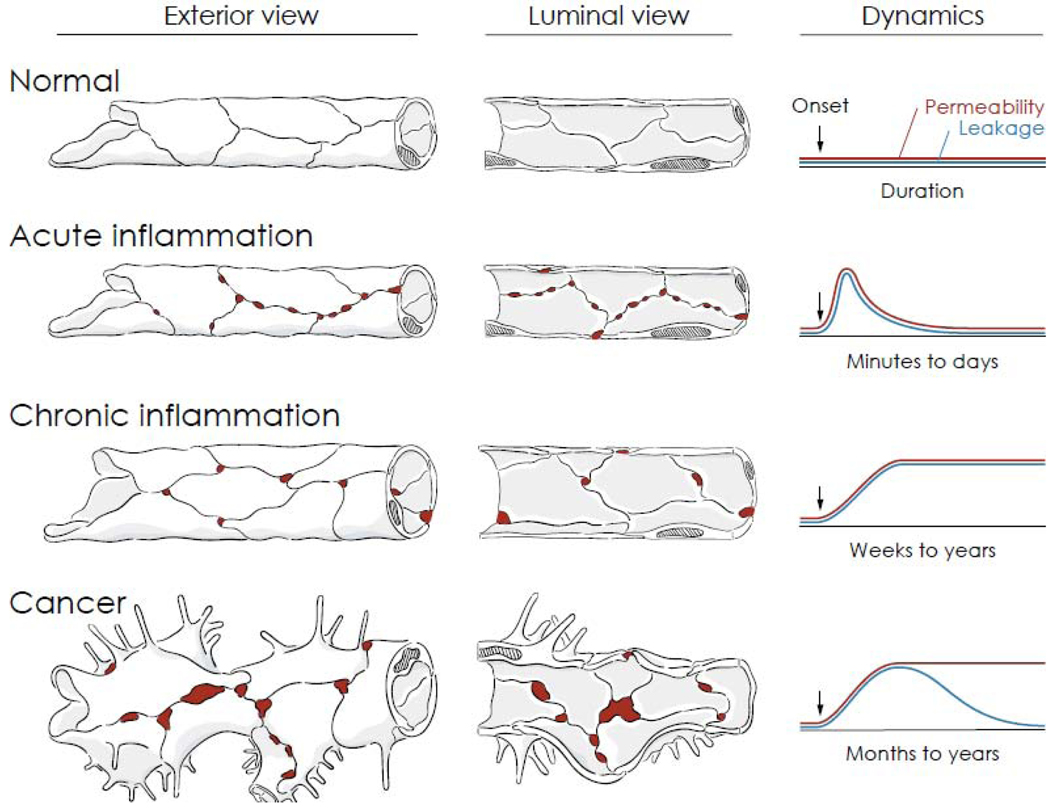
Figure 1. Vascular permeability and leakage in health and disease.
Comparison of exterior and luminal views of blood vessels of the microcirculation and corresponding dynamics of permeability and leakage over time under normal conditions, inflammation, and cancer. Durations are approximate values reflecting the vasculature of the entire organ rather than individual vessels or gaps. In normal blood vessels, junctions between endothelial cells form a uniform barrier that restricts extravasation of plasma. Gaps are not present between endothelial cells, and permeability and leakage are stable and low. In acute inflammation, leakage occurs as permeability increases rapidly through formation of focal endothelial gaps (red) in postcapillary venules. The gaps are transient, and vessels return to normal after the inflammatory stimulus ends or is inactivated. In chronic inflammation, vessels undergo structural remodeling, reflected by enlargement, proliferation (angiogenesis), increased mediator sensitivity, and sustained gap formation and leakage. The vascular changes do not resolve spontaneously but can be reversed by treatment of the chronic condition. In cancer, blood vessels that supply growing tumors undergo distinctive changes promoted by the abnormal tumor microenvironment, including sprouting angiogenesis, abnormal growth and gene expression, and defective endothelial junctions that result in leakage of plasma and even erythrocytes in some tumors. Increased endothelial permeability is sustained, but leakage decreases as interstitial pressure rises because of impaired lymphatic drainage.