Fig. 1. Metabolism and current delivery challenges.
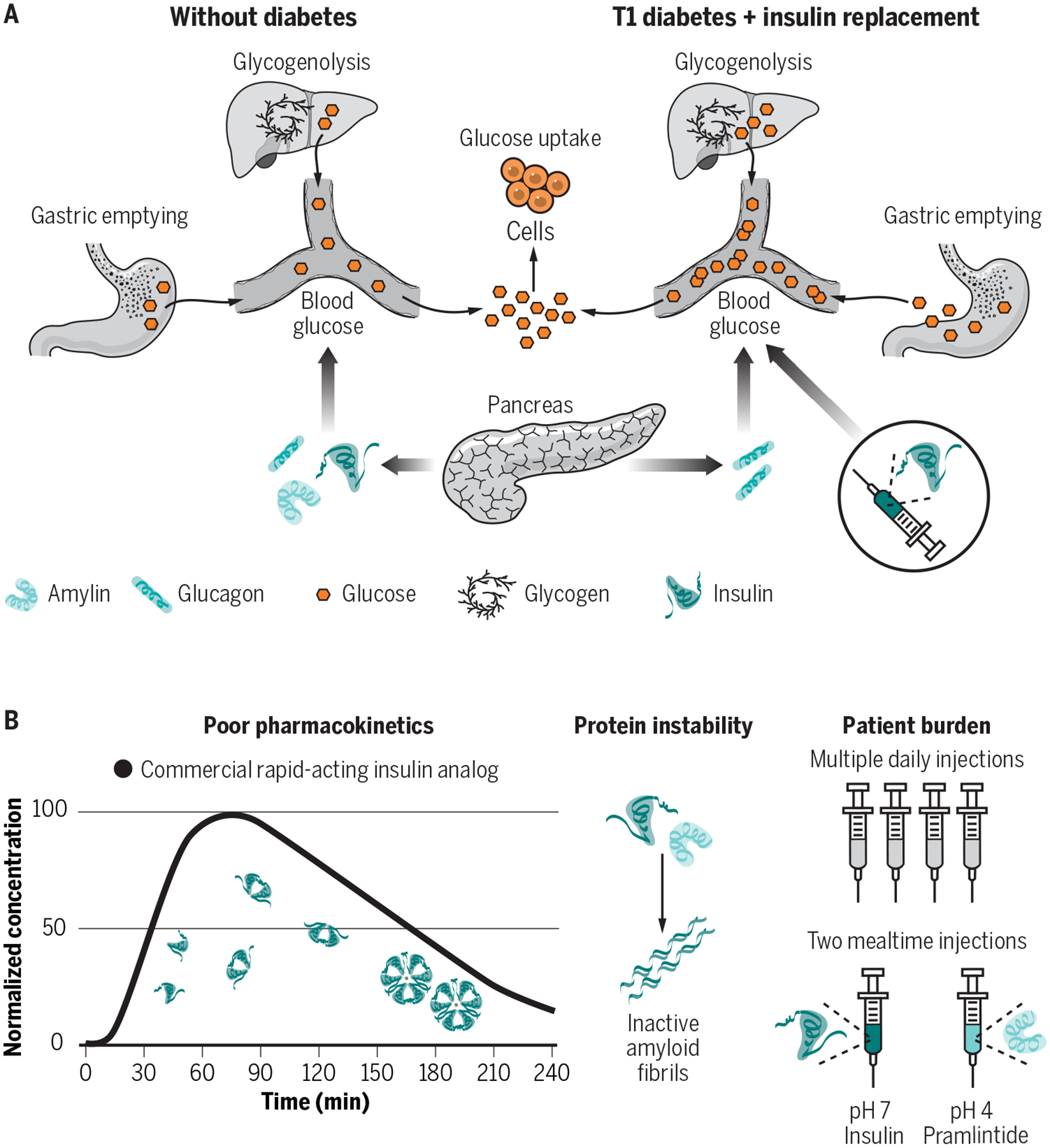
(A) In patients without diabetes, insulin, amylin and glucagon are secreted from the endocrine pancreas and work in tandem to maintain glucose homeostasis. Insulin and amylin work synergistically, where insulin promotes glucose uptake by cells and amylin slows gastric emptying and increases satiety. Glucagon, responsible for promoting glucose mobilization through glycogenolysis, is suppressed at mealtimes through paracrine signaling. (B) In patients with type 1 diabetes, subcutaneous delivery of insulin analogues (e.g., lispro, aspart, glulisine) can restore glucose uptake at mealtimes, but in the absence of replacement of amylin or its analogues (e.g., pramlintide) the effects of slowed gastric emptying and post-prandial glucagon suppression are lost – exacerbating prandial glucose excursions. (C) Therapies to deliver insulin, amylin analogues (pramlintide) and glucagon exist, but ideal use is highly burdensome, and the high costs preclude their use for many patients. Current drug delivery challenges include protein instability, burdensome treatment administration, and pharmacokinetics that do not sufficiently mimic endogenous hormone secretion to allow for optimal glucose control.
