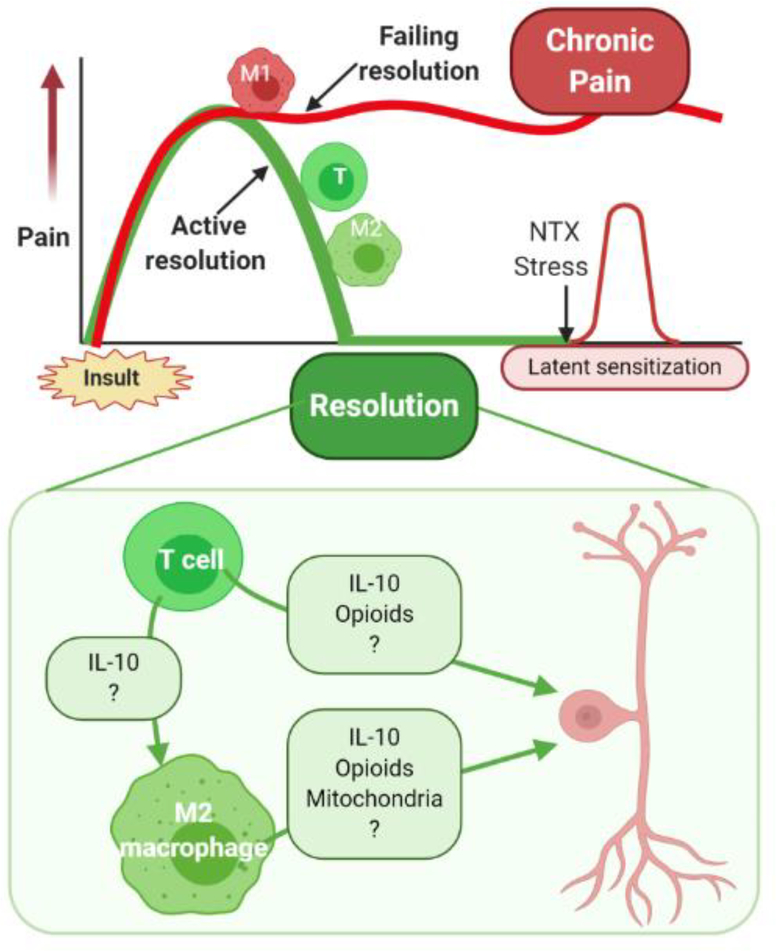
Figure 1, Key Figure: Contribution of T cells and macrophages to the resolution of pain.
Top Panel: Pain induced by transient insults such as tissue damage, inflammation, or drug treatment, does not resolve spontaneously once the driver is gone. Resolution of pain is an active regulatory process that requires the activity of T cells (T) and wound healing M2 macrophages (M2). When this resolution fails, M1 macrophages remain active and promote chronic pain. The apparent resolution of pain is the result of a novel homeostatic balance that requires active suppression, a situation known as latent sensitization.
Bottom Panel: Potential pathways contributing to T cell-mediated suppression or resolution of pain. CD4+ or CD8+ T cells suppress pain or promote the resolution of pain after recovery from inflammation, surgery or completion of chemotherapy via multiple pathways. T cells can produce the anti-inflammatory cytokine IL10 and promote the differentiation of M1 pro-inflammatory macrophages into M2 wound healing macrophages. Both T cells and M2 macrophages can release IL10 and opioid peptides that can signal to sensitized pain sensing neurons in the peripheral and central nervous system to reverse or control sensitization and resolve pain. In addition, M2 macrophages can transfer mitochondria to sensory neurons in dorsal root ganglia thereby contributing to resolution of pain. T cells and macrophages likely produce additional currently unknown factors (?) that contribute to pain resolution.