ABSTRACT
In the rapidly progressing field of telemedicine, there is a multitude of evidence assessing the effectiveness and financial costs of telemedicine projects; however, there is very little assessing the environmental impact despite the increasing threat of the climate emergency. This report provides a systematic review of the evidence on the carbon footprint of telemedicine. The identified papers unanimously report that telemedicine does reduce the carbon footprint of healthcare, primarily by reduction in transport-associated emissions. The carbon footprint savings range between 0.70–372 kg CO2e per consultation. However, these values are highly context specific. The carbon emissions produced from the use of the telemedicine systems themselves were found to be very low in comparison to emissions saved from travel reductions. This could have wide implications in reducing the carbon footprint of healthcare services globally. In order for telemedicine services to be successfully implemented, further research is necessary to determine context-specific considerations and potential rebound effects.
KEYWORDS: telemedicine, sustainability, e-health, carbon footprint
Introduction
Telemedicine is the use of information and communications technologies (ICT) within the realm of healthcare. The scope of services that fall within the remit of telemedicine is ambiguous. This paper uses the World Health Organization definition of telemedicine, defined as the use of ICT ‘for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers’.1
The applications of telemedicine can be categorised according to type of interaction (clinician-to-patient or clinician-to-clinician) or timing (asynchronous or synchronous).1 Asynchronous involves sending pre-recorded information between individuals, whereas synchronous is real-time data transmission. The data may be transmitted via a variety of media, such as audio, video or text. This paper will focus on all forms of telemedicine involving direct patient care where the carbon footprint of the telemedicine project is compared to a face-to-face (FTF) scenario.
Telemedicine is a recent development within healthcare. In this decade, there has been an explosion in telemedicine research, focusing on specific medical specialties. The reported advantages include lower financial costs, high patient satisfaction, better rural access, decreased waiting times and fewer missed appointment.2–7 There is less available evidence from primary care; however, there are positive findings in primary care chronic disease management.8–10 The main disadvantages are erosion of the clinician–patient relationship and concerns around quality of care. In terms of clinician–patient relationship, this concern arises particularly from elderly patients and healthcare providers themselves; however, acceptance has been shown to be increasing.6,11,12 There are mixed reports on the quality of care provided by telemedicine; some sources report improved or maintained standards of care, whereas others found a reduction in quality of care compared to FTF scenarios.9,13–19
In spite of the extensive research into the effectiveness, cost and perceptions of telemedicine, there have been few contributions assessing the environmental impact; despite many previous studies stating a reduction in travel time and the increasing awareness of environmental concerns within society.7,20–23
In a world where climate change has been named as one of the biggest threats to human health, the healthcare sector continues to significantly contribute to greenhouse gas (GHG) emissions.24 Health Care Without Harm estimated the global carbon footprint of healthcare to be 2 gigatons of carbon dioxide equivalents (CO2e) in 2014, equating to 4.4% of global net emissions; transport contributed 7% of this total.25
From a UK perspective, the estimated carbon footprint of the NHS in England was 25.0 megatons of CO2e in 2019.26 The NHS launched the ‘For a Greener NHS’ programme in January 2020, and has produced a Net Zero Report outlining the interventions needed to reach its target of being net carbon zero by 2050.26 Travel accounts for 10% of NHS’ GHG emissions and, in 2008, an estimated 5% of all road travel was attributable to the NHS.26,27 Telemedicine provides an exciting prospect for potential reduction in the NHS’ contribution to climate change. A 2018 NHS Midlands and Lancashire commissioned report estimated that the West Midlands could reduce emissions by 533,535 kg CO2e annually by shifting 15% of all hospital follow-up consultations to telemedicine.28
Methods
A review of the published works relating to the carbon footprint of telemedicine was carried out using the databases MEDLINE, Embase and Scopus. The search strategy is documented in supplementary material S1, Table S1.
The searches were carried out by two researchers between 10 May 2020 and 14 May 2020, and there were no limitations in terms of publication date. The publications were then screened for duplications. The inclusion criterium was for the publication to be a primary research study considering the carbon footprint of telemedicine programmes. The exclusion criteria were:
publications not involving direct patient care
veterinary or dentistry publications
non-English language publications
publications modelling theoretical carbon footprint savings from future adoption of telemedicine
publications without primary data.
There were no limitations on research methods. After having been screened for suitability, the publications were divided into three categories for analysis: telephone synchronous, video synchronous and asynchronous. The telephone consultations were not divided based on VoIP (Voice over Internet Protocol) versus mobile telephone or landline calls, since this information was not available in all of the publications.
In order to compare the studies, the total CO2e reductions were divided by the number of consultations to calculate emissions reduction per consultation. Travel distance saved was compared with the carbon footprint reduction per consultation, and linear regressions were used to quantify the strength of this correlation.
Results
Study selection
The PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) was used to screen the literature, illustrated in Fig 1.29
Fig 1.
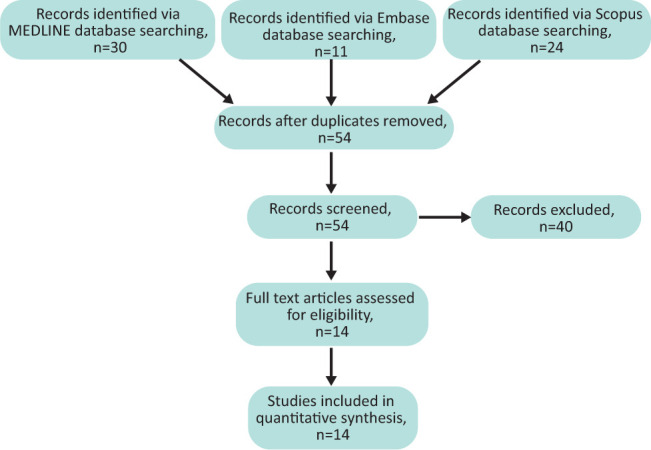
PRISMA diagram showing literature search results.
This literature search produced 65 results, 11 of which were found to be duplicates. After assessment against exclusion and inclusion criteria, 14 of these publications were found to be relevant to the assigned question.
Study comparison
Fig 2 illustrates the carbon footprint saved versus the average travel distance saved (Table 1). This positive correlation highlights that the carbon footprint saving is primarily due to travel reduction. The blue trendline considers only the studies which measured road travel, and there is strong positive correlation (r2=0.9973; p=3.78 × 10-14). The results of this linear regression are shown in supplementary material S1, Table S2. The two studies examining air travel do not appear to fit this pattern (shown in yellow). The strong congruence shown across road travel studies gives confidence in the reliability and thoroughness of the literature.
Fig 2.
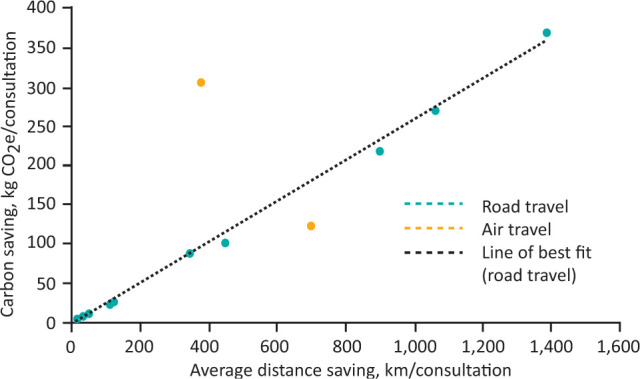
Carbon footprint against travel distance savings of telemedicine interventions.
Table 1.
Distance and carbon savings of telemedicine studies
| Study | Study region | Average distance saving (km/consultation) | Carbon footprint (kg CO2e/consultation) |
|---|---|---|---|
| Beswick et al (2014) | California, USA | 1,387 | 372 |
| Connor A et al (2011) | Warwickshire, UK | 39.3 | 8.05 |
| Connor MJ et al (2019) | London, UK | 15.0 | 2.93 (car) 0.70 (underground train) |
| Dorrian et al (2009) | Scotland, UK | 698 | 123 (air) |
| Dullet et al (2017) | California, USA | 447 | 102 |
| Holmner et al (2014) | Västerbotten, Sweden | 346 | 87.4 (Leduc LCA model) 176 (Lenzen LCA model) |
| Masino et al (2010) | Ontario, Canada | 901 | 220 |
| Miah et al (2019) | London, UK | 18.2 | 3.55 (car) 0.86 (underground train) |
| Oliveira et al (2013) | Alentejo, Portugal | 111 | 22.0 |
| Paquette et al (2019) | Michigan, USA | 50.2 | 11.2 |
| Robinson et al (2017) | Texas, USA | 1,061 | 271 |
| Vidal-Alaball et al (2019) | Catalonia, Spain | 21.3 | 3.25 |
| Whetten et al (2019) | New Mexico, USA | 381 | 306 (air) |
| Wootton et al (2010) | Scotland, UK | 126 | 26.9 |
LCA = life cycle assessment.
Telephone synchronous
There were four examples found of telephone synchronous papers. Two studies from the UK assessed a virtual urology clinic in London.30,31 Both studies measured carbon footprints by the distance saved from patients’ home addresses to the hospital in which the FTF appointment would have otherwise occurred. They calculated two different scenarios; assuming every patient either drove using a 1,800 cc petrol car or took the underground train. In Fig 2, the values for the car scenarios were used since this is the mode of transport primarily used in the other studies. Miah et al found an average distance saving of 18.2 km per patient, correlating with savings per consultation of 0.86 kg CO2e (underground scenario) and 3.55 kg CO2e (car scenario).30 MJ Connor et al assessed 1,008 patients and found an average saving of 15.0 km per patient, correlating to a carbon footprint reduction of 0.70 kg CO2e (underground scenario) and 2.93 kg CO2e (car scenario).31 It is unknown whether the individual patients overlapped between these two studies due to their overlapping time frames. This is a relatively low CO2e saving due to short travel distances in a densely populated region.
A Connor et al assessed telephone follow-up appointments post-renal transplant surgery.32 They examined 30 patients attending two consecutive telephone appointments. Calculating travel distances from home addresses, also taking into account mode of transport and vehicle specifications; the mean saving was 39.3 km, equating to 8.05 kg CO2e per consultation.
Robinson et al assessed the environmental savings from pre-surgical telephone consultations in Texas.33 There was only one tertiary centre providing this surgery, so large distances were travelled for surgical eligibility. Using ZIP codes, this study found that the average mileage saved was 1,061 km. They made the assumption of an average car, so not accounting for other methods of transport and vehicle specifications. The reduction in carbon footprint was calculated as 271 kg CO2e per consultation. This prospective study found there to be a correlation between increased travel distance and increased likelihood of choosing telemedicine over FTF appointments.
One limitation of these telephone synchronous studies is that they do not assess the carbon footprint of the running of the telephone service, which would have to be subtracted from the CO2e estimation.
Video synchronous
There were nine examples of video synchronous telemedicine. Since videoconferencing equipment is more specialised and therefore less common within people's homes, many of the video consultations occurred at an intermediate telemedicine site. Three of these sources additionally accounted for the carbon footprint of the telemedicine equipment of both of the clinician and patient devices.
Holmner et al assessed videoconferencing for telerehabilitation in Sweden. As well as looking at distances from the patients’ homes to the hospital, a comprehensive life cycle assessment (LCA) was carried out to estimate the carbon footprint of the videoconferencing equipment.34 This was a ‘cradle to grave’ assessment based on the model in Ong et al, which included energy consumption of equipment during the use-phase as well as emissions generated during design, manufacturing and disposal of equipment.35 LCAs of car travel were also included, based on average characteristics of European cars. From the 238 appointments at the hand and plastics surgery clinic, a total travel distance of 82,310 km was saved, giving a range of 87.4–176 kg CO2e per consultation saved using telemedicine. This range was due to the use of two different LCAs of vehicles. In Fig 2, 87.4 kg CO2e was used since this value arises from the most recent LCA by Leduc et al, reflecting recent increases in energy efficiency of cars.36 An important conclusion of this paper is that the carbon footprint of the telemedicine equipment is small compared to the carbon footprint of travel, at 1.86–8.43 kg CO2e per hour consultation.
Two additional studies consider the energy usage of the videoconferencing equipment, but do not include LCAs of emissions produced during production and disposal of equipment. Masino et al looked at telemedicine appointments in Ontario using estimated distances from the patient address to the telemedicine site, as compared with the hospital.37 There was a mean saving of 901 km per consultation. The environmental cost of the telemedicine equipment was found to be very low, at 0.04 kg CO2e per 1-hour consultation. The total GHG saving was 220 kg CO2e per consultation. Whetten et al produced a similar result of 0.052 kg CO2e per 1-hour consultation.38 This study looked at neurology video consultations from 12 rural hospital sites to a large hospital in New Mexico, which avoided unnecessary helicopter air ambulance flights. CH4 (methane), CO2 and N2O (nitrous oxide) emissions were used to calculate CO2e. This saved 381 km per consultation, equating to 306 kg CO2e.
Dullet et al investigated the carbon footprint of University of California Davis Health System's (UCDHS) outpatient telemedicine service.39 There were 157 telemedicine sites across California from which these services could be accessed. Average one-way distance to telemedicine sites was 27.4 km compared with a potential 251 km to the UCDHS. A total of 1,969,000 kg CO2e was saved over 19,246 consultations, corresponding to 102 kg CO2 per consultation. A similar large-scale study in Portugal by Oliveira et al assessed 20,824 video consultations.40 Estimates of travel distances were made using survey data on distance travelled and mode of transport. It concluded that without video consultations, patients would have travelled an extra 2,313,819 km, increasing the carbon footprint by 455,000 kg CO2e (22 kg CO2e per consultation). This gave a retrospectively calculated reduction of 95% in GHG emissions.
Paquette et al assessed video consultations from one vascular surgeon in Michigan.41 Using average vehicle emissions, the average distance saved travelling to the telemedicine site compared with the hypothetical distance to the hospital was calculated to be 50.2 km per consultation, equating to 11.2 kg CO2e.
Wootton et al assessed a videoconferencing tool used in nurse-led minor injuries units in Grampian, Scotland.42 This allowed clinicians to ask for advice from emergency doctors in Aberdeen, preventing unnecessary transfer in 90–95% of cases. This was estimated to avoid 260,000 km of travel, or 26.9 kg CO2e per consultation.
Two studies investigated the use of videoconferencing for head and neck cancer assessment.35,36 In Dorrian et al, doctors on the Shetland Islands performed laryngoscopy which was viewed live by a consultant in Aberdeen.43 The carbon footprint savings were calculated from both the road and air segments of the journey (a 698 km round-trip) estimated to reduce emissions by 123 kg CO2e per consultation. In Beswick et al, 21 patients were assessed for head and neck cancer over 39 videoconferences.44 This occurred with healthcare professionals at the patient's home, providing real time nasopharyngoscopy, which was viewed live by a surgeon at a hospital in California. The round-trip distance saved was 1,387 km road travel per consultation, equating to 372 kg CO2e. One limitation in both studies is that the travel distances of the healthcare professionals were not accounted for.
Non-synchronous
The literature search produced only one example of non-synchronous telemedicine. Vidal-Alaball et al looked at primary care referrals to telemedicine services in Catalan.45 Rather than using exact patient addresses, distances were calculated from the primary care centres to secondary care centres and assumed every patient travelled by car. The mean distance saved was 21.3 km, equating to 3.25 kg CO2e per patient.
Discussion
The studies in this review consistently report that telemedicine reduces the carbon footprint of healthcare as compared with FTF scenarios. This reported benefit was primarily through travel-associated savings which greatly outweighed the carbon footprint of the telemedicine equipment. The savings ranged from 0.70 to 372 kg CO2e per consultation but were highly context specific.
It is important to consider the differences between media sources within telemedicine. Videoconferencing has a higher energy consumption compared with telephone consultations, so it can be assumed that the carbon footprint would be higher. An advantage of telephone appointments is that the majority of people worldwide have access to a telephone, whereas videoconferencing may require travel to a telemedicine site.46 However, comparisons between the two media sources have found videoconferencing to be safer, with more favourable outcomes and better clinician decision making.47–50
The carbon footprint savings were highly dependent on the inter-related factors of medical specialty, geography and time. The higher the level of specialisation seemed to correspond with a greater reduction in travel, since specialised centres serviced a wider geographic region. For example, in Beswick et al, there was only one tertiary centre providing this service for veterans in south-west USA, therefore travel reductions were large.44 This implies that the extent of carbon footprint reduction will be dependent on the population density of the region, as well as on transport infrastructure.
There are limitations arising from variance in methodology within these research papers. There is variation in how travel and carbon footprint has been modelled. In terms of modes of transport, the majority of studies assumed the mode of transport to be a car, with assumed average characteristics. Considering the air travel scenarios, emissions from flights are highly dependent on the size and type of aircraft. The primary source of GHGs from travel is carbon dioxide, which was consistently accounted for in every study. However, some studies provided a more comprehensive assessment of GHG, also assessing CH4 and N2O.37,38 Another factor to consider is double consulting; a situation where a teleconsultation is inadequate, necessitating the need for a further FTF consultation. This scenario increases the net carbon emissions. Future studies should aim to incorporate carbon emissions from subsequent FTF consultations in order to more accurately represent net carbon savings.
There is a limitation in that the majority of studies did not include the carbon footprint of the telemedicine service; but when assessed, this was found to be low in comparison to travel carbon footprint. The most comprehensive LCA, carried out by Holmner et al, estimated that the studied telerehabilitation service became carbon cost-effective where the patient travel distance was over 7.2 km.34 This again highlights the variance in net savings depending on travel distance; however, all of the studies analysed in this paper had a travel distance of over 7.2 km. Fig 2 highlights the low significance of the telemedicine carbon footprint, since there was congruence between road travel studies regardless of whether they included this aspect or not. Another limitation is that the studies assumed that every telemedicine appointment would otherwise have taken place at the specified hospital. This may not have been the case; patients may have otherwise been referred to less specialised local hospitals or may have chosen not to attend an appointment due to large travel distances and costs. Therefore, the reductions in travel may be an overestimate.
This review assessed only the direct carbon footprint of telemedicine; there may be rebound effects to consider. It has not been determined what the time and money saved by individuals and healthcare organisations would have been used for instead. If these alternate activities were high carbon generating, then there is a risk that much of the savings could be undermined. However, since there is likely to be an increasing drive to decarbonise across all sectors, this argument should not be an impediment against reducing the carbon footprint of healthcare services. There are other environmental aspects in addition to carbon footprint which have not been considered in this review; for example, some of the studies additionally quantified the production of non-GHG gases which may be additionally harmful to health.37–39,41,45 Furthermore, reductions in car travel could reduce health harms from road traffic accidents and encourage increased walking and cycling.
There are additionally limitations within this systematic review. Although a comprehensive search strategy was used, it is possible that not all relevant studies were found. As this subject sits across disciplines of healthcare, technology and environmental sustainability, ensuring exhaustive pick up is challenging. Due to the limited number of relevant studies found, it was not possible to scrutinise and exclude on quality of methodology. There is a limitation in the small study sample size; however, the strong congruence found in the data may suggest reliability of these sources.
The implications of this paper will be dependent on the country being considered. Using the UK as an example, telemedicine could greatly reduce travel-associated emissions. In 2011–2012, there was found to be an average of 8.7 km one-way from homes to the nearest emergency centre in England (17.6 km in rural areas compared with 7.6 km in urban areas).51 In 2016–2017, 93.9 million outpatient appointments were attended by patients in England.52 Since travel accounts for 10% of NHS carbon footprint, the widespread adoption of telemedicine services within the NHS could lead to huge emission reductions.26 The studies in this paper all focused on secondary or tertiary care; however telemedicine may also have environmental savings within general practice. In the year from November 2017 to October 2018, there were an estimated 308 million general practice appointments, 82% of which were FTF appointments.53
In the current COVID-19 pandemic, the use of telemedicine is proving indispensable to remotely assess patients, both in diagnosis of COVID-19 as well as ongoing management of chronic disease.54,55 This has been adopted across both primary and secondary care.56,57 This may accelerate the uptake of telemedicine globally, and increase acceptance of it among clinicians and patients alike.
Conclusion
The studies found in this review have unanimously reported that the use of telemedicine services leads to a reduction in the carbon footprint of healthcare. There was found to be a strong relationship between the carbon footprint saving and the average travel distance saving; highlighting that the majority of environmental reductions arise from reduction in travel to appointments. The consistency between studies and the scientific plausibility of the findings can give us confidence in the overall validity of our conclusions.
Our review suggests that telemedicine could play a valuable role in the transition to a net carbon-zero healthcare system. Further research is necessary to understand how to implement telemedicine within specific contexts of specialty and geographic region in order to maximise clinical and environmental benefits. The rebound effects of these telemedicine programmes, as well as the impact of double consulting, need to be further explored. The majority of the studies analysed did not include LCAs for the telemedicine equipment or for the modes of transport, therefore missing out a component of the carbon footprint. Future studies should aim to include these LCAs in order to produce more accurate estimates of carbon footprint which can be used to assess whether these programmes are carbon cost-effective. As for any new intervention in healthcare, multiple factors need to be considered including clinical and cost effectiveness, safety and equity, all in relation to a local context. It is into this mix that environmental considerations such as carbon footprint need to be understood.
Supplementary material
Additional supplementary material may be found in the online version of this article at www.rcpjournals.org/fhj:
S1 – Search terms and regression statistics.
Conflicts of interest
Dr James Smith reports personal fees from Trumpington Street Medical Practice, grants and personal fees from NHS England, personal fees from World Health Organization Europe, personal fees from Better Value Healthcare Ltd, personal fees from Cambridgeshire County Council, personal fees from University of Cambridge and its colleges, outside the submitted work; and he is married to a practicing GP in Cambridgeshire.
References
- 1.World Health Organization . Telemedicine: Opportunities and developments in Member States. Geneva: WHO, 2010. [Google Scholar]
- 2.Kruse CS, Krowski N, Rodriguez B, et al. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open 2017;7:e016242. 10.1136/bmjopen-2017-016242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emami E, Kadoch N, Homayounfar , et al. Patient satisfaction with e-oral health care in rural and remote settings: A systematic review protocol. Syst Rev 2017;6:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One 2019;14:e0221848.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mounessa JS, Chapman S, Braunberger T, et al. A systematic review of satisfaction with teledermatology. J Telemed Telecare 2018;24:263–70. [DOI] [PubMed] [Google Scholar]
- 6.Bashshur RL, Howell JD, Krupinski EA, et al. The empirical foundations of telemedicine interventions in primary care. Telemed J E Health 2016;22:342–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Le Goff-Pronost M, Mourgeon B, Blanchère JP, et al. Real-world clinical evaluation and costs of telemedicine for chronic wound management. Int J Technol Assess Health Care 2018;34:567–75. [DOI] [PubMed] [Google Scholar]
- 8.Orozco-Beltran D, Sánchez-Molla M, Sanchez JJ, Mira JJ. Telemedicine in primary care for patients with Chronic conditions: The valcrònic quasi-experimental study. J Med Internet Res 2017;19:e400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kroenke K, Krebs EE, Wu J, et al. Telecare collaborative management of chronic pain in primary care a randomized clinical trial. JAMA 2014;312:240–8. [DOI] [PubMed] [Google Scholar]
- 10.Beste LA, Glorioso TJ, Ho PM, et al. Telemedicine specialty support promotes hepatitis c treatment by primary care providers in the department of veterans affairs. Am J Med 2017;130:432–8. e3. [DOI] [PubMed] [Google Scholar]
- 11.Ulrich O, Marlene B, Silvan T. [Telemedicine and the ageing population]. Ther Umsch 2015;72:567–75. [DOI] [PubMed] [Google Scholar]
- 12.Waller M, Stotler C. Telemedicine: a primer. Curr Allergy Asthma Rep 2018;18:54. [DOI] [PubMed] [Google Scholar]
- 13.Guaiana G, Mastrangelo J, Hendrikx S, Barbui C. A systematic review of the use of telepsychiatry in depression. Community Ment Health J 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang W, Cheng B, Zhu W, et al. Effect of telemedicine on quality of care in patients with coexisting hypertension and diabetes: a systematic review and meta-analysis. Telemed J E Health 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 15.Lazarus G, Permana AP, Nugroho SW, et al. Telestroke strategies to enhance acute stroke management in rural settings: A systematic review and meta-analysis. Brain Behav 2020;10:e01787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen L, Cheng L, Gao W, et al. Telemedicine in chronic wound management: Systematic review and meta-analysis. JMIR Mhealth Uhealth 2020;8:e15574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hammersley V, Donaghy E, Parker R, et al. Comparing the content and quality of video, telephone, and face-to-face consultations: A non-randomised, quasi-experimental, exploratory study in UK primary care. Br J Gen Pract 2019;69:e595–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ullah W, Pathan SK, Panchal A, et al. Cost-effectiveness and diagnostic accuracy of telemedicine in macular disease and diabetic retinopathy: A systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e20306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Y, Min J, Khuri J, et al. Effectiveness of mobile health interventions on diabetes and obesity treatment and management: Systematic review of systematic reviews. JMIR Mhealth Uhealth 2020;8:e15400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kessler EA, Sherman AK, Becker ML. Decreasing patient cost and travel time through pediatric rheumatology telemedicine visits. Pediatr Rheumatol Online J 2016;14:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Russo JE, McCool RR, Davies L. VA Telemedicine: An Analysis of Cost and Time Savings. Telemed J E Health 2016;22:209–15. [DOI] [PubMed] [Google Scholar]
- 22.Kahn EN, La Marca F, Mazzola CA. Neurosurgery and telemedicine in the united states: assessment of the risks and opportunities. World Neurosurg 2016;89:133–8. [DOI] [PubMed] [Google Scholar]
- 23.Ipsos MORI . Solving the environment is everyone's problem. Ipsos MORI, 2020. www.ipsos.com/ipsos-mori/en-uk/solving-environment-everyones-problem [Google Scholar]
- 24.World Health Organization . Climate change and health. WHO, 2018. www.who.int/news-room/fact-sheets/detail/climate-change-and-health [Accessed 16 April 2020].
- 25.Karliner J, Slotterback S, Boyd R, Ashby B, Steele K. Health care's climate footprint: how the health sector contributes to the global climate crisis and opportunities for action. Health Care Without Harm, 2019. [Google Scholar]
- 26.NHS . Delivering a ‘net zero’ National Health Service. NHS, 2020. www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf [Accessed 20 October 2020]. [Google Scholar]
- 27.Mayor S. NHS should bring in measures to reduce its carbon footprint, BMA says. BMJ 2008;336:740.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The Strategy Unit . The potential economic impact of virtual outpatient appointments in the west midlands: a scoping study. NHS Midlands and Lancashire Commissioning Support Unit, 2018. www.strategyunitwm.nhs.uk/sites/default/files/2018-11/180813_Economic%20Impact%20of%20OP%20Appointments%20for%20WM%20CCGs_FINAL.pdf [Accessed 21 October 2020].
- 29.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miah S, Dunford C, Edison M, et al. A prospective clinical, cost and environmental analysis of a clinician-led virtual urology clinic. Ann R Coll Surg Engl 2019;101:30–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Connor MJ, Miah S, Edison MA, et al. Clinical, fiscal and environmental benefits of a specialist-led virtual ureteric colic clinic: a prospective study. BJU Int 2019;124:1034–9. [DOI] [PubMed] [Google Scholar]
- 32.Connor A, Mortimer F, Higgins R. The follow-up of renal transplant recipients by telephone consultation: Three years experience from a single UK renal unit. Clin Med 2011;11:242–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robinson JD, Prochaska JD, Yngve DA. Pre-surgery evaluations by telephone decrease travel and cost for families of children with cerebral palsy. SAGE Open Med 2017;5:2050312117720046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holmner A, Ebi KL, Lazuardi L, Nilsson M. Carbon footprint of telemedicine solutions–unexplored opportunity for reducing carbon emissions in the health sector. PloS One 2014;9:e105040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ong D, Moors T, Sivaraman V. Complete life-cycle assessment of the energy/CO2 costs of videoconferencing vs face-to-face meetings. 2012 IEEE Online Conference on Green Communications (GreenCom) 2012:50–55. [Google Scholar]
- 36.Leduc G, Mongelli I, Uihlein A, Nemry F. How can our cars become less polluting? An assessment of the environmental improvement potential of cars. Transport Policy 2010;17:409–19. [Google Scholar]
- 37.Masino C, Rubinstein E, Lem L, Purdy B, Rossos PG. The impact of telemedicine on greenhouse gas emissions at an academic health science center in Canada. Telemed J E Health 2010;16:973–6. [DOI] [PubMed] [Google Scholar]
- 38.Whetten J, Montoya J, Yonas H. ACCESS to better health and clear skies: telemedicine and greenhouse gas reduction. Telemed J E Health 2019;25:960–5. [DOI] [PubMed] [Google Scholar]
- 39.Dullet NW, Geraghty EM, Kaufman T, et al. Impact of a university-based outpatient telemedicine program on time savings, travel costs, and environmental pollutants. Value Health 2017;20:542–6. [DOI] [PubMed] [Google Scholar]
- 40.Oliveira TC, Barlow J, Gonçalves L, Bayer S. Teleconsultations reduce greenhouse gas emissions. J Health Serv Res Policy 2013;18:209–14. [DOI] [PubMed] [Google Scholar]
- 41.Paquette S, Lin JC. Outpatient telemedicine program in vascular surgery reduces patient travel time, cost, and environmental pollutant emissions. Ann Vasc Surg 2019;59167–72. [DOI] [PubMed] [Google Scholar]
- 42.Wootton R, Tait A, Croft A. Environmental aspects of health care in the Grampian NHS region and the place of telehealth. J Telemed Telecare 2010;16:215–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dorrian C, Ferguson J, Ah-See K, et al. Head and neck cancer assessment by flexible endoscopy and telemedicine. J Telemed Telecare 2009;15:118–21. [DOI] [PubMed] [Google Scholar]
- 44.Beswick DM, Vashi A, Song Y, et al. Consultation via telemedicine and access to operative care for patients with head and neck cancer in a Veterans Health Administration population. Head and Neck 2016;38:925–9. [DOI] [PubMed] [Google Scholar]
- 45.Vidal-Alaball J, Franch-Parella J, Seguí FL, Cuyas FG, Pena JM. Impact of a telemedicine program on the reduction in the emission of atmospheric pollutants and journeys by road. Int J Environ Res Public Health 2019;16:4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Statista . Number of mobile phone users worldwide 2015 to 2020. Statista, 2016. www.statista.com/statistics/274774/forecast-of-mobile-phone-users-worldwide [Accessed 13 May 2020]. [Google Scholar]
- 47.Capampangan DJ, Wellik KE, Bobrow BJ, et al. Telemedicine versus telephone for remote emergency stroke consultations: A critically appraised topic. Neurologist 2009;15:163–6. [DOI] [PubMed] [Google Scholar]
- 48.Poon WS, Leung CHS, Lam MK, et al. The comparative impact of video consultation on neurosurgical health services. Int J Med Inform 2001;62:175–80. [DOI] [PubMed] [Google Scholar]
- 49.Bolle SR, Larsen F, Hagen O, Gilbert M. Video conferencing versus telephone calls for team work across hospitals: A qualitative study on simulated emergencies. BMC Emerg Med 2009;9:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seuren LM, Wherton J, Greenhalgh T, et al. Physical examinations via video for patients with heart failure: qualitative study using conversation analysis. J Med Internet Res 2020;22:e16694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roberts A, Blunt I, Bardsley M. Focus on: distance from home to emergency care. Nuffield Trust, The Health Foundation, 2014. [Google Scholar]
- 52.NHS Digital . Hospital Outpatient Activity, 2016-17. NHS, 2017. https://digital.nhs.uk/data-and-information/publications/statistical/hospital-outpatient-activity/hospital-outpatient-activity-2016-17 [Accessed 02 April 2020]. [Google Scholar]
- 53.NHS Digital . Appointments in General Practice, October 2018. NHS, 2018.. https://digital.nhs.uk/data-and-information/publications/statistical/appointments-in-general-practice/oct-2018 [Accessed 03 April 2020]. [Google Scholar]
- 54.Portnoy J, Waller M, Elliott T. Telemedicine in the era of COVID-19. J Allergy Clin Immunol Pract 2020;8:1489–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill 2020;6:e18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Greenhalgh T, Koh GCH, Car J. Covid-19: a remote assessment in primary care. BMJ 2020;368:m1182. [DOI] [PubMed] [Google Scholar]
- 57.Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020;7:e17–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


