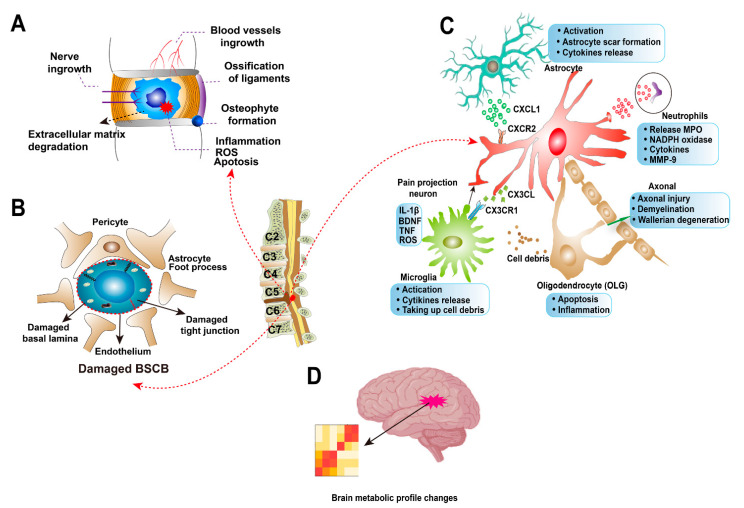
Figure 3.
Molecular features of degenerative cervical myelopathy (DCM). (A) The hallmarks of cervical disc degeneration. Compared to healthy intervertebral disc, the degenerative disc has increased blood vessel and neuronal ingrowth. Increased inflammation, reactive oxygen species (ROS) and cell apoptosis result in extracellular matrix degradation. The cartilage endplate may be calcified, and osteophytes form on the adjacent vertebral bones. Ossification of the posterior longitudinal ligament (OPLL) can also be found in degenerative cervical spines. (B) Blood–spinal cord barrier (BSCB) is disrupted in DCM, with the features of damaged basal lamina and tight junction. (C) The roles of cells types in spinal cord during DCM. Astrocyte participates in scar formation in spinal cord; and activated astrocytes can release CXCL1 to interact with CXCR2 receptor on neurons, inducing descending neuron degeneration in spinal cord. CX3CL/CX3CR1 interaction between microglia and neuron regulates neuroinflammation in DCM. Microglia can also take up cell debris from other cells, such as apoptosis oligodendrocytes (OLG). Infiltrating neutrophils release myeloperoxidase (MPO), nicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase) and other cytokines in the microenvironment. Neutrophils can also express Matrix metalloproteinase (MMP)-9 as a strong pro-inflammatory molecule. (D) The brain metabolic profile was found to change in DCM patients.