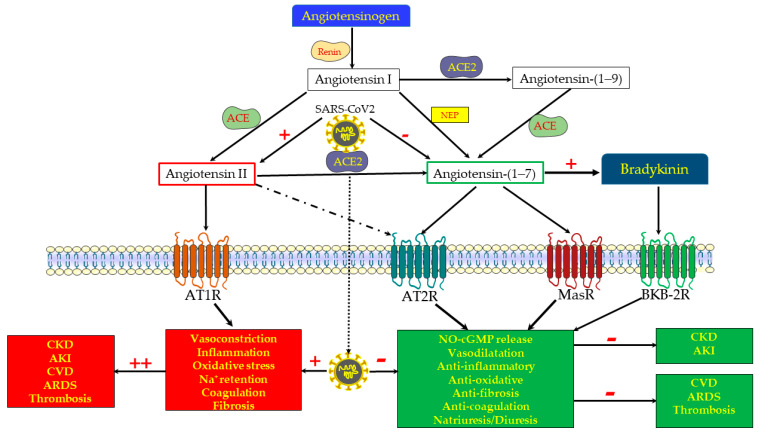
Figure 1.
Biosynthesis and functional scheme of the renin–angiotensin system (RAS). The classical RAS consists of the protease renin, which is secreted from renal juxtaglomerular cells adjacent to the afferent arteriole, and which acts on the circulating precursor angiotensinogen to generate angiotensin (Ang) I, an inactive 10 amino acid (aa) peptide. The latter is converted by the angiotensin-converting enzyme (ACE) to Ang II, an 8 aa active peptide. Ang II is the main effector component of the RAS, as evident from its potent action, stimulating vasoconstriction, oxidative stress, Na+ retention, inflammation, fibrosis and coagulation, all mediated by the AT1 receptor (AT1R). However, Ang II also acts via AT2R, which is part of the “depressor” or protective arm of RAS, as made evident by its oppositely effects on the various target organs, including the kidney, heart, and vasculature. ACE2 is a peptidase located on cell membranes in various tissues, including the kidneys, where it promotes the proteolytic cleavage of the octapeptide Ang II with the formation of Ang-(1-7). Alternatively, Ang 1-7 can be generated by a preliminary cleavage of the decapeptide Ang I with the formation of Ang 1-9, followed by the removal of two additional amino acids by ACE. Ang-(1-7) may also be formed directly from angiotensinogen, following proteolytic cleavage by neprilysin (NEP). Ang-(1-7) acts via the Mas receptor (Mas-R) to stimulate nitric oxide (NO) and cGMP, exerting vasodilation and attenuating inflammation, oxidative stress, pro-fibrotic processes, coagulopathy, and probably permeating diuresis and natriuresis. Ang-(1-7) also modifies the kinin pathways, promoting bradykinin action through its type B2 receptors. Since AT2R and MasR exert comparable physiologic responses, mediated by the same downstream mechanisms, namely cGMP and NO, it is assumed that the Ang-(1-7) actions are also attributed to its binding to AT2R (a receptor activated also by Ang II). Thus, the ACE2/Ang-(1-7)/MasR + AT2R axis forms an under-recognized beneficial arm of the RAS, that in concert with bradykinin/bradykinin type B2 receptors counterbalances the delirious arm, namely the ACE/Ang II/AT1R axis, which is involved in the pathogenesis of various cardiovascular, pulmonary, renal and hematological diseases. The COVID-19 disease is characterized by the depletion of ACE2 and Ang-(1-7) along unleashed ACE/Ang II/AT1R, conceivably playing a central role in the devastating cytokine storm, oxidative stress, coagulopathy and fibrosis that characterizes this disorder. In light of their beneficial effects on the progression of cardiovascular, pulmonary and renal diseases, ACE2 repletion and the administration of Ang-(1-7) constitute the therapeutic options currently tested in the management of severe COVID-19 disease, with the expectation of renal vasodilation and the attenuation of oxidative stress, inflammation, tissue damage and subsequent fibrosis. Although most outcomes indicate that triggering the ACE2/Ang-(1-7)/MasR axis may be nephroprotective in the setup of AKI, there is contradicting evidence that under certain conditions, it may accelerate renal damage in CKD and AKI.