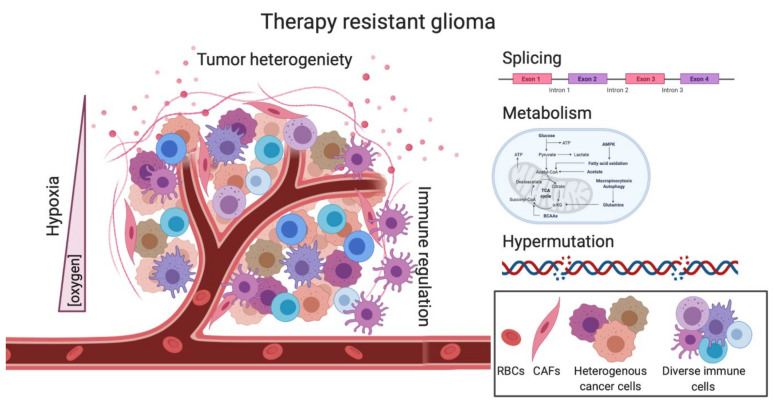
Figure 3.
Complex pathways underlie the therapeutic resistance of GBM. The decrease of oxygen within in the tumor can facilitate hypoxia-induced signaling which can render cells less sensitive to treatment. Tumor heterogeneity can complicate therapeutic response as not all clones are targeted equally by standard treatments. Immune regulation is severely dampened in GBM, creating a “cold” TME. Splicing changes via RBPs or splicing factors can affect isoform outcome leading to dysregulated AS. Metabolic changes induced by TMZ or RT are able to change metabolism in both the tumor cells as well as the TME, creating a therapeutic-resistant microenvironment. TMZ-induced hypermutation can create a hypermutator state in which patient outcome is correlated with a worse overall survival, as compared to other cancers. Overall, many pathways play a role in GBM therapeutic resistance, and all should be investigated for better second-line treatments. RBPs, RNA binding proteins; AS, Alternative splicing; RBCs, red blood cells, CAFs, cancer-associated fibroblasts.