. The effect of participating in a functional electrical stimulation exercise program on affect in people with spinal cord injuries. Arch Phys Med Rehabil. Jun 1994;75(6):676-679. [DOI] [PubMed] [Google Scholar]
- 152.Simon G. E. Unipolar major depression in adults: Choosing initial treatment. UpToDate Inc. 2017:1-27. Accessed 12/3/2017.
- 153.Tate DG, Forchheimer MB, Krause JS, Meade MA, Bombardier CH.. Patterns of alcohol and substance use and abuse in persons with spinal cord injury: Risk factors and correlates. Arch Phys Med Rehabil. Nov 2004;85(11):1837-1847. [DOI] [PubMed] [Google Scholar]
- 154.Lusilla-Palacios P, Castellano-Tejedor C.. Spinal cord injury and substance use: A systematic review. Adicciones. 2015;27(4):294-310. [PubMed] [Google Scholar]
- 155.Saunders LL, Krause JS. Prevalence of cigarette smoking and attempts to quit in a population-based cohort with spinal cord injury. Spinal cord. Advance online publication. Spinal Cord. 2016. [DOI] [PubMed]
- 156.Hatch MN, Raad J, Suda K, Stroupe KT, Hon AJ, Smith BM.. Evaluating the use of medicare part d in the veteran population with spinal cord injury/disorder. Arch Phys Med Rehabil. Jun 2018;99(6):1099-1107. [DOI] [PubMed] [Google Scholar]
- 157.Guilcher SJT, Hogan ME, Calzavara A, Hitzig SL, Patel T, Packer T, Lofters AK.. Prescription drug claims following a traumatic spinal cord injury for older adults: A retrospective population-based study in ontario, canada. Spinal Cord. Nov 2018;56(11):1059-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kitzman P, Cecil D, Kolpek JH.. The risks of polypharmacy following spinal cord injury. J Spinal Cord Med. 03 2017;40(2):147-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hand BN, Velozo CA, Krause JS.. Rasch measurement properties of the pain medication questionnaire in persons with spinal cord injury. Spinal Cord. Aug 1 2017. [DOI] [PubMed] [Google Scholar]
- 160.Clark JM, Cao Y, Krause JS.. Risk of pain medication misuse after spinal cord injury: The role of substance use, personality, and depression. J Pain. Feb 2017;18(2):166-177. [DOI] [PubMed] [Google Scholar]
- 161.Krause JS, Cao Y, Clark JMR.. Pain intensity, interference, and medication use after spinal cord injury: Association with risk of mortality after controlling for socioeconomic and other health factors. Arch Phys Med Rehabil. Dec 2017;98(12):2464-2470. [DOI] [PubMed] [Google Scholar]
- 162.Saunders LL, Krause JS.. Psychological factors affecting alcohol use after spinal cord injury. Spinal Cord. May 2011;49(5):637-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Schandler SL, Cohen MJ, Vulpe M, Frank SE.. Incidence and characteristics of spinal cord injured patients with a family history of alcoholism. Journal of Studies on Alcohol. Sep 1995;56(5):522-527. [DOI] [PubMed] [Google Scholar]
- 164.Tate DG, Forchheimer MB, Krause JS, Meade MA, Bombardier CH.. Patterns of alcohol and substance use and abuse in persons with spinal cord injury: Risk factors and correlates. Arch Phys Med Rehabil. Nov 2004;85(11):1837-1847. [DOI] [PubMed] [Google Scholar]
- 165.Garshick E, Kelley A, Cohen SA, Garrison A, Tun CG, Gagnon D, Brown R.. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord. Jul 2005;43(7):408-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Krause JS, Saunders LL.. Socioeconomic and behavioral risk factors for mortality: Do risk factors observed after spinal cord injury parallel those from the general USA population? Spinal Cord. 2012;50:609-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Richardson EJ, Richards JS, Stewart CC, Ness TJ.. Effects of nicotine on spinal cord injury pain: A randomized, double-blind, placebo controlled crossover trial. Top Spinal Cord Inj Rehabil. Spring 2012;18(2):101-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bethel M, Weaver FM, Bailey L, Miskevics S, Svircev JN, Burns SP, Hoenig H, Lyles K, Carbone LD.. Risk factors for osteoporotic fractures in persons with spinal cord injuries and disorders. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. Oct 2016;27(10):3011-3021. [DOI] [PubMed] [Google Scholar]
- 169.Carbone LD, Chin AS, Lee TA, Burns SP, Svircev JN, Hoenig HM, Akhigbe T, Weaver FM.. The association of opioid use with incident lower extremity fractures in spinal cord injury. J Spinal Cord Med. Mar 2013;36(2):91-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Saunders LL, Krause JS.. Behavioral factors related to fatigue among persons with spinal cord injury. Arch Phys Med Rehabil. Feb 2012;93(2):313-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R.. Primary care validation of a single-question alcohol screening test. J Gen Int Med. 2009;24(7):783-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R.. A single-question screening test for drug use in primary care. Arch Intern Med. 2010;170(13):1155-1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Gryczynski J, McNeely J, Wu LT, Subramaniam GA, Svikis DS, Cathers LA, Sharma G, King J, Jelstrom E, Nordeck CD, Sharma A, Mitchell SG, O’Grady KE, Schwartz RP.. Validation of the taps-1: A four-item screening tool to identify unhealthy substance use in primary care. J Gen Intern Med. Sep 2017;32(9):990-996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Brown RL, Rounds LA.. Conjoint screening questionnaires for alcohol and other drug abuse: Criterion validity in a primary care practice. Wisconsin Medical Journal. 1995;94(3):135-140. [PubMed] [Google Scholar]
- 175.Brown RL, Leonard T, Saunders LA, Papasouliotis O.. A two-item conjoint screen for alcohol and other drug problems. Journal of the American Board of Family Practitioners. 2001;14:95-106. [PubMed] [Google Scholar]
- 176.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR.. Audit-c as a brief screen for alcohol misuse in primary care. Alcoholism, clinical and experimental research. Jul 2007;31(7):1208-1217. [DOI] [PubMed] [Google Scholar]
- 177.Dugosh KL, Cacciola JS. Clinical assessment of substance use disorders. UpToDate Inc. 2018. https://www-uptodate-com.offcampus.lib.washington.edu. Accessed Accessed on August 30, 2018.
- 178.The Management of Substance Use Disorders Work Group . Va/dod clinical practice guideline for the management of substance use disorders. 2015. https://www.healthquality.va.gov/guidelines/mh/sud/. Accessed February 3, 2019. [Google Scholar]
- 179.Marlatt GA, Donovan DM, eds. Relapse prevention: Maintenance strategies in treatment of addictive behaviors. Second ed. New York: Guilford Press; 2005. [Google Scholar]
- 180.Prochaska JO, Diclemente CC, Norcross JC.. In search of how people change - applications to addictive behaviors. Am Psychol. Sep 1992;47(9):1102-1114. [DOI] [PubMed] [Google Scholar]
- 181.Substance Abuse and Mental Health Services Administration CfBHSaQ . The nsduh report: Substance use and mental health estimates from the 2013 national survey on drug use and health: Overview of findings. Rockville, md. Rockville, MD: Substance Abuse and Mental Health Services Administration.;2014. [PubMed]
- 182.Institute of Medicine NAoS . Broadening the base of treatment for alcohol problems. Washington, DC: National Acadeny Press; 1990. [PubMed] [Google Scholar]
- 183.Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, Viera AJ, Wilkins TM, Schwartz CJ, Richmond EM, Yeatts J, Evans TS, Wood SD, Harris RP.. Behavioral counseling after screening for alcohol misuse in primary care: A systematic review and meta-analysis for the u.S. Preventive services task force. Ann Intern Med. Nov 6 2012;157(9):645-654. [DOI] [PubMed] [Google Scholar]
- 184.O’Donnell A, Anderson P, Newbury-Birch D, Schulte B, Schmidt C, Reimer J, Kaner E.. The impact of brief alcohol interventions in primary healthcare: A systematic review of reviews. Alcohol Alcohol. Jan-Feb 2014;49(1):66-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Gentilello LM, Rivara FP, Donovan DM, Jurkovich GJ, Daranciang E, Dunn CW, Villaveces A, Copass M, Ries RR.. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. Oct 1999;230(4):473-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Stecker T, McGovern MP, Herr B.. An intervention to increase alcohol treatment engagement: A pilot trial. Journal of substance abuse treatment. Sep 2012;43(2):161-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Bombardier CH, Rimmele CT.. Alcohol use and readiness to change after spinal cord injury. Arch Phys Med Rehabil. Sep 1998;79(9):1110-1115. [DOI] [PubMed] [Google Scholar]
- 188.Gentilello L, Duggan P, Drummnd D, Tonnensen A, Degner E, Fischer R.. Major injury as a unique opportunity to initiate treatment in the alcoholic. Journal of Surgery. 1988;156:558-561. [DOI] [PubMed] [Google Scholar]
- 189.Basford JR, Rohe DE, Barnes CP, DePompolo RW.. Substance abuse attitudes and policies in us rehabilitation training programs: A comparison of 1985 and 2000. Arch Phys Med Rehab. Apr 2002;83(4):517-522. [DOI] [PubMed] [Google Scholar]
- 190.Cardoso E, Pruett SR, Chan F, Tansey TN.. Substance abuse assessment and treatment: The current training and practice of apa division 22 members. Rehabil Psychol. 2006;51(2):175-178. [Google Scholar]
- 191.Himstreet J. Va primary care tobacco cessation handbook: A resource for providers. 2014. https://www.mentalhealth.va.gov/quit-tobacco/docs/IB_10-565-Primary-Care-Smoking-Handbook-PROVIDERS-508.pdf. Accessed Feb 5, 2019.
- 192.Pfizer labs (per FDA) . Product information: Chantrix(r) oral tablets, varenicline oral tablets. New York, NY2014.
- 193.Pfizer labs (per FDA) . Product information: Chantrix(r) oral tablets, varenicline oral tablets. New York, NY2016.
- 194.Weaver FM, Smith B, LaVela SL, Evans CT, Ullrich P, Miskevics S, Goldstein B, Strayer J, Burns SP.. Smoking behavior and delivery of evidence- based care for veterans with spinal cord injuries and disorders. J Spinal Cord Med. 2011;34(1):35-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lexicomp online . Lexicomp Online 2019; https://www.wolterskluwercdi.com/lexicomp-online/. Accessed September 2019, 2019.
- 196.Oliva EM, Christopher MLD, Wells D, Bounthavong M, Harvey M, Himstreet J, Emmendorfer T, Valentino M, Franchi M, Goodman F, Trafton JA, Veterans Health Administration Opioid Overdose E, Naloxone Distribution National S, Development W. Opioid overdose education and naloxone distribution: Development of the veterans health administration’s national program. J Am Pharm Assoc (2003). Mar-Apr 2017;57(2S):S168-S179 e164. [DOI] [PubMed] [Google Scholar]
- 197.Sweeney TT, Foote JE.. Treatment of drug and alcohol abuse in spinal cord injury veterans. Int J Addict. Jul 1982;17(5):897-904. [DOI] [PubMed] [Google Scholar]
- 198.Kaner EF, Beyer FR, Muirhead C, Campbell F, Pienaar ED, Bertholet N, Daeppen JB, Saunders JB, Burnand B.. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev. Feb 24 2018;2:CD004148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Barata IA, Shandro JR, Montgomery M, Polansky R, Sachs CJ, Duber HC, Weaver LM, Heins A, Owen HS, Josephson EB, Macias-Konstantopoulos W.. Effectiveness of sbirt for alcohol use disorders in the emergency department: A systematic review. West J Emerg Med. Oct 2017;18(6):1143-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.DiClemente CC, Corno CM, Graydon MM, Wiprovnick AE, Knoblach DJ.. Motivational interviewing, enhancement, and brief interventions over the last decade: A review of reviews of efficacy and effectiveness. Psychology of addictive behaviors: journal of the Society of Psychologists in Addictive Behaviors. Dec 2017;31(8):862-887. [DOI] [PubMed] [Google Scholar]
- 201.Magill M, Ray LA.. Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta- analysis of randomized controlled trials. Journal of studies on alcohol and drugs. Jul 2009;70(4):516-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW.. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. Feb 2008;165(2):179-187. [DOI] [PubMed] [Google Scholar]
- 203.Roozen HG, de Waart R, van der Kroft P.. Community reinforcement and family training: An effective option to engage treatment-resistant substance-abusing individuals in treatment. Addiction. Oct 2010;105(10):1729-1738. [DOI] [PubMed] [Google Scholar]
- 204.Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, Heyman RB, Jaen CR, Kottke TE, Lando HA, Mecklenburg RE, Mullen PD, Nett LM, Robinson L, Stitzer ML, Tommasello A, Villejo L, Wewers ME. Treating tobacco use and dependence: Clinical practice guideline. In: U.S. Department of Health and Human Services PHS, ed. Rockville, MD2000.
- 205.Himstreet J. My tobacco cessation workbook: A resource for veterans. 2014. https://www.mentalhealth.va.gov/quit-tobacco/docs/My-Smoking-Workbook-REVISED-2017-final-508.pdf. Accessed Feb 5, 2019.
- 206.Moore BA, Fiellin DA, Cutter CJ, Buono FD, Barry DT, Fiellin LE, O’Connor PG, Schottenfeld RS.. Cognitive behavioral therapy improves treatment outcomes for prescription opioid users in primary care buprenorphine treatment. Journal of substance abuse treatment. Dec 2016;71:54-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Watkins KE, Ober AJ, Lamp K, Lind M, Setodji C, Osilla KC, Hunter SB, McCullough CM, Becker K, Iyiewuare PO, Diamant A, Heinzerling K, Pincus HA.. Collaborative care for opioid and alcohol use disorders in primary care: The summit randomized clinical trial. JAMA Intern Med. Oct 1 2017;177(10):1480-1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Osilla KC, D’Amico EJ, Lind M, Ober AJ, Watkins KE.. Brief treatment for substance use disorders: A guide for behavioral health providers. Santa Monica, CA: Rand Corporation; 2016: https://www.rand.org/pubs/tools/TL147.html. Accessed February 3, 2019. [Google Scholar]
- 209.Bryant RA, Nickerson A, Creamer M, O’Donnell M, Forbes D, Galatzer-Levy I, McFarlane AC, Silove D.. Trajectory of post-traumatic stress following traumatic injury: 6-year follow-up. Br J Psychiatry. May 2015;206(5):417-423. [DOI] [PubMed] [Google Scholar]
- 210.Johannesson KB, Arinell H, Arnberg FK.. Six years after the wave. Trajectories of posttraumatic stress following a natural disaster. J Anxiety Disord. Dec 2015;36:15-24. [DOI] [PubMed] [Google Scholar]
- 211.Bryant RA. Acute stress disorder in adults: Epidemiology, pathogenesis, clinical manifestations, course, and diagnosis. UpToDate Inc. 2019. https://www-uptodate-com.offcampus.lib.washington.edu. Accessed Accessed on January 10, 2019.
- 212.Stein MB. Approach to treating posttraumatic stress disorder in adults. UpToDate Inc. 2019. https://www-uptodate-com.offcampus.lib.washington.edu. Accessed Accessed on January 10, 2019.
- 213.Bryant RA. Acute stress disorder as a predictor of posttraumatic stress disorder: A systematic review. J Clin Psychiatry. Feb 2011;72(2):233-239. [DOI] [PubMed] [Google Scholar]
- 214.Bryant RA. The current evidence for acute stress disorder. Current psychiatry reports. Oct 13 2018;20(12):111. [DOI] [PubMed] [Google Scholar]
- 215.Rothbaum BO, Davis M.. Applying learning principles to the treatment of post-trauma reactions. Ann N Y Acad Sci. Dec 2003;1008:112-121. [DOI] [PubMed] [Google Scholar]
- 216.Pollock K, Dorstyn D, Butt L, Prentice S.. Posttraumatic stress following spinal cord injury: A systematic review of risk and vulnerability factors. Spinal Cord. Sep 2017;55(9):800-811. [DOI] [PubMed] [Google Scholar]
- 217.Hatcher MB, Whitaker C, Karl A.. What predicts post-traumatic stress following spinal cord injury? Br J Health Psychol. Sep 2009;14(Pt 3):541-561. [DOI] [PubMed] [Google Scholar]
- 218.Cao Y, Li C, Newman S, Lucas J, Charlifue S, Krause JS.. Posttraumatic stress disorder after spinal cord injury. Rehabil Psychol. May 2017;62(2):178-185. [DOI] [PubMed] [Google Scholar]
- 219.Etingen B, Locatelli SM, Miskevics S, LaVela SL.. Examining the relationship between post-traumatic stress disorder and social participation among veterans with spinal cord injuries and disorders. Disabil Rehabil. Nov 2018;40(22):2637-2643. [DOI] [PubMed] [Google Scholar]
- 220.American College of Surgeons CoT . Statement on post-traumatic stress disorder in adults. 2018; https://www.facs.org/about-acs/statements/109-adult-ptsd. Accessed February 19, 2019, 2019. [Google Scholar]
- 221.Hanley J, deRoon-Cassini T, Brasel K.. Efficiency of a four-item posttraumatic stress disorder screen in trauma patients. J Trauma Acute Care Surg. Oct 2013;75(4):722-727. [DOI] [PubMed] [Google Scholar]
- 222.Warren AM, Reynolds M, Driver S, Bennett M, Sikka S.. Posttraumatic stress symptoms among spinal cord injury patients in trauma: A brief report. Top Spinal Cord Inj Rehabil. Summer 2016;22(3):203-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Hunt JC, Sapp M, Walker C, Warren AM, Brasel K, deRoon-Cassini TA.. Utility of the injured trauma survivor screen to predict ptsd and depression during hospital admission. J Trauma Acute Care Surg. Jan 2017;82(1):93-101. [DOI] [PubMed] [Google Scholar]
- 224.Martz E, Livneh H, Priebe M, Wuermser LA, Ottomanelli L.. Predictors of psychosocial adaptation among people with spinal cord injury or disorder. Arch Phys Med Rehabil. Jun 2005;86(6):1182-1192. [DOI] [PubMed] [Google Scholar]
- 225.Krause JS, Saunders LL, Newman S.. Posttraumatic stress disorder and spinal cord injury. Arch Phys Med Rehabil. Aug 2010;91(8):1182-1187. [DOI] [PubMed] [Google Scholar]
- 226.Schonenberg M, Reimitz M, Jusyte A, Maier D, Badke A, Hautzinger M.. Depression, posttraumatic stress, and risk factors following spinal cord injury. Int J Behav Med. Feb 2014;21(1):169-176. [DOI] [PubMed] [Google Scholar]
- 227.Spoont MR, Williams JW, Jr., Kehle-Forbes S, Nieuwsma JA, Mann-Wrobel MC, Gross R.. Does this patient have posttraumatic stress disorder?: Rational clinical examination systematic review. JAMA. Aug 4 2015;314(5):501-510. [DOI] [PubMed] [Google Scholar]
- 228.Geier TJ, Hunt JC, Nelson LD, Brasel KJ, deRoon-Cassini TA.. Detecting ptsd in a traumatically injured population: The diagnostic utility of the ptsd checklist for dsm-5. Depress Anxiety. Feb 2019;36(2):170-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, Kaloupek DG, Schnurr PP, Kaiser AP, Leyva YE, Tiet QQ.. The primary care ptsd screen for dsm-5 (pc-ptsd-5): Development and evaluation within a veteran primary care sample. J Gen Intern Med. Oct 2016;31(10):1206-1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Utzon-Frank N, Breinegaard N, Bertelsen M, Borritz M, Eller NH, Nordentoft M, Olesen K, Rod NH, Rugulies R, Bonde JP.. Occurrence of delayed-onset post-traumatic stress disorder: A systematic review and meta-analysis of prospective studies. Scand J Work Environ Health. May 1 2014;40(3):215-229. [DOI] [PubMed] [Google Scholar]
- 231.Clark C, Classen CC, Fourt A, Shetty M.. Treating the trauma survivor: An essential guide to trauma- informed care. New York, NY: Taylor Francis; 2015. [Google Scholar]
- 232.Harris M, Fallot RD, eds. New directions for mental health services. Using trauma theory to design service systems. San Francisco, CA: Josey-Bass; 2001. [Google Scholar]
- 233.Williamson LF, Kautz DD.. Trauma-informed care is the best clinical practice in rehabilitation nursing. Rehabilitation Nursing. 2018;42(2):73-80. [DOI] [PubMed] [Google Scholar]
- 234.The Management of Posttraumatic Stress Disorder Work Group . Va/dod clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. In: Department of Veterans Affairs DoD, ed. Version 3.0 ed2017.
- 235.Kliem S., K C.. Prevention of chronic ptsd with early cognitive behavioral therapy. A meta- analysis using mixed-effects modeling . Behaviour research and therapy. 2013;51(11):753-761. [DOI] [PubMed] [Google Scholar]
- 236.Roberts NP, Kitchiner NJ, Kenardy J, Bisson J.. Multiple session early psychological interventions for the prevention of post-traumatic stress disorder. Cochrane Database Syst Rev. Jul 8 2009(3):CD006869. [DOI] [PubMed] [Google Scholar]
- 237.Kornor H, Winje D, Ekeberg O, Weisaeth L, Kirkehei I, Johansen K, Steiro A.. Early trauma-focused cognitive-behavioural therapy to prevent chronic post-traumatic stress disorder and related symptoms: A systematic review and meta-analysis. BMC Psychiatry. Sep 19 2008;8:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Shalev AY, Ankri Y, Israeli-Shalev Y, Peleg T, Adessky R, Freedman S.. Prevention of posttraumatic stress disorder by early treatment: Results from the jerusalem trauma outreach and prevention study. Arch Gen Psychiatry. Feb 2012;69(2):166-176. [DOI] [PubMed] [Google Scholar]
- 239.Argolo FC, Cavalcanti-Ribeiro P, Netto LR, Quarantini LC.. Prevention of posttraumatic stress disorder with propranolol: A meta-analytic review. Journal of psychosomatic research. Aug 2015;79(2):89-93. [DOI] [PubMed] [Google Scholar]
- 240.DeVivo MJ, Black KJ, Richards JS, Stover SL.. Suicide following spinal cord injury. Paraplegia. Nov 1991;29(9):620-627. [DOI] [PubMed] [Google Scholar]
- 241.Cao Y, Massaro JF, Krause JS, Chen Y, Devivo MJ.. Suicide mortality after spinal cord injury in the united states: Injury cohorts analysis. Arch Phys Med Rehabil. Feb 2014;95(2):230-235. [DOI] [PubMed] [Google Scholar]
- 242.McCullumsmith CB, Kalpakjian CZ, Richards JS, Forchheimer M, Heinemann AW, Richardson EJ, Wilson CS, Barber J, Temkin N, Bombardier CH, Fann JR, Investigators P.. Novel risk factors associated with current suicidal ideation and lifetime suicide attempts in individuals with spinal cord injury. Arch Phys Med Rehabil. May 2015;96(5):799-808. [DOI] [PubMed] [Google Scholar]
- 243.Nam HS, Kim HR, Ha TH, Shin HI.. Suicidal ideation in korean persons with spinal cord injury. Spinal Cord. Oct 2013;51(10):789-793. [DOI] [PubMed] [Google Scholar]
- 244.Charlifue SW, Gerhart KA.. Behavioral and demographic predictors of suicide after traumatic spinal cord injury. Arch Phys Med Rehab. Jun 1991;72(7):488-492. [PubMed] [Google Scholar]
- 245.Savic G, DeVivo MJ, Frankel HL, Jamous MA, Soni BM, Charlifue S.. Suicide and traumatic spinal cord injury-a cohort study. Spinal Cord. Jan 2018;56(1):2-6. [DOI] [PubMed] [Google Scholar]
- 246.Louzon SA, Bossarte R, McCarthy JF, Katz IR.. Does suicidal ideation as measured by the phq-9 predict suicide among va patients? Psychiatr Serv. May 1 2016;67(5):517-522. [DOI] [PubMed] [Google Scholar]
- 247.Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ.. The columbia-suicide severity rating scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. Dec 2011;168(12):1266-1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Na PJ, Yaramala SR, Kim JA, Kim H, Goes FS, Zandi PP, Vande Voort JL, Sutor B, Croarkin P, Bobo WV.. The phq-9 item 9 based screening for suicide risk: A validation study of the patient health questionnaire (phq)-9 item 9 with the columbia suicide severity rating scale (c-ssrs). J Affect Disord. May 2018;232:34-40. [DOI] [PubMed] [Google Scholar]
- 249.Rudd MD. Suicide warning signs in clinical practice. Current psychiatry reports. Feb 2008;10(1):87-90. [DOI] [PubMed] [Google Scholar]
- 250.Assessment and The Management of Risk for Suicide Working Group. Va/dod clinical practice guideline for assessment and management of patients at risk for suicide. In: Department of Veterans Affairs DoD, ed. Version 1.0 ed2013.
- 251.Assessment and The Management of Risk for Suicide Working Group. Va/dod clinical practice guideline for assessment and management of patients at risk for suicide. In: Department of Veterans Affairs DoD, ed. Version 2.0 ed2019.
- 252.Tarrier N, Taylor K, Gooding P.. Cognitive- behavioral interventions to reduce suicide behavior: A systematic review and meta-analysis. Behav Modif. Jan 2008;32(1):77-108. [DOI] [PubMed] [Google Scholar]
- 253.Hooley JM, Franklin JC, Nock MK.. Chronic pain and suicide: Understanding the association. Curr Pain Headache Rep. 2014;18(8):435. [DOI] [PubMed] [Google Scholar]
- 254.Ilgen MA, Bohnert AS, Ganoczy D, Bair MJ, McCarthy JF, Blow FC.. Opioid dose and risk of suicide. Pain. May 2016;157(5):1079-1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Muller R, Landmann G, Bechir M, Hinrichs T, Arnet U, Jordan X, Brinkhof MWG.. Chronic pain, depression and quality of life in individuals with spinal cord injury: Mediating role of participation. J Rehabil Med. Jun 28 2017;49(6):489-496. [DOI] [PubMed] [Google Scholar]
- 256.Yuodelis-Flores C, Ries RK.. Addiction and suicide: A review. Am J Addict. Mar 2015;24(2):98-104. [DOI] [PubMed] [Google Scholar]
- 257.Stanford RE, Soden R, Bartrop R, Mikk M, Taylor TK.. Spinal cord and related injuries after attempted suicide: Psychiatric diagnosis and long-term follow-up. Spinal Cord. Jun 2007;45(6):437-443. [DOI] [PubMed] [Google Scholar]
- 258.Bryson CN, Cramer RJ, Schmidt AT.. Traumatic brain injury and lifetime suicidality: Applying the interpersonal-psychological theory perspective. Death Stud. Aug 2017;41(7):399-405. [DOI] [PubMed] [Google Scholar]
- 259.Madsen T, Erlangsen A, Orlovska S, Mofaddy R, Nordentoft M, Benros ME.. Association between traumatic brain injury and risk of suicide. JAMA. Aug 14 2018;320(6):580-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Gould MS, Lake AM, Galfalvy H, Kleinman M, Munfakh JL, Wright J, McKeon R.. Follow-up with callers to the national suicide prevention lifeline: Evaluation of callers’ perceptions of care. Suicide Life Threat Behav. Feb 2018;48(1):75-86. [DOI] [PubMed] [Google Scholar]
- 261.Stanley B, Brown GK, Brenner LA, Galfalvy HC, Currier GW, Knox KL, Chaudhury SR, Bush AL, Green KL.. Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry. Sep 1 2018;75(9):894-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Lewiecki EM, Miller SA.. Suicide, guns, and public policy. Am J Public Health. Jan 2013;103(1):27-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Shenassa ED, Rogers ML, Spalding KL, Roberts MB.. Safer storage of firearms at home and risk of suicide: A study of protective factors in a nationally representative sample. J Epidemiol Community Health. Oct 2004;58(10):841-848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Duberstein PR, Conwell Y, Conner KR, Eberly S, Evinger JS, Caine ED.. Poor social integration and suicide: Fact or artifact? A case-control study. Psychol Med. Oct 2004;34(7):1331-1337. [DOI] [PubMed] [Google Scholar]
- 265.Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, Wallace R.. Risk factors for late-life suicide: A prospective, community-based study. Am J Geriatr Psychiatry. Jul-Aug 2002;10(4):398-406. [PubMed] [Google Scholar]
- 266.Conwell Y. Suicide later in life: Challenges and priorities for prevention. Am J Prev Med. Sep 2014;47(3 Suppl 2): S244-250. [DOI] [PubMed] [Google Scholar]
- 267.Whitlock J, Wyman PA, Moore SR.. Connectedness and suicide prevention in adolescents: Pathways and implications. Suicide Life Threat Behav. Jun 2014;44(3):246-272. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.