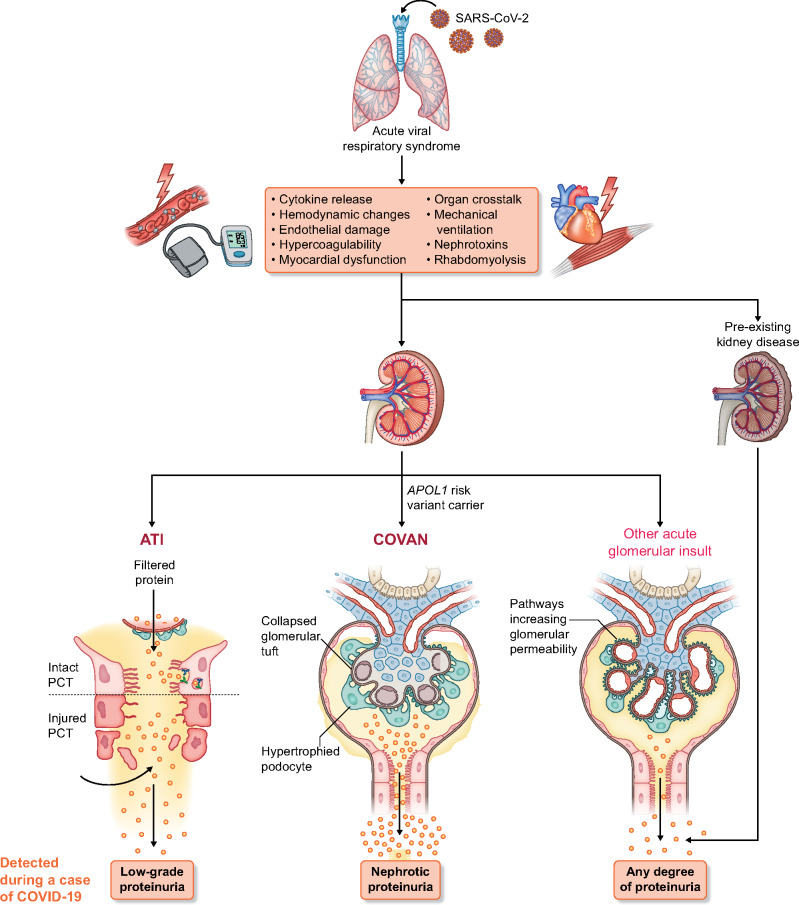
FIGURE 1:
Pathogenesis of proteinuria in COVID-19. Individuals infected with SARS-CoV-2 develop an acute respiratory illness that is followed by multiple pathological mechanisms that may lead to the development of AKI. Low-grade proteinuria can be observed in COVID-19 presenting with a subclinical form of AKI, i.e. without elevation of the serum creatinine concentration. The most common type of AKI in COVID-19 is ATI. In cases of ATI, low-grade proteinuria can also be detected, presumably resulting from damage to the proximal convoluted tubule, when detached and sloughed tubular cells cannot reabsorb the filtered protein that is normally reclaimed through the apical endocytic apparatus. Susceptible individuals of African ancestry who are carriers of the APOL1 high-risk genotype can acquire collapsing glomerulopathy when they are infected with COVID-19 (i.e. COVAN) and present with nephrotic-range proteinuria and AKI. Systemic inflammatory response has been linked to an increase in glomerular permeability. Other acute glomerular insults can occur in patients with COVID-19 (e.g. thrombotic microangiopathy). Preexisting CKD can lead to detection of proteinuria in a patient with COVID-19 and the magnitude of the proteinuria in those cases could be of any degree, stable or worse than its baseline value.