Figure 2:
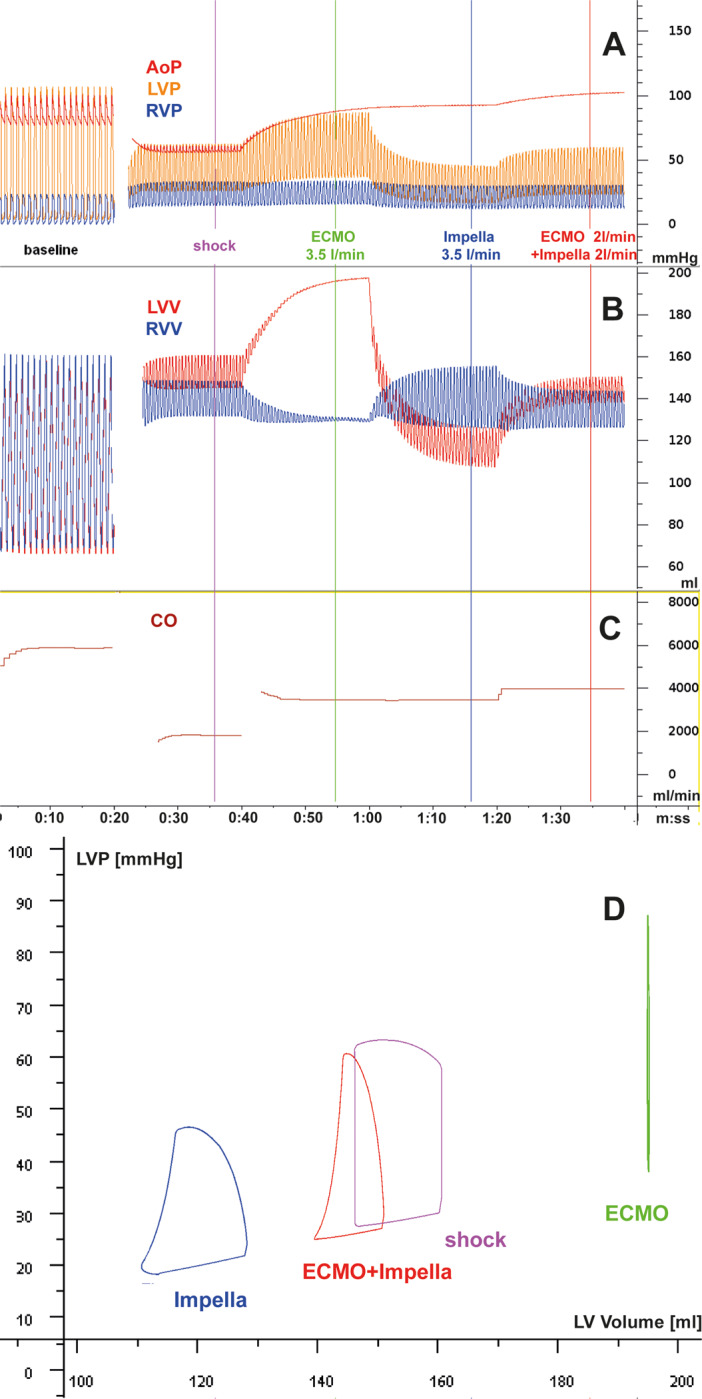
The differential haemodynamic effects of cardiogenic shock in acute myocardial infarction with mechanical support by ECMO, Impella, and their combination is modelled based on the Basel Virtual Patient, a multi-organ computational patient simulator at the University Hospital of Basel. Panels A–C shows parameters over time, and Panel D shows the left ventricular pressure/volume loops at the time points indicated by coloured bars in panels A–C, with violet: unsupported cardiogenic shock (CS); green: CS with ECMO support at 3.5 L/min; blue: CS with Impella support at 3.5 L/min; red: CS with ECMO at 2 L/min plus Impella at 2 L/min. Starting with a normal cardiac function at baseline (heart rate, 60/min), a myocardial infarction-triggered shock state is induced by partial loss of contractile left ventricular myocardium [reduced overall left ventricular (LV) systolic contractility], impaired LV diastolic function (delayed relaxation and increased stiffness), resulting in acute heart failure and triggering adrenergic activation with tachycardia (120/min), systemic and pulmonary vasoconstriction and venous pooling, while right ventricular systolic and diastolic function are not affected. AoP, aortic pressure; CO, combined cardiac output from heart and devices; LVP, left ventricular pressure; LVV, left ventricular volume; RVP, right ventricular pressure; RVV, right ventricular volume. (A–C) In the absence of RV failure, ECMO and Impella are similarly capable of delivering a cardiac output to the systemic circulation, but their effects on the left ventricle and the pulmonary circulation differ: in ECMO, residual forward flow through the pulmonary artery and the bronchial artery system and eventually some backflow from minor aortic regurgitation may lead to increased LV loading, increased LV pressures, and LV wall tension in ECMO. In Impella, the LV is consistently unloaded, wall tension is decreased and forward flow in the small circulation is maintained. When aortic pressure exceeds the maximum pressure that can be developed by the infarcted LV, the entire cardiac output is delivered by the respective device(s). Despite venous drainage in ECMO, high LV filling pressures in ECMO can occur and are compatible with the occurrence of pulmonary oedema in these patients, in contrast to the patients treated by ECpella or Impella alone. The combination of the two pumps, even with lower output from each individual device, reverses the LV loading observed by the ECMO. (D) ECMO support typically leads to a right shift of the PV loop (i.e. loading). Impella support consistently leads to a left shift of the PV loop indicating reduced diastolic and systolic wall tension and reduced myocardial oxygen consumption as predicted by pressure loop area. Source: University Hospital Basel, Basel, Switzerland
