Abstract
Purpose
The role of hypoalbuminemia and raised C-reactive protein (CRP) levels in predicting critical prognosis has been described extensively in adult literature. However, there are limited studies in pediatrics, particularly neonates. The CRP/albumin (CRP/ALB) ratio is often associated with higher mortality, organ failure and prolonged hospital stay. We hypothesized that the serum CRP/ALB ratio has a prognostic value in predicting surgery and mortality in neonates with necrotizing enterocolitis (NEC).
Methods
Retrospective review of all neonates with clinical and radiological evidence of non-perforated NEC that were treated in a tertiary-level referral hospital between 2009 and 2018. General patient demographics, laboratory parameters and outcomes were recorded. Receiver operating characteristics analysis was performed to evaluated optimal cut-offs and area under the curve (AUC) with 95% confidence intervals (CI).
Results
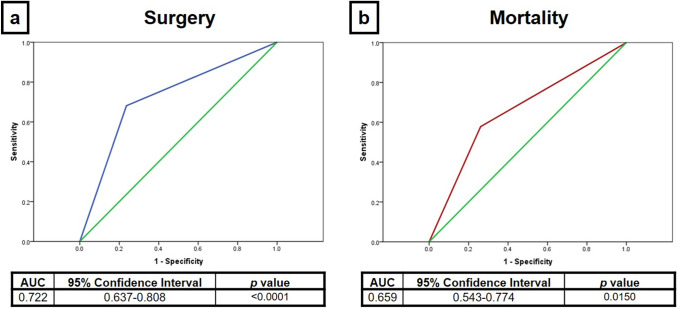
A total of 191 neonates were identified. Of these, 103 (53.9%) were born at ≤ 28 weeks of gestation and 101 (52.9%) had a birth weight of ≤ 1000 g. Eighty-four (44.0%) patients underwent surgical intervention for NEC. The overall survival rate was 161/191 (84.3%). A CRP/ALB ratio of ≥ 3 on day 2 of NEC diagnosis was associated with a statistically significant higher likelihood for surgery [AUC 0.71 (95% CI 0.63–0.79); p < 0.0001] and mortality [AUC 0.66 (95% CI 0.54–0.77); p = 0.0150], respectively.
Conclusions
A CRP/ALB ratio of ≥ 3 on day 2 is indicative of a critical pathway in neonates with radiologically confirmed, non-perforated NEC. This could be used as an additional criterion to guide parental counselling in NEC for surgical intervention and mortality.
Keywords: Necrotizing enterocolitis, C-reactive protein, Albumin, Surgery, Mortality, Outcomes
Introduction
Necrotizing enterocolitis (NEC) is one of the most common and critical gastrointestinal emergencies in neonates, which predominately affects premature and low birth weight infants in the first weeks of life. Surgical NEC is known to be associated with a significantly higher morbidity and mortality [1, 2]. However, the optimal timing for surgical intervention in neonates with NEC is not yet established [3, 4]. It has recently been shown that the largest proportion of perioperative deaths in pediatric surgery is secondary to NEC, with a 30-day perioperative mortality of up to 19% [5]. Hence, there is a need to identify validated early predictors for surgical intervention and mortality in neonates with NEC. Early predictors for surgery in neonates with NEC would optimize referral and treatment pathways, and potentially lead to improved outcomes [6]. Improving triage of neonates with NEC in non-surgical neonatal intensive care units in turn may lead to earlier referral, transfer and surgery. Ideally, a prognostic tool may predict surgical intervention in neonates with NEC as well as indicate the potential risk of death. This would also change parental counselling early in the disease process, thus enabling conversations to be tailored to each patient when discussing the probability of surgery and death in NEC cases [7].
The role of reduced serum albumin (ALB) and raised C-reactive protein (CRP) levels in predicting a critical prognosis has been described extensively in adult literature but is very limited in pediatrics. Research in adults has revealed that the CRP/ALB ratio is associated with higher mortality, organ failure and prolonged hospital stay in seriously ill or septic patients on acute medical wards and intensive care units, respectively [8, 9]. More recently, it has been demonstrated that a high CRP/ALB ratio is indicative of worse outcome (i.e. organ failure and/or death) in critically ill children on a pediatric intensive care unit [10]. The aim of this study was to investigate if the serum CRP/ALB ratio has a prognostic value in predicting surgical intervention and mortality in neonates with NEC.
Materials and methods
Study population and design
A retrospective cohort study of all neonates diagnosed with radiologically confirmed, non-perforated NEC that were consecutively admitted to the specialized neonatal intensive care unit at the Royal London Hospital (i.e. large, tertiary-level referral hospital) from 1 January 2009 to 31 December 2018 was performed. Details of each patient were identified using the BadgerNet platform (Clevermed, Edinburgh, United Kingdom)—a national electronic neonatal database. General patient demographics were collected on gender, pregnancy, gestational age and birth weight. Clinical presentation and examination findings were correlated with abdominal radiographs to ensure the patient met the inclusion criteria. Inclusion criteria were radiological evidence of NEC (i.e. pneumatosis intestinalis) and presence of one or more clinical findings (i.e. abdominal distension, bilious/bloody aspirates, blood per rectum, abdominal tenderness, abdominal wall erythema/discoloration or abdominal mass). The first day of NEC diagnosis was classified as day 1 of the disease process, and daily measured serum CRP and ALB levels were extracted from the individual electronical or paper medical records. When several blood samples were taken per day, the time of the first set of bloods was used and results from the next nearest tests done at 24 h, 48 h, etc. were recorded. If applicable, date of surgery and mortality data were noted for each patient. Indications for surgery were subsequent evidence of perforation, increasing abdominal distension, erythema, discoloration and tenderness despite maximal medical management and increasing ventilatory/inotropic support. Neonates presenting with radiologically confirmed perforated NEC were excluded from the study, which was formally registered with the clinical effectiveness unit at the Barts Health NHS Trust. As the study was retrospective in nature and therefore did not change the clinical management of patients involved, it was exempt from full IRB review but followed the principles expressed in the Declaration of Helsinki.
Statistical analysis
Data was collated into an electronic spreadsheet and statistical analysis was performed using PASW Statistics 18.0 software application (SPSS Inc., Chicago, USA). Statistical differences between two cohorts of neonates with NEC (i.e. surgical intervention vs. conservative medical management) as well as outcome were analyzed using Chi-square or Fisher’s exact test, where appropriate. The serum CRP/ALB ratio on day 1, 2 and 3 of NEC diagnosis was determined in each patient. Bivariate and receiver operating characteristics (ROC) analysis was used to assess optimal cut-offs for the CRP/ALB ratio with sensitivity/specificity and to calculate the area under the ROC curves (AUC) with 95% confidence intervals (CI), respectively. A p value of < 0.05 was considered statistically significant.
Results
General patients’ demographics
A total of 191 consecutive neonates with radiologically confirmed, non-perforated NEC were identified during the study period. Of these, 106 (55.5%) were male and 85 (44.5%) were female. Median gestational age was 28.2 weeks (range 23.1–39.0) with a median birth weight of 1113 g (range 490–4140). One hundred and three (53.9%) were born at ≤ 28 weeks of gestation and 101 (52.9%) had a birth weight of ≤ 1000 g. In total, 84 (44.0%) patients eventually underwent surgical intervention for NEC. Indications for surgery were increasing abdominal distension, erythema or discoloration with tenderness despite maximal medical management and increasing ventilatory and/or inotropic support. Six patients had surgical intervention for a subsequent bowel perforation on a median of 3.5 days (range 1–10) after NEC diagnosis. Overall, for all neonates who underwent surgery, this occurred on a median of 3 days (range 1–23) of medical treatment. Except for gender and gestational age, there were no statistical difference between patients that had surgical intervention and those that did not (Table 1). The overall survival rate was 161/191 (84.3%). Of the 30 cases that died, 23 (76.7%) had surgery, compared to 61/161 (37.9%) of the surviving patients (p < 0.0001). Neonates who died were significantly more likely to be very premature (i.e. ≤ 28 weeks) and extremely low birth weight (i.e. ≤ 1000 g).
Table 1.
General patients’ demographics and outcomes in 191 neonates with radiologically confirmed, non-perforated NEC
| Patient characteristics | Surgery | Medical management | p = | Survived | Died | p = | |
|---|---|---|---|---|---|---|---|
| (n = 84) | (n = 107) | (n = 161) | (n = 30) | ||||
| Gender | 0.014 | 0.289 | |||||
| Male | 55 (65.5%) | 51 (47.7%) | 92 (57.1%) | 14 (46.7%) | |||
| Female | 29 (34.5%) | 56 (52.3%) | 69 (42.9%) | 16 (53.3%) | |||
| Pregnancy | 0.251 | 0.710 | |||||
| Single | 60 (71.4%) | 86 (80.3%) | 123 (76.4%) | 23 (76.7%) | |||
| Twin | 20 (23.8%) | 19 (17.8%) | 32 (19.9%) | 7 (23.3%) | |||
| Triplet | 4 (4.8%) | 2 (1.9%) | 6 (3.7%) | – | |||
| Gestational age | 0.003 | 0.010 | |||||
| Term | 3 (3.6%) | 2 (1.9%) | 4 (2.5%) | 1 (3.3%) | |||
| Preterm (≤ 37 weeks) | 25 (29.8%) | 58 (54.2%) | 77 (47.8%) | 6 (20.0%) | |||
| Very preterm (≤ 28 weeks) | 56 (66.6%) | 47 (43.9%) | 80 (49.7%) | 23 (76.7%) | |||
| Birth weight | 0.112 | 0.003 | |||||
| Normal | 5 (5.9%) | 6 (5.6%) | 10 (6.2%) | 1 (3.3%) | |||
| Low birth weight (≤ 2500 g) | 14 (16.7%) | 22 (20.6%) | 33 (20.5%) | 3 (10.0%) | |||
| Very low birth weight (≤ 1500 g) | 13 (15.5%) | 30 (28.0%) | 42 (26.1%) | 1 (3.3%) | |||
| Extremely low birth weight (≤ 1000 g) | 52 (61.9%) | 49 (45.8%) | 76 (47.2%) | 25 (83.4%) | |||
Predictive value of CRP/ALB ratio for surgery and mortality
Bivariate analysis comparing sensitivity and specificity of different CRP/ALB ratios in predicting surgery and mortality was calculated (Table 2). A serum CRP/ALB ratio of ≥ 2 on day 1 of NEC diagnosis has a reasonably good predictive value for surgical intervention with a sensitivity of 43.9% (95% CI 32.6–55.9) and a specificity of 76.1% (95% CI 66.4–83.6). Sensitivity levels and AUCs increase as medical management of NEC continues from day 1 to 3. The CRP/ALB ratio of ≥ 3 on day 3 had the best predictive ability at sensitivity of 76.4% (95% CI 63.7–85.6) and specificity of 71.9% (95% CI 62.2–79.9) in predicting surgery for NEC with a AUC of 0.72 [(95% CI 0.64–0.81); p < 0.0001] (Fig. 1a).
Table 2.
Sensitivity, specificity and AUC of CRP/ALB ratios in predicting surgery and mortality in neonates with radiologically confirmed, non-perforated NEC
| Outcomes | CRP/ALB ratio | Sensitivity (95% CI) | Specificity (95% CI) | AUC (95% CI) | p = |
|---|---|---|---|---|---|
| Surgery | Day 1 (n = 158) | ||||
| CRP/ALB ratio ≥ 2 | 43.9 (32.6–55.9) | 76.1 (66.4–83.6) | 0.60 (0.51–0.69) | 0.032 | |
| CRP/ALB ratio ≥ 2.5 | 43.9 (32.6–55.9) | 76.1 (66.4–83.6) | 0.60 (0.51–0.69) | 0.032 | |
| CRP/ALB ratio ≥ 3 | 39.4 (28.5–51.5) | 78.3 (68.8–85.5) | 0.59 (0.50–0.68) | 0.059 | |
| Day 2 (n = 170) | |||||
| CRP/ALB ratio ≥ 2 | 78.4 (67.7–86.2) | 56.3 (46.3–65.7) | 0.67 (0.59–0.76) | < 0.001 | |
| CRP/ALB ratio ≥ 2.5 | 75.7 (53.6–72.5) | 63.5 (53.6–72.5) | 0.70 (0.62–0.78) | < 0.001 | |
| CRP/ALB ratio ≥ 3 | 70.3 (59.1–79.5) | 68.1 (58.0–76.8) | 0.71 (0.63–0.79) | < 0.001 | |
| Day 3 (n = 146) | |||||
| CRP/ALB ratio ≥ 2 | 81.2 (69.7–89.8) | 50.6 (40.5–60.6) | 0.66 (0.57–0.75) | 0.001 | |
| CRP/ALB ratio ≥ 2.5 | 80.0 (67.6–88.5) | 60.4 (50.2–69.9) | 0.70 (0.62–0.79) | < 0.001 | |
| CRP/ALB ratio ≥ 3 | 76.4 (63.7–85.6) | 71.9 (62.2–79.9) | 0.72 (0.64–0.81) | < 0.001 | |
| Mortality | Day 1 (n = 158) | ||||
| CRP/ALB ratio ≥ 2 | 31.8 (16.4–52.7) | 67.7 (59.4–74.9) | 0.50 (0.37–0.63) | 0.968 | |
| CRP/ALB ratio ≥ 2.5 | 31.8 (16.4–52.7) | 67.7 (59.4–74.9) | 0.50 (0.37–0.63) | 0.968 | |
| CRP/ALB ratio ≥ 3 | 31.8 (16.4–52-7) | 57.8 (49.7–65.5) | 0.52 (0.38–0.65) | 0.813 | |
| Day 2 (n = 170) | |||||
| CRP/ALB ratio ≥ 2 | 78.3 (58.1–90.3) | 44.2 (36.4–52.3) | 0.61 (0.50–0.73) | 0.083 | |
| CRP/ALB ratio ≥ 2.5 | 73.9 (53.5–87.5) | 49.7 (41.7–57.7) | 0.62 (0.50–0.74) | 0.069 | |
| CRP/ALB ratio ≥ 3 | 73.9 (53.3–87.5) | 71.3 (63.2–78.3) | 0.66 (0.54–0.77) | 0.015 | |
| Day3 (n = 146) | |||||
| CRP/ALB ratio ≥ 2 | 76.5 (52.7–90.5) | 40.3 (32.2–48.9) | 0.58 (0.45–0.72) | 0.262 | |
| CRP/ALB ratio ≥ 2.5 | 76.5 (52.7–90.5) | 48.1 (39.6–56.6) | 0.62 (0.49–0.76) | 0.101 | |
| CRP/ALB ratio ≥ 3 | 70.6 (46.9–86.7) | 54.3 (45.7–62.6) | 0.62 (0.49–0.76) | 0.096 | |
Fig. 1.
Predictive ability of CRP/ALB ratio of ≥ 3 ratio for (a) surgery on day 3 and (b) mortality on day 2 in neonates with radiologically confirmed, non-perforated NEC (The green line is a reference line when AUC = 0.5, which would suggest the predictive value is 50%. By comparison, the blue (a) and red (b) lines represent the AUCs for predicting surgery and mortality, respectively)
A serum CRP/ALB ratio of ≥ 3 on day 2 of NEC diagnosis had the highest predictive value for mortality with a sensitivity of 73.9% (95% CI 53.3–87.5), specificity of 71.3% (95% CI 63.2–78.3) and AUC of 0.66 (0.54–0.77); p = 0.0150 (Fig. 1b).
Discussion
In this study, neonates with radiologically confirmed, non-perforated NEC who underwent surgery reflected previously well-established findings in NEC research showing correlation between surgery, male gender and gestational age ≤ 28 weeks. Within this group of patients, we have demonstrated that a CRP/ALB ratio of ≥ 2 early in the disease process (i.e. day 1–3) correlates with surgical intervention.
CRP is an acute phase protein, which will be raised in conditions that provoke a systemic inflammatory response syndrome (SIRS). This has been noted clinically and CRP is often part of the daily tests to monitor neonates for NEC disease progression [11]. A raised CRP in clinically deteriorating NEC cases has been demonstrated [12, 13]. Furthermore, a low serum ALB level has been associated with poor clinical outcomes in critically ill children [14, 15]. Hypoalbuminemia in NEC has recently been identified as a novel marker for disease progression [16].
The significance of the CRP/ALB ratio has previously been reported in a variety of adult conditions [8, 9, 17]. It has been shown that a higher CRP/ALB ratio is an independent prognostic factor in conditions as diverse as chronic kidney disease [18], lung cancer [19, 20] and severe sepsis [9]. The CRP/ALB ratio has also been identified to be an independent predictor of mortality in critically ill or septic adults [21, 22]. There are some comparable research findings reported in pediatrics. In a prospective observational study of 100 critically ill children on a pediatric intensive care unit (PICU), a high CRP/ALB ratio predicted an unfavorable prognosis with adverse outcome (i.e. organ failure and/or death) [10]. Another study looking at 178 pediatric patients used the CRP/ALB ratio to risk stratify children admitted to a PICU [23]. The CRP/ALB ratio within 24 h of PICU admission was utilized. Patients requiring either ventilator or inotropic support had a significantly higher median CRP/ALB ratio. In addition, the CRP/ALB ratio was significantly higher in non-survivors compared with survivors (18.6 vs. 4.65; p < 0.0001), further indicating that the CRP/ALB ratio at PICU admission is an independent predictor of mortality.
To date, there has only been one single-center study that analyzed the CRP/ALB ratio in neonates. Yang et al. [24] investigated the use of the CRP/ALB ratio in premature infants with perinatal infection. They demonstrated that the ratio is useful for detection of early infection and suggested this as a valuable tool to rationalize the use of antibiotics. A systemic infection in a neonate will trigger a systemic inflammatory response, which is reflected in high serum CRP and low serum albumin levels, and this accounts for these findings. Similarly, although NEC is a disease that originates in the gastrointestinal tract, it has the ability to impact the whole neonate, potentially leading to SIRS. As bowel is progressively compromised during the evolving disease process, the impact of SIRS is reflected in the neonates’ changing physiology and subsequent laboratory serum findings.
Our study has a number of limitations. It was retrospective in nature with a limited number of patients and thus dependent on individually written chart records. Therefore, not reported confounding factors could not necessarily be ruled out, which may have caused a potential result bias. Within single-center studies, there is an overall bias towards how NEC assessment and treatment is carried out. In our center, there are several consultant pediatric surgeons, all operating on and managing neonates with NEC. As a result, the decision-making process is different for each surgeon. In particular, the timing of surgery in a neonate who is medically managed for NEC is very subjective, and hence variable. For example, there are some instances when this variability is uniformly minimized, e.g. in neonates with evidence of bowel perforation.
Conclusions
To our knowledge, this is the first study analyzing the CRP/ALB ratio specifically in NEC. Our observations showed that a CRP/ALB ratio of ≥ 2 on day 1 has already a reasonably good predictive ability for surgical intervention in neonates with radiologically confirmed, non-perforated NEC. However, a CRP/ALB ratio of ≥ 3 on day 3 had the highest predictive value for surgery in our cohort. This finding may be utilized to triage neonates for transfer to specialist neonatal surgical centers, which would optimize surgical cot utilization. Our study also demonstrated the predicative ability of the CRP/ALB ratio of ≥ 3 on day 2 in view of mortality. This could be used as an additional criterion to guide parental counselling for NEC. Nevertheless, we need to aim for a more standardized decision-making and surgery in NEC. Therefore, we propose a prospective, multicenter study that would enable validation of our results in a larger cohort of neonates with NEC. This would potentially provide a simple, easily accessible and inexpensive tool to provide prediction of surgery and mortality in NEC.
Author contributions
Study conception and design: SPS. Data acquisition: AA, SPS. Analysis and data interpretation: AA, RAZ, FF, SPS. Drafting of the manuscript: AA, RAZ, FF, SPS. Critical revision: AA, RAZ, FF, SPS.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors did not receive any financial support for the submitted work.
Declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Florian Friedmacher and Shazia P. Sharif shared last authorship.
References
- 1.Lang J, Hickey L, King S, Curley A. OC58 morbidity and mortality of medical and surgical necrotising enterocolitis. Arch Dis Child. 2019;104:A24. [Google Scholar]
- 2.Jones IH, Hall NJ. Contemporary outcomes for infants with necrotizing enterocolitis—a systematic review. J Pediatr. 2020;220:86–92.e3. doi: 10.1016/j.jpeds.2019.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Robinson JR, Rellinger EJ, Hatch LD, et al. Surgical necrotizing enterocolitis. Semin Perinatol. 2017;41:70–79. doi: 10.1053/j.semperi.2016.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munaco AJ, Veenstra MA, Brownie E, Danielson LA, Nagappala KB, Klein MD. Timing of optimal surgical intervention for neonates with necrotizing enterocolitis. Am Surg. 2015;81:438–443. doi: 10.1177/000313481508100521. [DOI] [PubMed] [Google Scholar]
- 5.Bonasso PC, Dassinger MS, Ryan ML, Gowen MS, Burford JM, Smith SD. 24-hour and 30-day perioperative mortality in pediatric surgery. J Pediatr Surg. 2019;54:628–630. doi: 10.1016/j.jpedsurg.2018.06.026. [DOI] [PubMed] [Google Scholar]
- 6.Gregory KE. Clinical predictors of necrotizing enterocolitis in premature infants. Nurs Res. 2008;57:260–270. doi: 10.1097/01.NNR.0000313488.72035.a9. [DOI] [PubMed] [Google Scholar]
- 7.Allin B, Long AM, Gupta A, Knight M, Lakhoo K, British Association of Paediatric Surgeons Congenital Anomalies Surveillance System Necrotising Enterocolitis Collaboration A UK wide cohort study describing management and outcomes for infants with surgical necrotising enterocolitis. Sci Rep. 2017;7:41149. doi: 10.1038/srep41149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fairclough E, Cairns E, Hamilton J, Kelly C. Evaluation of a modified early warning system for acute medical admissions and comparison with C-reactive protein/albumin ratio as a predictor of patient outcome. Clin Med (Lond) 2009;9:30–33. doi: 10.7861/clinmedicine.9-1-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranzani OT, Zampieri FG, Forte DN, Azevedo LC, Park M. C-reactive protein/albumin ratio predicts 90-day mortality of septic patients. PLoS ONE. 2013;8:e59321. doi: 10.1371/journal.pone.0059321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhandarkar N, Save S, Bavdekar SB, Sisodia P, Desai S. Serum albumin and C-reactive protein as predictors of adverse outcomes in critically ill children: a prospective observational pilot study. Indian J Pediatr. 2019;86:758–759. doi: 10.1007/s12098-019-02934-3. [DOI] [PubMed] [Google Scholar]
- 11.Duci M, Fascetti-Leon F, Erculiani M, et al. Neonatal independent predictors of severe NEC. Pediatr Surg Int. 2018;34:663–669. doi: 10.1007/s00383-018-4261-1. [DOI] [PubMed] [Google Scholar]
- 12.Cetinkaya M, Ozkan H, Köksal N, Akaci O, Ozgür T. Comparison of the efficacy of serum amyloid A, C-reactive protein, and procalcitonin in the diagnosis and follow-up of necrotizing enterocolitis in premature infants. J Pediatr Surg. 2011;46:1482–1489. doi: 10.1016/j.jpedsurg.2011.03.069. [DOI] [PubMed] [Google Scholar]
- 13.Srinivasjois R, Nathan E, Doherty D, Patole S. Prediction of progression of definite necrotising enterocolitis to need for surgery or death in preterm neonates. J Matern Fetal Neonatal Med. 2010;23:695–700. doi: 10.3109/14767050903551467. [DOI] [PubMed] [Google Scholar]
- 14.Leite HP, da Silva AVR, de Iglesias SBO, Nogueira PCK. Serum albumin is an independent predictor of clinical outcomes in critically ill children. Pediatr Crit Care Med. 2016;17:e50–57. doi: 10.1097/PCC.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 15.Kumar S, Aroor S, Kini PG, Mundkur S, Moideen A. Hypoalbuminemia as a marker of adverse outcome in children admitted to pediatric intensive care unit. Indian J Child Health. 2018;5:6–10. doi: 10.32677/IJCH.2018.v05.i01.002. [DOI] [Google Scholar]
- 16.Yakut I, Tayman C, Oztekin O, Namuslu M, Karaca F, Kosus A. Ischemia-modified albumin may be a novel marker for the diagnosis and follow-up of necrotizing enterocolitis. J Clin Lab Anal. 2014;28:170–177. doi: 10.1002/jcla.21661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xie Q, Zhou Y, Xu Z, et al. The ratio of CRP to prealbumin levels predict mortality in patients with hospital-acquired acute kidney injury. BMC Nephrol. 2011;12:30. doi: 10.1186/1471-2369-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Menon V, Greene T, Wang X, et al. C-reactive protein and albumin as predictors of all-cause and cardiovascular mortality in chronic kidney disease. Kidney Int. 2005;68:766–772. doi: 10.1111/j.1523-1755.2005.00455.x. [DOI] [PubMed] [Google Scholar]
- 19.Zhou T, Zhan J, Hong S, et al. Ratio of C-reactive protein/albumin is an inflammatory prognostic score for predicting overall survival of patients with small-cell lung cancer. Sci Rep. 2015;5:10481. doi: 10.1038/srep10481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang F, Ying L, Jin J, et al. The C-reactive protein/albumin ratio predicts long-term outcomes of patients with operable non-small cell lung cancer. Oncotarget. 2017;8:8835–8842. doi: 10.18632/oncotarget.13053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim MH, Ahn JY, Song JE, et al. The C-reactive protein/albumin ratio as an independent predictor of mortality in patients with severe sepsis or septic shock treated with early goal-directed therapy. PLoS ONE. 2015;10(7):e0132109. doi: 10.1371/journal.pone.0132109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park JE, Chung KS, Song JH, et al. The C-reactive protein/albumin ratio as a predictor of mortality in critically ill patients. J Clin Med. 2018;7:E333. doi: 10.3390/jcm7100333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mohamed SA, ElHawary R. C-Reactive protein/albumin ratio as an independent predictor of mortality in critically ill pediatric patients. J Child Sci. 2020;10:e1–11. doi: 10.1055/s-0040-1701623. [DOI] [Google Scholar]
- 24.Yang C, Yang Y, Li B, Xu P, Shen Q, Yang Q. The diagnostic value of high-sensitivity C-reactive protein/albumin ratio in evaluating early-onset infection in premature. Chin Crit Care Med. 2016;28:173–177. doi: 10.3760/cma.j.issn.2095-4352.2016.02.017. [DOI] [PubMed] [Google Scholar]